Stem cells can develop into many cell types and act as the body’s repair system. They replace or restore damaged tissues, offering new possibilities for treating diseases.
Send us all your questions or requests, and our expert team will assist you.

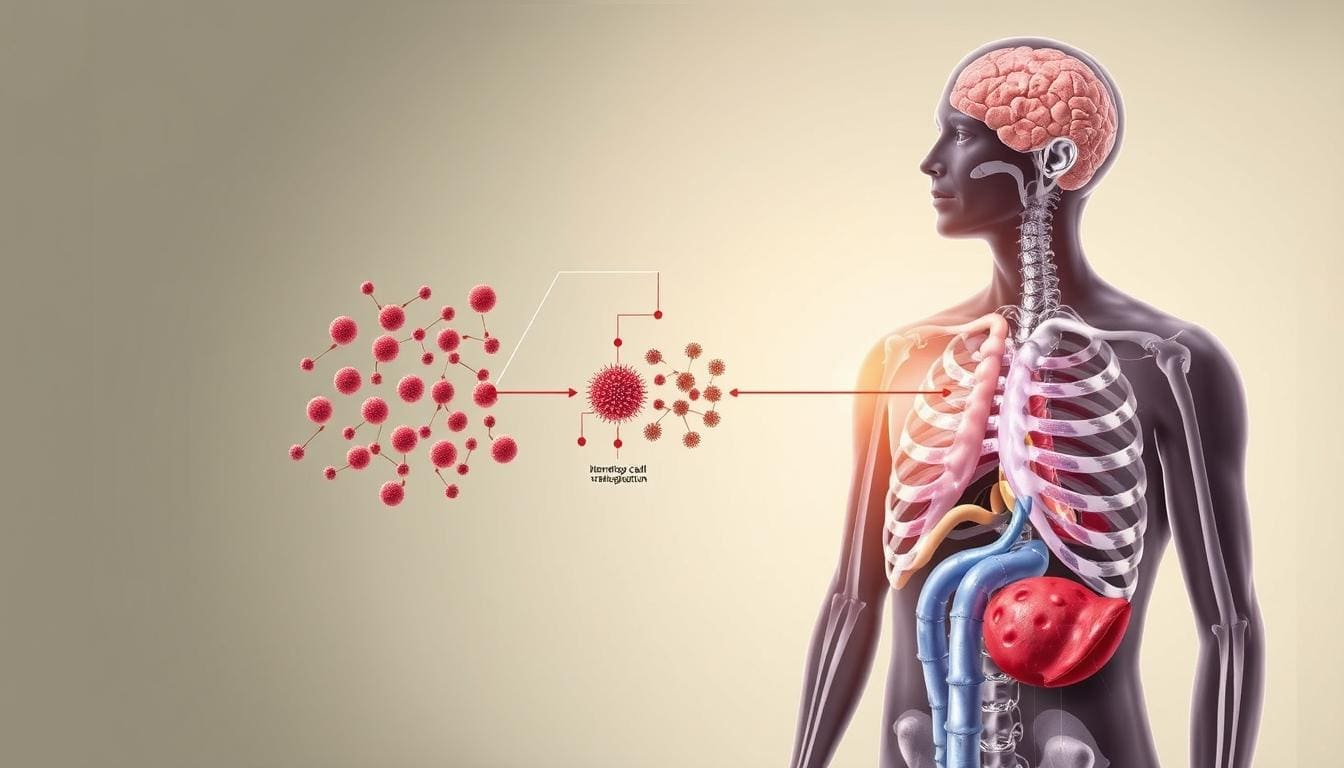
Multiple myeloma is a type of blood cancer that starts in plasma cells, which are a kind of white blood cell important for the immune system. To understand this disease, it helps to know what plasma cells normally do. They develop from B-lymphocytes in the bone marrow and are responsible for making antibodies (immunoglobulins). These antibodies help the body recognize and fight off bacteria and viruses. In healthy people, plasma cells multiply when needed to fight infection and then die off naturally once the infection is gone.
In multiple myeloma, a genetic change happens in one plasma cell. This change stops the cell from dying and causes it to multiply out of control. The result is a group of identical cells, called monoclonal gammopathy. Unlike healthy plasma cells that make many types of antibodies, these cancerous cells make large amounts of just one abnormal antibody, called the M-protein or paraprotein. This abnormal protein does not help the immune system and can build up in the blood and urine, leading to kidney and other organ problems.
The disease is termed “multiple” myeloma because it typically affects multiple areas of the bone marrow simultaneously. The malignant cells accumulate within the spongy marrow tissue of the bones—including the spine, skull, pelvis, and ribs—crowding out the healthy hematopoietic stem cells that produce red blood cells, white blood cells, and platelets. This invasion of the marrow space is the fundamental link between myeloma and regenerative medicine. The pathology is essentially a failure of the bone marrow’s regulatory environment, and the most effective long-term therapies often involve resetting this environment through stem cell transplantation.

