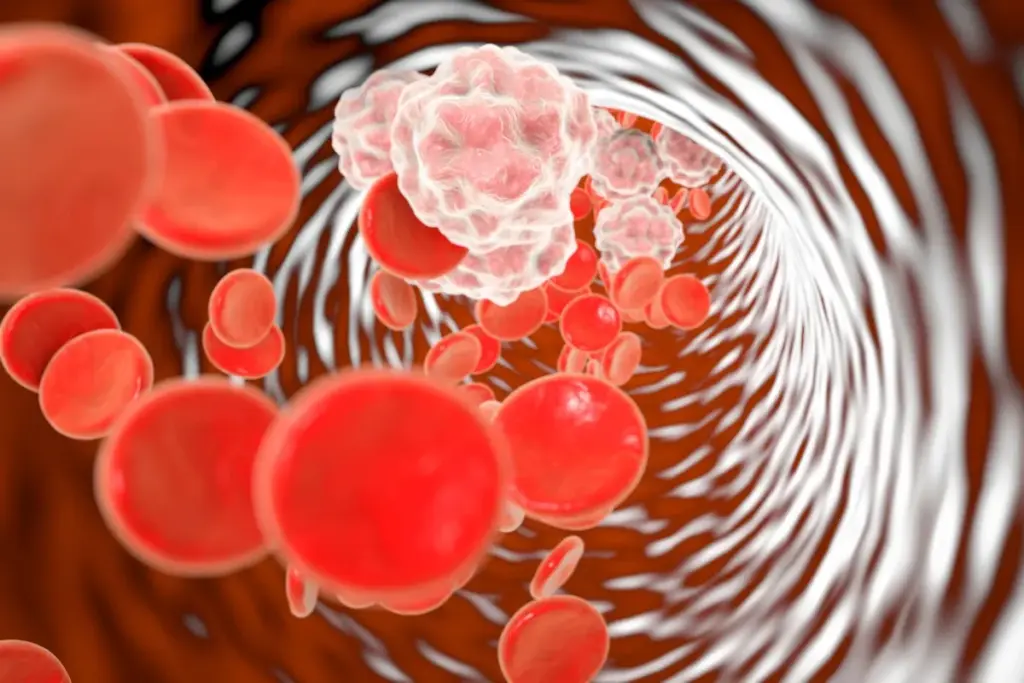
Cardiology is the medical specialty focused on the heart and the cardiovascular system. It involves the diagnosis, treatment, and prevention of conditions affecting the heart and blood vessels. These conditions include coronary artery disease, heart failure, arrhythmias (irregular heartbeats), and valve disorders. The field covers a broad spectrum, from congenital heart defects present at birth to acquired conditions like heart attacks.
Send us all your questions or requests, and our expert team will assist you.
