Orthopedics focuses on the musculoskeletal system. Learn about the diagnosis, treatment, and rehabilitation of bone, joint, ligament, and muscle conditions.
Send us all your questions or requests, and our expert team will assist you.
The necessity for joint replacement arises when the articular cartilage that cushions the ends of the bones wears away or is destroyed. This exposes the underlying nerve rich bone, causing severe pain and inflammation. While osteoarthritis is the most common culprit, several biological and mechanical pathways can lead to end stage joint failure.
Understanding the root cause of the joint destruction is vital for treatment planning. For example, the surgical approach for a joint destroyed by an autoimmune disease may differ from one destroyed by a traumatic fracture. The quality of the bone, the condition of the soft tissues, and the patient’s systemic health are all influenced by the etiology of the arthritis.
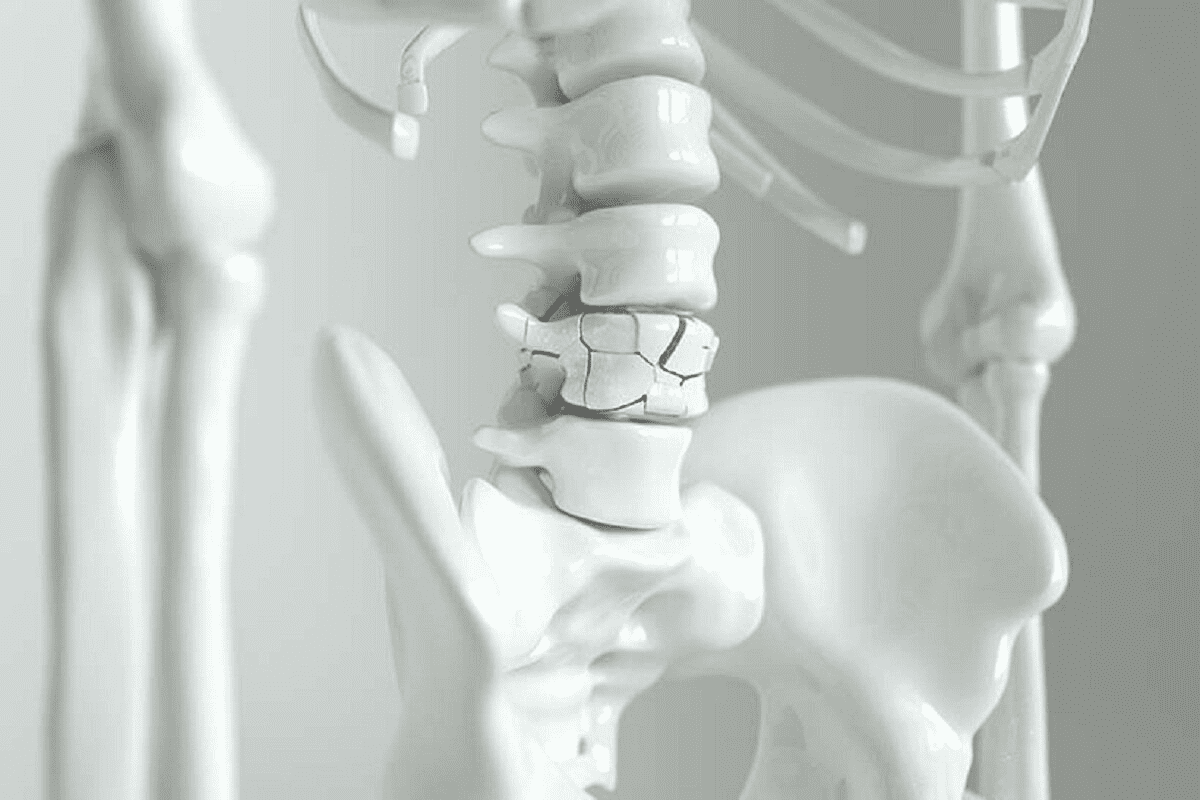
Regardless of the cause, the end result is a mechanical failure of the joint. The smooth gliding surfaces become rough and irregular, the joint space collapses, and the body attempts to stabilize the joint by growing extra bone (spurs), which further restricts motion.

Osteoarthritis is the most prevalent cause of joint replacement. It is a degenerative “wear and tear” condition that occurs over time. The cartilage breaks down, becoming frayed and rough. As the protective buffer disappears, the joint space narrows.
This process is not purely mechanical; it involves a complex biological response. The bone beneath the cartilage hardens (sclerosis), and the joint capsule thickens. Risk factors include aging, obesity, genetics, and previous injuries to the joint.