Myeloma cells act like parasites in the bone marrow. They do more than just take up space—they change the nearby cells to help themselves survive. They release chemicals that encourage new blood vessels to grow and weaken the local immune response.
Furthermore, myeloma cells disrupt the delicate balance of bone remodeling. Healthy bone is in a constant state of flux, maintained by osteoblasts (cells that build bone) and osteoclasts (cells that break down bone). Myeloma cells overstimulate the osteoclasts and inhibit the osteoblasts. This uncoupling results in the rapid destruction of bone tissue, leading to the lytic lesions (holes in the bone), fractures, and severe bone pain that characterize the disease. This aspect of the disease highlights the importance of a multidisciplinary approach to care, integrating hematology with orthopedics and regenerative bone therapies.

Doctors first described multiple myeloma in the mid-1800s, when Samuel Solly and Henry Bence Jones found unusual proteins in patients’ urine. For many years, the disease was almost always fatal and there were few treatments. In the mid-1900s, new drugs called alkylating agents helped relieve symptoms, but people still did not live long with the disease.
Major progress in treating myeloma came with advances in stem cell science. In the 1980s and 1990s, doctors started using high-dose chemotherapy followed by a transplant of the patient’s own stem cells. This approach helped people live longer and feel better. Now, treatment also includes new drugs like proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies, often used together with stem cell transplants to achieve better results.

Multiple myeloma is the second most common blood cancer worldwide, after non-Hodgkin lymphoma. It mostly affects older adults, with most people diagnosed in their mid-to-late 60s, though younger people can also get it. The disease is a bit more common in men than women and is much more common in African American populations. Researchers are studying possible genetic and environmental reasons for these differences.
Researchers often use myeloma to test new regenerative and immune-based treatments. Since myeloma cells live in the bone marrow and interact with the immune system, therapies like CAR-T cell therapy developed for myeloma are now being tried in other cancers. The goal has moved from just controlling the disease to aiming for a cure by targeting even the smallest traces of cancer. Leading hospitals, including those in the Liv Hospital network, use the latest treatments and share knowledge worldwide to help manage this chronic but treatable disease.
Send us all your questions or requests, and our expert team will assist you.
Lifting heavy weights increases intra-abdominal pressure. If a man performs this exertion with a full bladder, the high pressure can force urine backwards from the urethra into the ejaculatory ducts and down the vas deferens to the epididymis. This is called “urine reflux.” Urine is a chemical irritant to the delicate epididymal tissue and causes inflammation known as chemical epididymitis, which mimics the symptoms of an infection but is caused by sterile urine.
An enlarged prostate (BPH) obstructs the flow of urine out of the bladder. This forces the bladder to squeeze harder during urination, creating high internal pressure. It also prevents the bladder from emptying, allowing stagnant urine to accumulate where bacteria can grow. The combination of high pressure and infected urine increases the likelihood that bacteria will be pushed back into the reproductive tract, leading to epididymitis.
Amiodarone is a medication used to treat heart rhythm problems. It has a unique side effect: it accumulates to high concentrations in the epididymis. This buildup causes a non-infectious inflammation that leads to pain and swelling. It typically affects the head of the epididymis and resolves when the medication is reduced or discontinued, distinguishing it from bacterial infections.
Yes, a urinary tract infection (UTI) is a very common precursor to epididymitis, especially in older men or those with anatomical abnormalities. The bacteria causing the UTI (often E. coli) can migrate from the bladder or urethra, travel down the vas deferens, and colonize the epididymis. Treating the underlying UTI is essential to resolving the epididymitis and preventing recurrence.
Evidence suggests that uncircumcised infants and men may have a slightly higher risk of urinary tract infections due to bacteria colonizing the area under the foreskin. Since UTIs can ascend to the epididymis, there is a theoretical link. However, in sexually active adults, the risk is more strongly tied to sexual behaviors and barrier protection than to circumcision status alone.


