Cardiology is the medical specialty focused on the heart and the cardiovascular system. It involves the diagnosis, treatment, and prevention of conditions affecting the heart and blood vessels. These conditions include coronary artery disease, heart failure, arrhythmias (irregular heartbeats), and valve disorders. The field covers a broad spectrum, from congenital heart defects present at birth to acquired conditions like heart attacks.
Send us all your questions or requests, and our expert team will assist you.

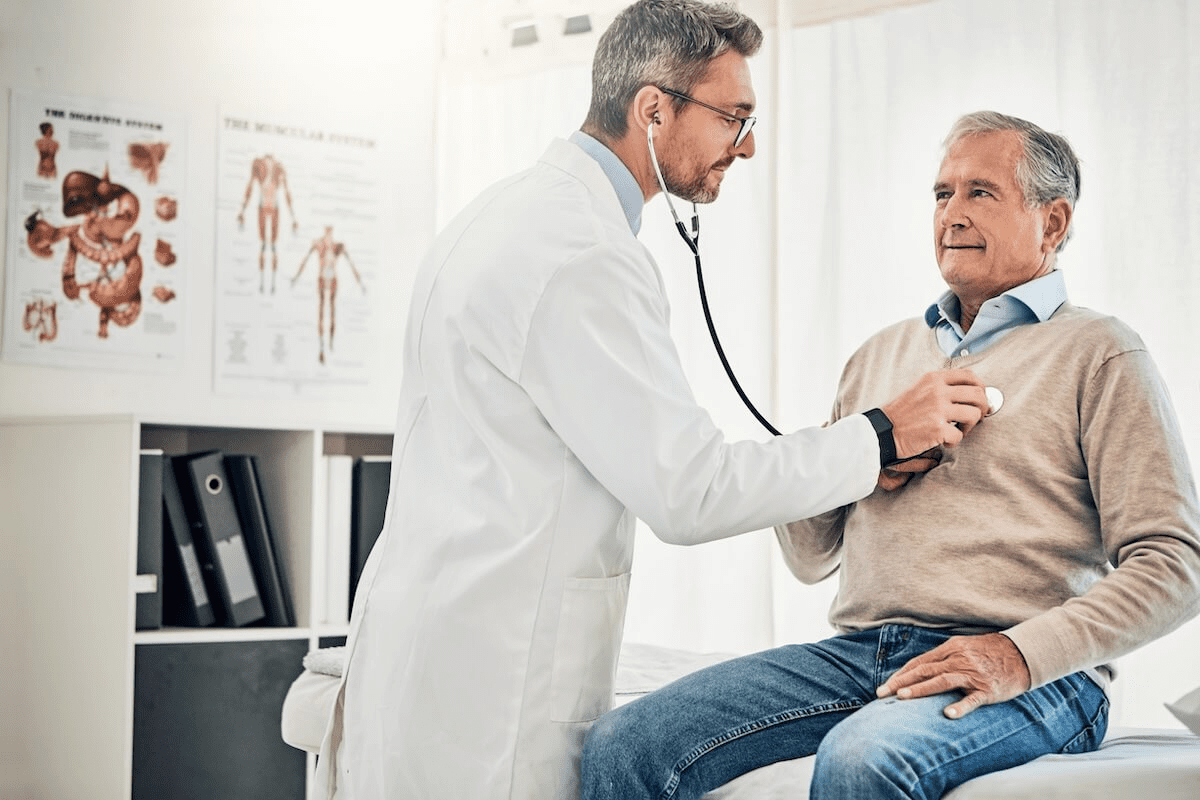
Diagnosing heart valve disease is a step-by-step process that moves from the simple to the complex. Often, the journey begins during a routine check-up when a doctor hears something unusual through their stethoscope. Heart valve issues often produce sound, unlike some internal problems that remain hidden until they cause pain. This sound, known as a murmur, is the turbulence of blood flowing through a narrowed or leaking valve. However, hearing a murmur is just the first clue. It tells the doctor that there is turbulence, but not why or how severe it is.
To get a complete picture, doctors use various tests. These tests are designed to visualize the heart’s structure, measure the blood flow, check the heart’s electrical rhythm, and assess how well the heart functions under stress. Most of these tests are non-invasive, meaning they don’t require surgery or needles (other than perhaps an IV line). They are safe and provide the critical data needed to decide if surgery is necessary, what type of surgery is best, and when it should be performed. Accuracy in diagnosis is the foundation of a successful treatment plan.
The physical exam is the cornerstone of diagnosis. Your doctor will start by checking your blood pressure and pulse. They will look for physical signs like swollen ankles or pulsing neck veins. Then, they will use a stethoscope to listen to your heart sounds at various points on your chest. A normal heart makes a “lub-dub” sound as the valves close. If a valve is diseased, the doctor might hear a “whooshing” or “clicking” noise.
The timing, loudness, and location of this murmur give the doctor a lot of information. For example, a murmur heard during the “lub” part of the beat might indicate a problem with the mitral valve, while a murmur during the “dub” might point to the aortic valve. The doctor might ask you to lean forward, roll onto your side, or hold your breath to hear the sound better. While a skilled doctor can learn a lot just by listening, a murmur alone is not enough to plan surgery. It simply signals the need for more advanced testing.
The echocardiogram, often just called an “echo,” is the most important test for diagnosing valve disease. It is essentially an ultrasound of the heart. It uses sound waves to create moving pictures of your heart on a screen. This allows the doctor to see the valves opening and closing in real-time. They can measure the size of the heart chambers, the thickness of the heart muscle, and the speed of the blood flowing through the valves.
There are two main types of echocardiograms. The standard one is non-invasive and painless. The specialized one provides a closer look. Both are crucial for determining the severity of the valve defect—whether it is mild, moderate, or severe. This grading is the primary factor in deciding when to operate.
This is the standard echo. A technician puts a cool gel on your chest and moves a wand-like device called a transducer over your skin. The transducer sends sound waves into the chest, which bounce off the heart and return to create an image. It is painless, safe, and takes about 30 to 45 minutes. It gives a fantastic overall view of the heart’s function.
Occasionally, the standard echo doesn’t show enough detail because the ribs or lungs get in the way. In a TEE, a small transducer is attached to a flexible tube. After your throat is numbed and you are given medication to relax, this tube is guided down your esophagus (the food pipe). Since the esophagus sits right behind the heart, this technique provides incredibly clear, close-up images of the valves. It is often done to plan the specific details of a surgery.