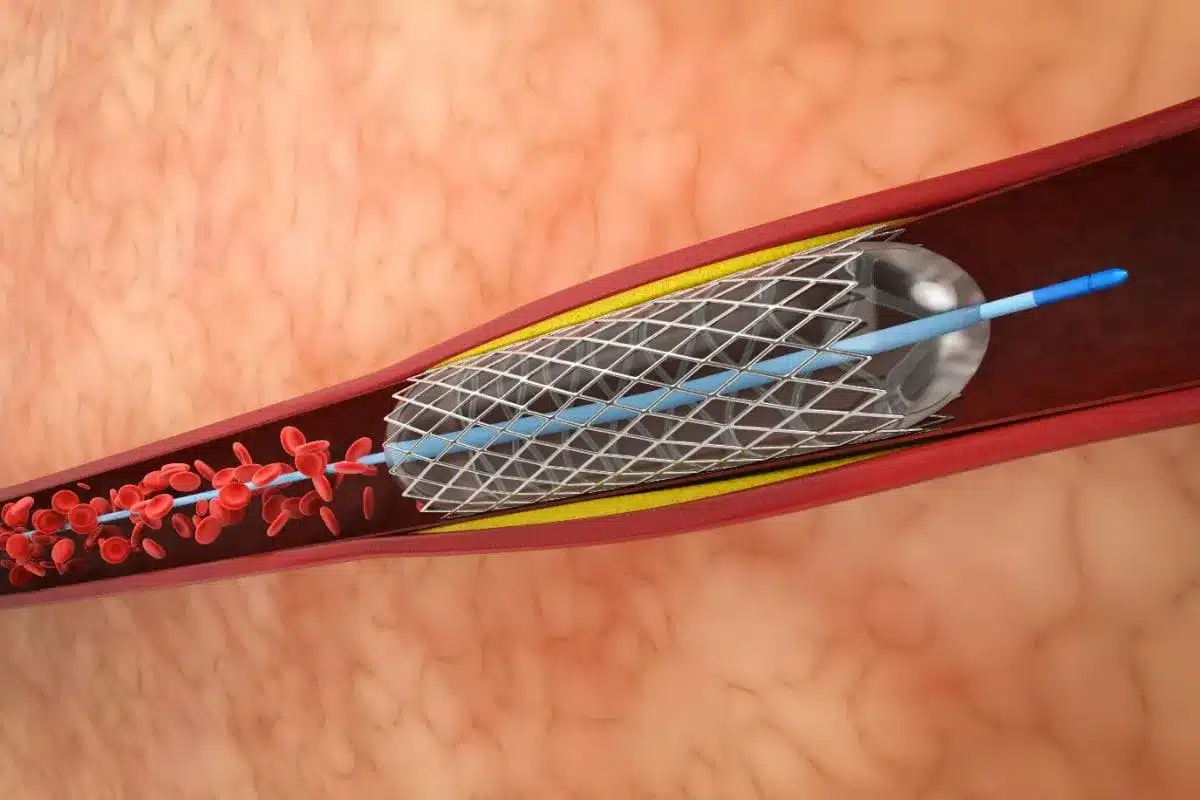
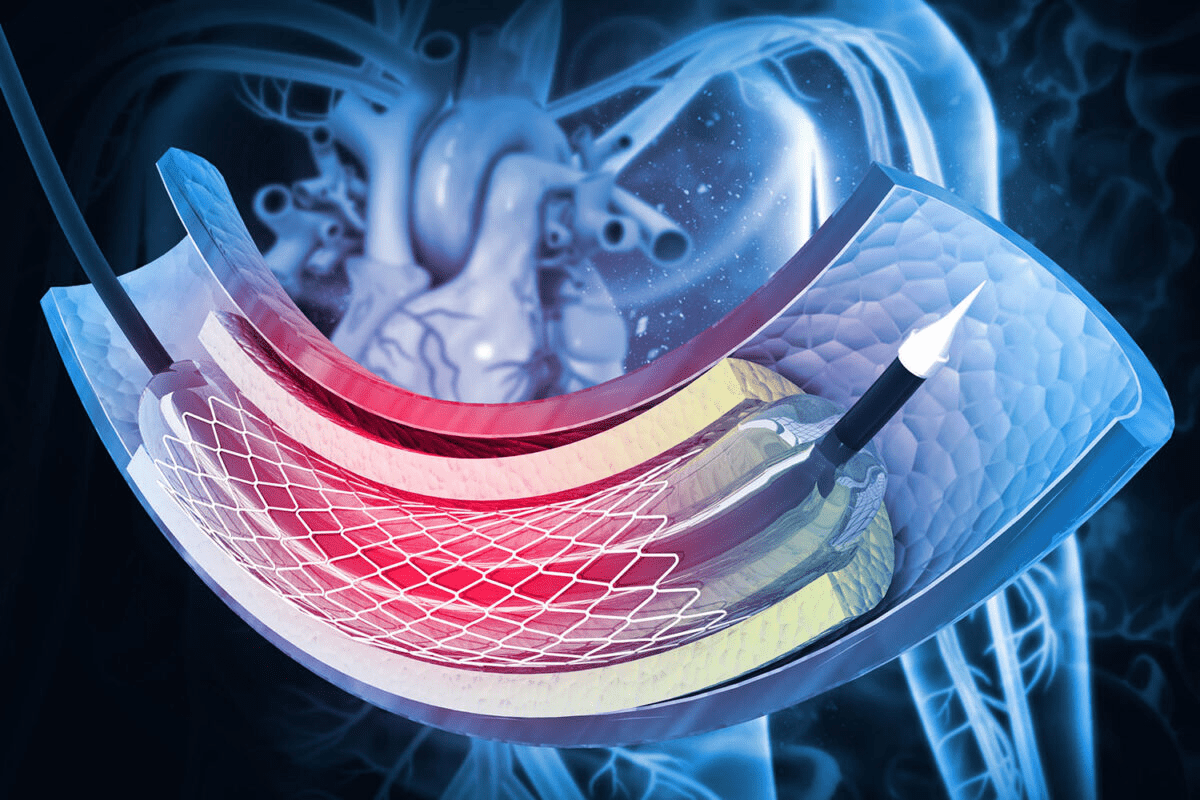
Doctors usually decide to place a coronary stent as part of a larger treatment plan. It is usually the result of a chain of events starting with specific symptoms that warn of heart trouble. Understanding these symptoms is vital because the earlier a blockage is found, the easier it is to treat, and the less damage is done to the heart muscle. The symptoms of blocked arteries can be dramatic, like a sudden collapse, or they can be subtle, like a nagging fatigue that won’t go away.
