Orthopedics focuses on the musculoskeletal system. Learn about the diagnosis, treatment, and rehabilitation of bone, joint, ligament, and muscle conditions.
Send us all your questions or requests, and our expert team will assist you.
The decision to proceed with joint replacement is never based on X rays alone; it is a clinical decision based on the patient’s symptoms and their impact on daily life. However, advanced imaging is crucial for confirming the diagnosis, assessing the severity of damage, and planning the surgical reconstruction.
The diagnostic process begins with a physical examination to rule out other sources of pain. For example, hip pain can sometimes originate from the spine. Once the joint is identified as the source, imaging provides the roadmap. Modern imaging goes beyond simple 2D pictures, utilizing 3D modeling to customize the surgery to the patient’s unique anatomy.
Laboratories studies are also employed to rule out infection or systemic inflammatory diseases. This comprehensive workup ensures that the surgery is safe and that the correct problem is being addressed.

The surgeon evaluates the joint’s range of motion, noting any stiffness or contractures (inability to straighten). They observe the patient’s gait, looking for limps or compensatory movements.
Palpation identifies specific areas of tenderness and checks for fluid (effusion) within the joint. Stability testing is crucial; for example, a knee replacement requires competent collateral ligaments to function. If ligaments are loose, a more constrained implant may be needed.

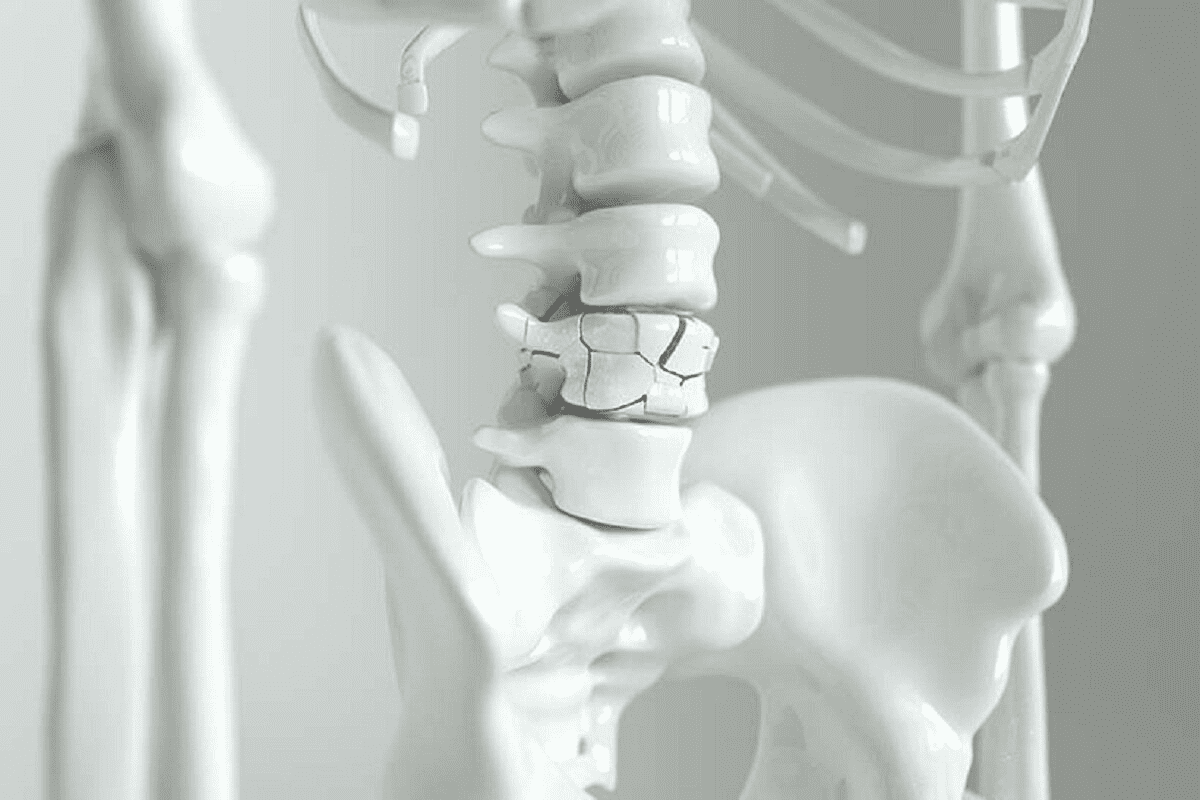
Weight bearing X rays are the gold standard for diagnosing lower limb arthritis. Standing up compresses the joint, revealing the true extent of cartilage loss. A “bone on bone” appearance confirms end stage disease.
Special views are taken to assess deformity. A long leg alignment film measures the mechanical axis of the leg, showing how much the arthritis has bowed the leg (varus) or knocked the knee (valgus). This guides the surgeon on how much correction is needed.
MRI is typically not needed to diagnose severe arthritis visible on X ray. However, it is invaluable for early stage disease or complex cases. It visualizes soft tissues like the rotator cuff in the shoulder or the ACL in the knee.
MRI is also used to evaluate the bone for avascular necrosis (AVN). It can detect the early death of bone cells before the bone collapses and becomes visible on an X ray. This allows for earlier intervention that might save the joint.