Rheumatoid arthritis is a systemic autoimmune disease. The body’s immune system attacks the synovium, the lining of the joint capsule. This chronic inflammation produces enzymes that aggressively digest cartilage and bone.
Unlike OA, which creates bone spurs, RA causes bone erosion. The bone becomes soft and osteopenic. This affects the surgical strategy, as the surgeon must be careful with the softer bone and may need to use specific fixation methods to ensure the implant is stable.
Injuries such as fractures or dislocations can damage the joint surface directly or alter the mechanics of the joint. Even if a fracture heals, the disruption to the smooth cartilage surface can start a cascade of degeneration that leads to arthritis years later.
This condition often affects younger patients. The anatomy may be distorted by previous hardware (plates and screws) or malunion of the bones. Surgeons must often remove old hardware and correct deformities during the replacement surgery.

Avascular necrosis, or osteonecrosis, is the death of bone tissue due to a lack of blood supply. This is most common in the hip but can affect the knee and shoulder. When the bone dies, it loses its structural integrity and collapses.
The overlying cartilage, having lost its foundation, also collapses and the joint surface becomes irregular. AVN can be caused by steroid use, alcohol consumption, trauma, or it can be idiopathic (cause unknown).
Developmental Dysplasia of the Hip (DDH) is a condition where the hip socket is shallow or malformed. This results in a smaller contact area for the femoral head, leading to massively increased pressure on the cartilage.
Over time, this mechanical overload wears out the joint prematurely. Patients with dysplasia often require hip replacement in their 40s or 50s. The anatomy is often altered, requiring specialized implants or surgical techniques to reconstruct the socket in the correct position.
In the shoulder, massive, chronic tears of the rotator cuff tendons can lead to a specific type of arthritis. Without the rotator cuff to hold the humerus centered in the socket, the large deltoid muscle pulls the arm bone upward.
This abnormal motion causes the humerus to rub against the acromion bone above it, destroying the joint surface. A standard shoulder replacement will not work here; a reverse total shoulder replacement is required to change the mechanics of the joint.
An infection within a joint can rapidly destroy cartilage. Bacteria release enzymes that digest the joint surface. Even after the infection is cleared with antibiotics and washouts, the damage left behind is permanent.
Joint replacement in a previously infected joint carries a higher risk of reinfection. Surgeons typically require a long period of being infection free and rigorous testing to ensure the joint is sterile before implanting a prosthetic.
Certain hip disorders in childhood can lead to arthritis in adulthood. Legg Calve Perthes disease involves a temporary loss of blood supply to the hip in children, leading to a misshapen femoral head. Slipped Capital Femoral Epiphysis (SCFE) involves the ball of the hip slipping off the neck.
These conditions leave the hip joint incongruent. The mismatch in shape acts like a square peg in a round hole, grinding down the cartilage over decades and necessitating replacement in young adulthood.
Patients with hemophilia suffer from recurrent bleeds into their joints (hemarthrosis). Blood is toxic to cartilage; the iron in red blood cells damages the chondrocytes and causes the synovium to become thick and inflamed.
Repeated bleeds lead to severe, rapid destruction of the joints, often at a very young age. Joint replacement in these patients requires careful coordination with hematologists to manage clotting factors and prevent excessive bleeding during surgery.
Gout involves the deposition of uric acid crystals in the joint. Pseudogout involves calcium pyrophosphate crystals. These crystals act like sandpaper, physically grinding the cartilage surface.
Chronic, uncontrolled crystal disease can cause massive erosions and destruction of the joint architecture. While medication manages the acute flares, the structural damage is irreversible and may require arthroplasty for pain relief.
Send us all your questions or requests, and our expert team will assist you.
The pain comes from several sources. The exposed bone is full of nerve endings, so bone rubbing on bone is painful. The lining of the joint (synovium) becomes inflamed and swollen. Additionally, the muscles around the joint often spasm in an attempt to protect it.
Changes in barometric pressure can affect the pressure inside the joint capsule. In an arthritic joint, the capsule is often scarred or inflamed, making it hypersensitive to these pressure shifts, which the brain interprets as pain or stiffness.
There is a genetic component to osteoarthritis. If your parents had joint replacements, you are at a higher risk. However, genetics is not destiny; lifestyle factors like weight, activity level, and injury history play a huge role in whether the genes are expressed.
You cannot regrow cartilage, but you can slow the progression. Maintaining a healthy weight reduces the load on the joint. Low impact exercise keeps the muscles strong and the joint lubricated. Anti inflammatory diets may also help reduce systemic inflammation.
Trauma, such as an ACL tear or a meniscus injury, changes the mechanics of the knee. Even if fixed, the joint may never move perfectly again. This subtle instability or uneven loading creates “hot spots” of wear that eventually turn into arthritis.


Joints are essential components of the skeletal system, providing both movement and flexibility. Did you know we have over 300 joints in our body? Each


Oprah Winfrey is a well-known media executive and former talk show host. Recently, her health has been a topic of interest. This is mainly because

Shoulder arthroscopy is a common orthopedic procedure. It’s done thousands of times a year in the U.S. The American Academy of Orthopaedic Surgeons says arthroscopic


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)