An electrocardiogram, abbreviated as ECG or EKG, is a quick and simple test that records the electrical activity of the heart. Small sticky patches called electrodes are placed on your chest, arms, and legs. These are connected by wires to a machine that traces the electrical waves that make your heart beat. It only takes a few minutes.
While an ECG cannot “see” the valves, it shows the effects of valve disease. For example, if a valve is narrow and the heart has to work harder, the muscle thickens. The electrical pattern on the ECG changes because of this thickening. It can also detect irregular heart rhythms, like atrial fibrillation, which is a common complication of mitral valve disease. It is a vital screening tool that provides a snapshot of the heart’s electrical health.

Sometimes, doctors need more detail than an echo can provide. This is where Cardiac MRI (Magnetic Resonance Imaging) and Cardiac CT (Computed Tomography) scans come in. A cardiac MRI uses powerful magnets to create detailed still and moving images. It is excellent for measuring exactly how much blood is leaking through a valve and for assessing the health of the heart muscle itself—specifically, looking for scar tissue.
A cardiac CT scan uses X-rays to create detailed 3D images of the heart. It is particularly useful for looking at the aorta and checking for calcium buildup on the valves. For patients being considered for TAVR (the catheter-based replacement), a CT scan is mandatory because it allows doctors to measure the exact size of the valve to the millimeter, ensuring the new artificial valve fits perfectly. These tests are painless but require you to lie still inside a scanner.
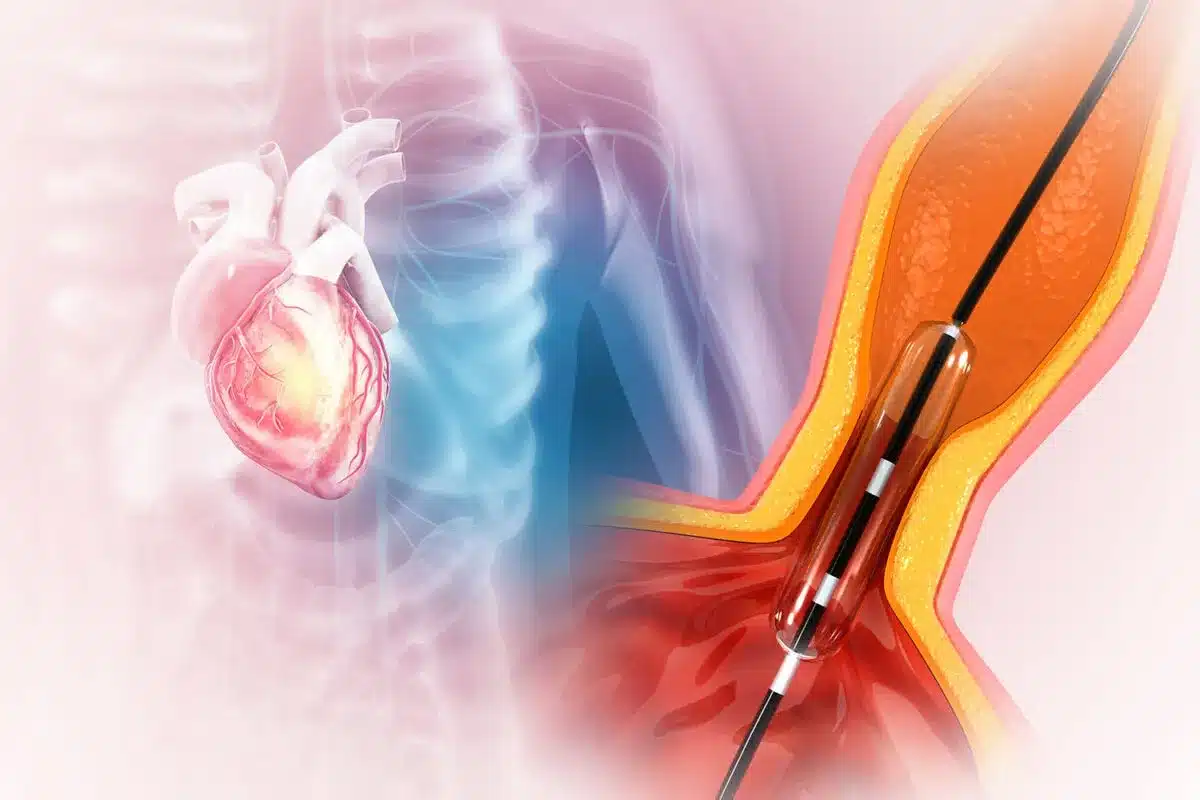
Cardiac catheterization, often called an angiogram, is an invasive diagnostic procedure. It is usually the final test done before surgery. A doctor inserts a long, thin tube (catheter) into a blood vessel in your wrist or groin and threads it up to the heart. Contrast dye is injected through the tube, and X-ray movies are taken.
The primary purpose of this test before valve surgery is to check the coronary arteries. The doctor needs to know if there are any blockages (coronary artery disease) supplying the heart muscle. If blockages are found, the surgeon might need to perform bypass surgery at the same time as the valve surgery. This test also allows for direct measurement of the pressures inside the heart chambers, which helps confirm the severity of the valve blockage or leak.