CT scans provide detailed 3D images of the bone. They are essential for robotic surgery planning. The scan data is uploaded to a computer, which generates a 3D model of the patient’s joint.
The surgeon uses this model to virtually perform the surgery before entering the operating room. They can size the implant, check the alignment, and plan the bone cuts with sub millimeter precision. CT is also critical for assessing bone loss in revision surgeries.
When the source of pain is unclear, a diagnostic injection can be definitive. A local anesthetic (numbing medicine) is injected directly into the joint, often using ultrasound or X ray guidance to ensure accuracy.
If the patient’s pain disappears immediately after the injection, it confirms the joint is the pain generator. If the pain remains, the problem likely lies elsewhere, such as the spine or surrounding muscles. This prevents unnecessary surgery.
If a joint is swollen and warm, infection must be ruled out. Aspiration involves using a needle to draw fluid out of the joint. This fluid is sent to the lab for analysis.
High white blood cell counts in the fluid indicate infection or severe inflammation. Crystal analysis checks for gout or pseudogout. This is a critical step, as operating on an infected joint without knowing it can lead to catastrophic failure.
Blood work helps screen for systemic conditions. Erythrocyte Sedimentation Rate (ESR) and C Reactive Protein (CRP) are markers of inflammation. Elevated levels may suggest rheumatoid arthritis or an underlying infection.
Rheumatoid factor and anti CCP antibodies help diagnose rheumatoid arthritis. Preoperative blood work also checks for anemia, kidney function, and nutritional status to ensure the patient is medically optimized for surgery.
In complex cases, computerized gait analysis provides objective data on how the patient moves. Sensors attached to the body track joint angles and forces during walking.
This helps identify subtle biomechanical issues that may affect the outcome of the surgery. It is particularly useful for planning complex realignments or for patients with neuromuscular conditions like cerebral palsy.
Bone quality is as important as bone shape. A DEXA scan measures bone mineral density. Patients with severe osteoporosis may need cemented implants rather than press fit ones, as their bone may be too soft to grip the metal.
Identifying poor bone quality allows the surgeon to prepare specific implants or use gentle techniques to prevent fractures during the surgery. It also prompts treatment for osteoporosis to protect the implant long term.
A nuclear bone scan detects areas of high metabolic activity in the bone. It is highly sensitive but not very specific. It helps detect loosening of previous implants, stress fractures, or metastatic disease.
It is often used when a patient has pain after a joint replacement but the X rays look normal. A “hot spot” on the scan indicates that the bone is reacting to stress or movement, pointing to loosening or infection.
Send us all your questions or requests, and our expert team will assist you.
If your surgeon uses a robotic assistant, the CT scan is used to build a 3D map of your knee. This allows the robot to know exactly where your bone is during surgery, ensuring the cuts are precise and the implant fits perfectly.
Yes. If a cortisone shot relieves your pain, even temporarily, it confirms that the pain is coming from inflammation inside that specific joint. It acts as both a treatment and a diagnostic test.
We treat people, not X-rays. If you have severe arthritis on X-ray but function well and have little pain, surgery is generally not recommended. Surgery is for pain relief and quality of life, not just to fix a picture.
Standard MRIs cannot see well around metal implants due to artifacts. However, specialized metal suppression MRIs (MARS) can see fluid or tissue reactions around an implant, helping to diagnose loosening or soft tissue issues.
The nerves that supply the hip and leg come from the lower back. Arthritis in the spine (stenosis) can pinch these nerves and cause pain that feels like it is in the hip or thigh. This is called “referred pain.”




Shoulder arthroscopy is a common orthopedic procedure. It’s done thousands of times a year in the U.S. The American Academy of Orthopaedic Surgeons says arthroscopic


Joints are essential components of the skeletal system, providing both movement and flexibility. Did you know we have over 300 joints in our body? Each

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)