Context is also important. Symptoms do not occur in a vacuum; they happen to people who usually have specific risk factors. Risk factors are the conditions or habits that make plaque buildup more likely. Some of these are things you are born with, while others are developed over time. By recognizing the connection between your lifestyle, your genetics, and the way you feel physically, you can become an active partner in identifying the need for intervention before a crisis occurs.
The most classic symptom indicating the need for a stent is angina. Angina is the medical term for chest pain or discomfort caused by reduced blood flow to the heart muscle. It is important to know that this often does not feel like sharp pain. Many patients describe it as a pressure, a squeezing sensation, a heaviness, or a feeling of fullness in the center of the chest. It might feel like a tight band is wrapped around your ribs or like a heavy weight is sitting on your breastbone.
This discomfort can be deceptive because it can radiate. This means the pain travels from the chest to other parts of the body. The pain often spreads to the left shoulder, left arm, neck, jaw, or back between the shoulder blades. Angina is typically triggered by physical exertion or emotional stress—times when the heart needs more oxygen than the blocked artery can supply.

Not everyone experiences chest pain. For many, particularly older adults and those with diabetes, the primary symptom of a blocked artery is shortness of breath. You might find yourself gasping for air after simple activities that used to be easy, like making the bed, carrying groceries, or walking to the mailbox. The condition is called “dyspnea.” It happens because the heart, weakened by a lack of oxygen, cannot pump efficiently, causing fluid to back up in the lungs or simply failing to deliver oxygenated blood to the muscles.
Profound fatigue is another subtle warning sign. This is not just feeling sleepy at the end of a long day; it is a deep, bone-weary exhaustion that does not improve with sleep. You might feel like your limbs are heavy or that walking feels like trudging through mud. This “exercise intolerance” is a key indicator that the heart’s fuel supply is compromised and that a stent might be needed to restore energy levels.
It is a frightening reality that coronary artery disease can be “silent.” This means a person can have significant blockages in their arteries without feeling any chest pain or shortness of breath. This is known as silent ischemia. It is particularly common in people with diabetes because high blood sugar can damage the nerves that transmit pain signals from the heart. These patients literally cannot feel the warning signs.
In these cases, the need for a stent might be discovered during a routine check-up when an electrocardiogram (ECG) shows abnormalities, or it might unfortunately be discovered only when a sudden heart attack occurs. This highlights the importance of screening and knowing your risk factors. Even if you feel fine, if you have high cholesterol and high blood pressure, your arteries could still be narrowing silently.

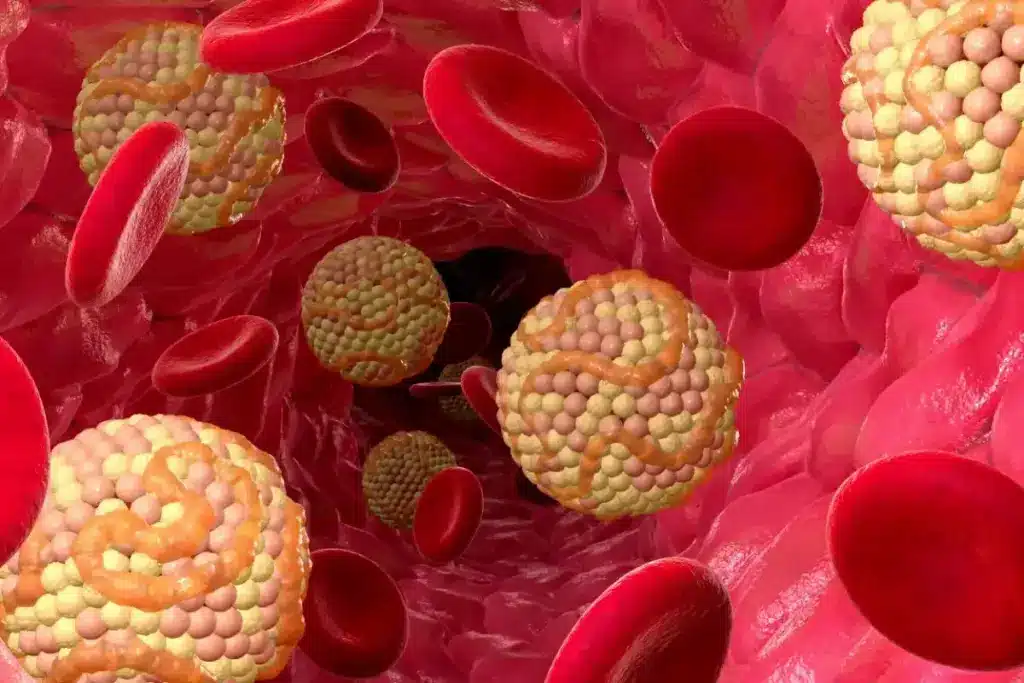
The primary biological driver for needing a stent is atherosclerosis, which is the buildup of plaque. Plaque is a sticky substance made of cholesterol, fat, calcium, and cellular waste. High levels of low-density lipoprotein (LDL), often called “bad cholesterol,” are the raw material for this plaque. When there is too much LDL in the bloodstream, it burrows into the inner lining of the artery walls.