Sometimes symptoms only appear when the heart is working hard. A stress test helps reveal these hidden issues. You will be asked to walk on a treadmill while hooked up to an ECG monitor. The speed and incline increase gradually. The doctor watches to see how your heart handles the extra workload. Does your blood pressure drop? Does the rhythm change? Do you get short of breath immediately? This indicator helps determine if it is safe to wait or if surgery is needed soon.
A Holter monitor is a portable ECG device that you wear for 24 to 48 hours while you go about your normal daily life. It records every heartbeat. This is useful for detecting intermittent rhythm problems that a 10-second ECG in the office might miss. It helps correlate your symptoms—like a flutter in your chest—with the actual heart rhythm at that moment.

Send us all your questions or requests, and our expert team will assist you.
No, a standard transthoracic echocardiogram is completely painless. It involves a plastic wand moving over your skin with some gel. A transesophageal echo (TEE) can be slightly uncomfortable due to the tube in the throat, but you are given medication to help you relax and often don’t remember it.
You need it to check the arteries around the heart. If those arteries are clogged, fixing the valve alone won’t be enough. Surgeons need to know if they need to perform a bypass and a valve repair at the same time.
Not usually. They provide different information. The echo is best for seeing the motion of the valves and blood flow. The CT scan is best for seeing the static structure, calcification, and precise measurements of the anatomy. They complement each other.
The amount of radiation from a cardiac CT or angiogram is carefully controlled and is considered low risk, especially compared to the risk of untreated heart valve disease. MRI and echocardiograms do not use any radiation at all.
You typically need to wear comfortable clothes and walking shoes. You may be asked not to eat or drink caffeine for a few hours before the test. Your doctor might also ask you to stop taking certain heart medications on the day of the test so they don’t mask the results.

Heart valve problems affect millions globally, with 1 in 4 people over 65 facing valve disease. It’s vital to tackle these issues quickly and effectively.

Find out the key average time for heart valve replacement surgery duration. Get powerful facts and know what to expect. Heart valve disease affects millions
Heart valve disorders affect millions worldwide, with many needing surgery. Surprisingly, nearly 1 in 5 patients undergoing heart surgery has a challenging heart condition that

Heart valve disease affects millions worldwide. Valvular repair surgery is a life-changing treatment for many. Recent data shows that medical technology advancements, like those by
Did you know that heart valve disorders affect over 4 million people in the United States? The mitral valve is one of the most commonly

Nearly 1 in 5 adults in the United States have heart valve disease. Mitral valve issues are very common. Mitral valve repair surgery is a

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)