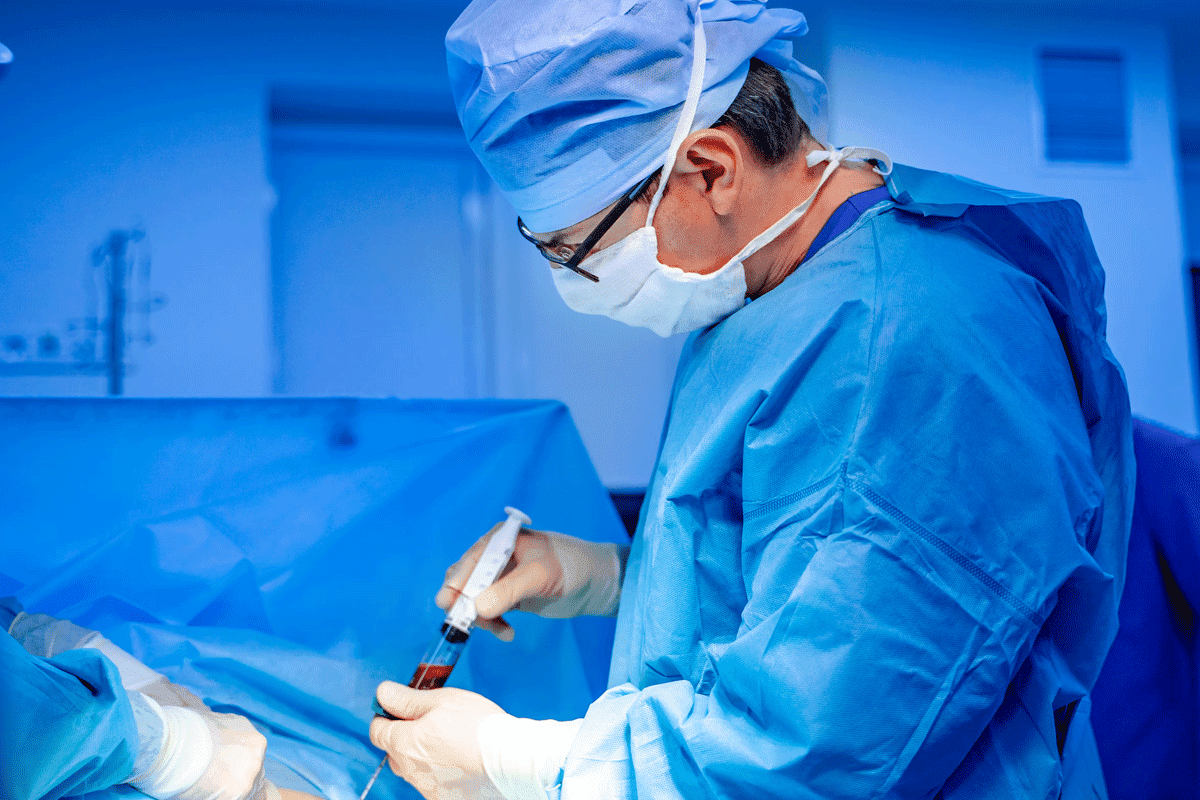
stem cell transplant for multiple myeloma Recent studies show that life expectancy after a stem cell transplant varies. This depends on the type of cancer


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)