Stem cells can develop into many cell types and act as the body’s repair system. They replace or restore damaged tissues, offering new possibilities for treating diseases.
Send us all your questions or requests, and our expert team will assist you.

The management of multiple myeloma has undergone a paradigm shift over the last two decades. The goal of treatment has evolved from simple symptom control to achieving deep, durable remissions and extending survival by many years. The standard approach for eligible patients involves a sequenced strategy: Induction therapy, Consolidation (typically with Stem Cell Transplantation), and Maintenance therapy. This comprehensive pathway leverages both pharmacological innovation and regenerative medicine principles.

The first phase of treatment is “Induction.” The objective is to rapidly reduce the number of myeloma cells in the body (tumor burden), reverse acute symptoms like kidney failure, and prepare the patient for stem cell collection.

For patients who are fit and eligible, high-dose chemotherapy followed by Autologous Stem Cell Transplantation remains the cornerstone of consolidation therapy. It utilizes the regenerative capacity of the patient’s own stem cells to deliver a chemotherapy dose that would otherwise be fatal to the bone marrow.
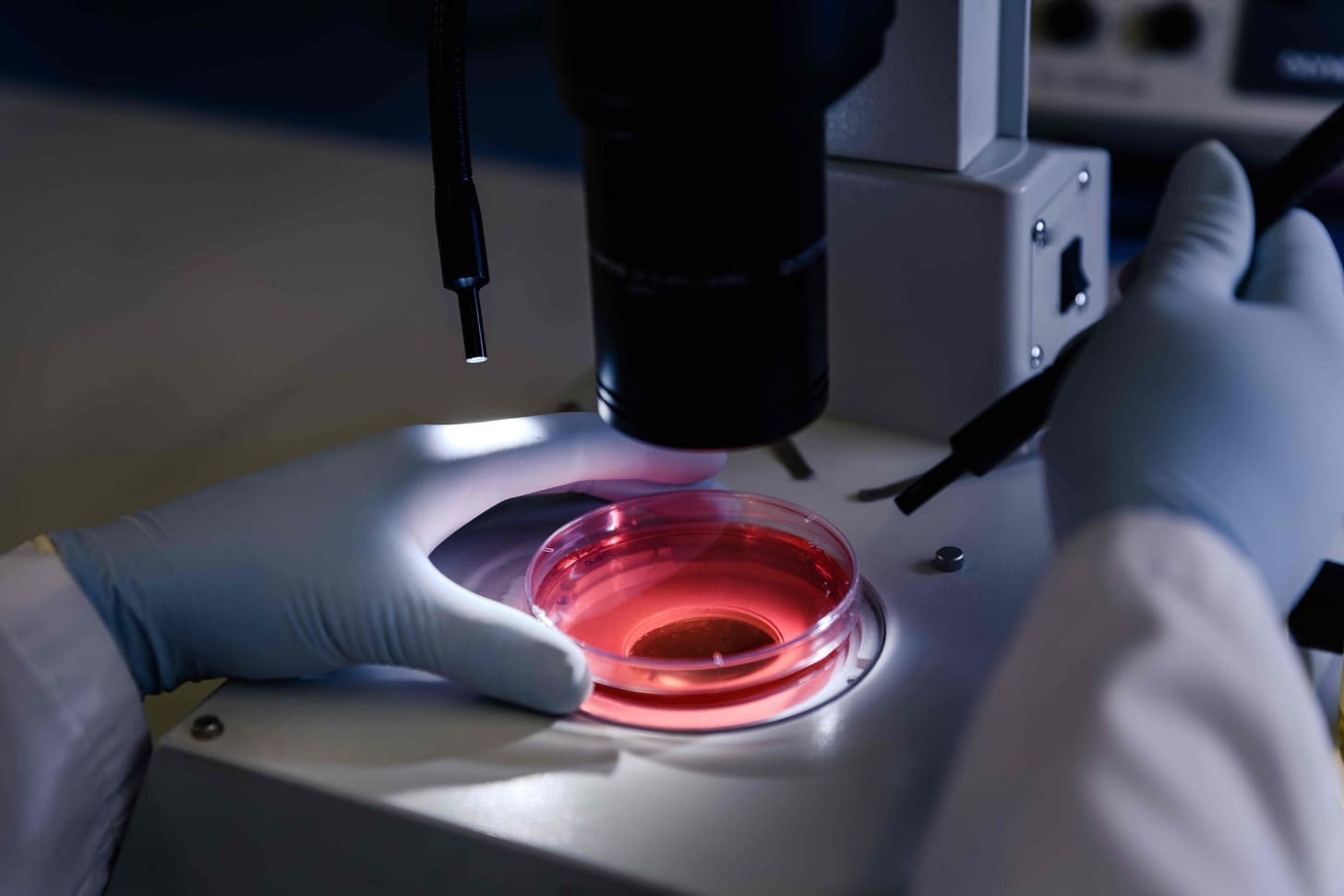
Phase 1: Mobilization and Collection (Apheresis)
After induction therapy reduces the cancer burden, the patient receives growth factors (G-CSF) to stimulate the bone marrow to release hematopoietic stem cells into the bloodstream. The patient is connected to an apheresis machine that draws blood, separates the stem cells, and returns the remaining blood to the patient. These stem cells are then cryopreserved (frozen) for later use.
Phase 2: Conditioning
The patient is admitted to the hospital or a specialized outpatient unit. They receive a high dose of chemotherapy, typically Melphalan. This drug is a potent alkylating agent that is highly effective at killing myeloma cells in the bone marrow. However, it also destroys the healthy blood-forming stem cells.
Phase 3: Reinfusion (The Transplant)
A day or two after the chemotherapy is cleared from the body, the frozen stem cells are thawed and infused back into the patient’s vein, similar to a blood transfusion. These cells navigate through the bloodstream, “home” to the bone marrow cavities, and begin regenerating a new, healthy blood and immune system.

In rare cases, an Allogeneic transplant (using stem cells from a donor) may be considered. Unlike autologous transplants, this relies on the “Graft-Versus-Myeloma” effect, where the donor’s immune system attacks the cancer. However, due to higher risks of complications like Graft-Versus-Host Disease, this is generally reserved for younger patients with very high-risk disease or those who have relapsed after multiple other therapies.

Following the transplant, patients typically start Maintenance Therapy. This involves taking a lower dose of medication (usually an immunomodulatory drug) for an extended period. The goal is to suppress any microscopic residual disease and keep the myeloma in remission for as long as possible.

Regenerative care in myeloma also focuses on the skeleton.

When myeloma relapses, advanced cellular therapies offer new hope.
The main benefit is that it allows doctors to use a very high dose of chemotherapy (Melphalan) to kill as many cancer cells as possible. The stem cells are simply a rescue mechanism to restore the blood counts afterwards. Studies show that this intensive approach significantly prolongs the time a patient stays in remission compared to chemotherapy alone.
No, despite the name, a stem cell transplant is not a surgical procedure. The collection of cells is done with a machine similar to a dialysis machine, and the reinfusion of cells is via an IV line, just like a blood transfusion. The “transplant” refers to the transfer of cells, not an operation.
Hair loss is uncommon with many of the modern induction drugs (like Bortezomib or Lenalidomide). However, the high-dose Melphalan used during the stem cell transplant process does cause temporary hair loss. The hair typically regrows within 3 to 6 months after the procedure.
The typical hospital stay for an autologous stem cell transplant is approximately 2 to 3 weeks. This time is needed for the chemotherapy to be administered and, more importantly, for the new stem cells to engraft and produce enough white blood cells to protect the patient from infection before they go home.
If myeloma relapses, there are many remaining treatment options. Patients can be treated with different classes of drugs they haven’t seen before, second-generation novel agents, or newer immunotherapies like CAR-T cells. In some selected cases, a second stem cell transplant may even be considered.






Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)