Over time, this cholesterol deposit provokes an immune response. The body tries to wall it off, creating a rigid shell or a soft, inflamed bump inside the artery. As this bump grows, it intrudes into the channel where blood flows, narrowing it. Stents are the mechanical solution to push this plaque back against the wall and restore the channel’s width.
LDL is the bad cholesterol that clogs arteries. HDL is the “good” cholesterol that acts like a garbage truck, carrying fat away from the arteries to the liver. A healthy balance is crucial. If LDL is too high and HDL is too low, the risk of blockage skyrockets.
Doctors now know that inflammation plays a giant role. It is not just about grease in a pipe; the artery wall is inflamed and angry. This inflammation makes the plaque unstable and more likely to rupture, causing a heart attack.
Many of the factors that lead to needing a stent are under our control. Smoking is perhaps the single most significant preventable cause. The chemicals in tobacco smoke damage the lining of the blood vessels, making them rough and sticky, which invites plaque to form. Smoking also thickens the blood, increasing the risk of clots.
Diet and physical inactivity are also major contributors. A diet high in saturated fats, trans fats, sugar, and salt accelerates arterial damage. Being sedentary leads to weight gain and poor blood sugar control. Obesity puts a physical strain on the heart and is linked to chronic inflammation. Addressing these lifestyle factors are not only part of prevention but are also critical after getting a stent to ensure it stays open.
Some risks cannot be changed, but knowing them helps you stay vigilant. Age is the most common risk factor; as we get older, our arteries naturally become stiffer and more prone to plaque buildup. Gender also plays a role; men are generally at higher risk of developing coronary artery disease at a younger age than women, although a woman’s risk increases significantly after menopause.
Genetics and family history are powerful influencers. If your parents or siblings developed heart disease at a young age, you are statistically more likely to develop it too. This is not necessarily because you share habits, but because you may inherit how your body processes cholesterol or regulates blood pressure. Knowing your family history allows doctors to screen you earlier and perhaps intervene with a stent before a heart attack occurs.

Send us all your questions or requests, and our expert team will assist you.
Women are more likely to experience “atypical” symptoms. Instead of crushing chest pressure, they might feel nausea, extreme fatigue, shortness of breath, or pain in the back or jaw. Because these symptoms can mimic the flu or indigestion, they are often dismissed, leading to delayed treatment.
Stress itself does not put plaque in the artery, but chronic stress raises blood pressure and inflammation, which accelerates damage to the artery walls. Furthermore, sudden severe stress can trigger a plaque rupture in an already narrowed artery, leading to a heart attack.
Yes. Imagine a garden hose under extremely high pressure; eventually, the inner lining will crack or weaken. High blood pressure creates microscopic tears in the artery lining. Plaque loves to stick to these damaged rough spots, starting the blockage process.
Yes. While being overweight is a risk factor, thin people can still have high cholesterol, high blood pressure, and a strong genetic family history of heart disease. You cannot judge the health of your arteries by your waistline alone
Yes, diabetes is considered a major risk equivalent to having already had a heart attack. High blood sugar acts like slow-acting poison to the blood vessels, making them stiff and prone to extensive plaque buildup. Patients with diabetes often require multiple stents.


Did you know that over 100 million urinary catheters are used worldwide each year? This number shows how important catheters are in medical care. They
Every year, over a million people get a stent to fight coronary artery disease. This disease narrows or blocks the coronary arteries. Many wonder if
Knowing when a stent or bypass surgery is needed is key for both patients and doctors. At Liv Hospital, we focus on you, with top-notch

Coronary artery disease (CAD) is a big problem worldwide. It’s a leading cause of sickness and death. Stenting is a main treatment when arteries get

Coronary artery disease affects millions worldwide. For many, a stent procedure is a lifesaving intervention. But what does this mean for patients facing the prospect
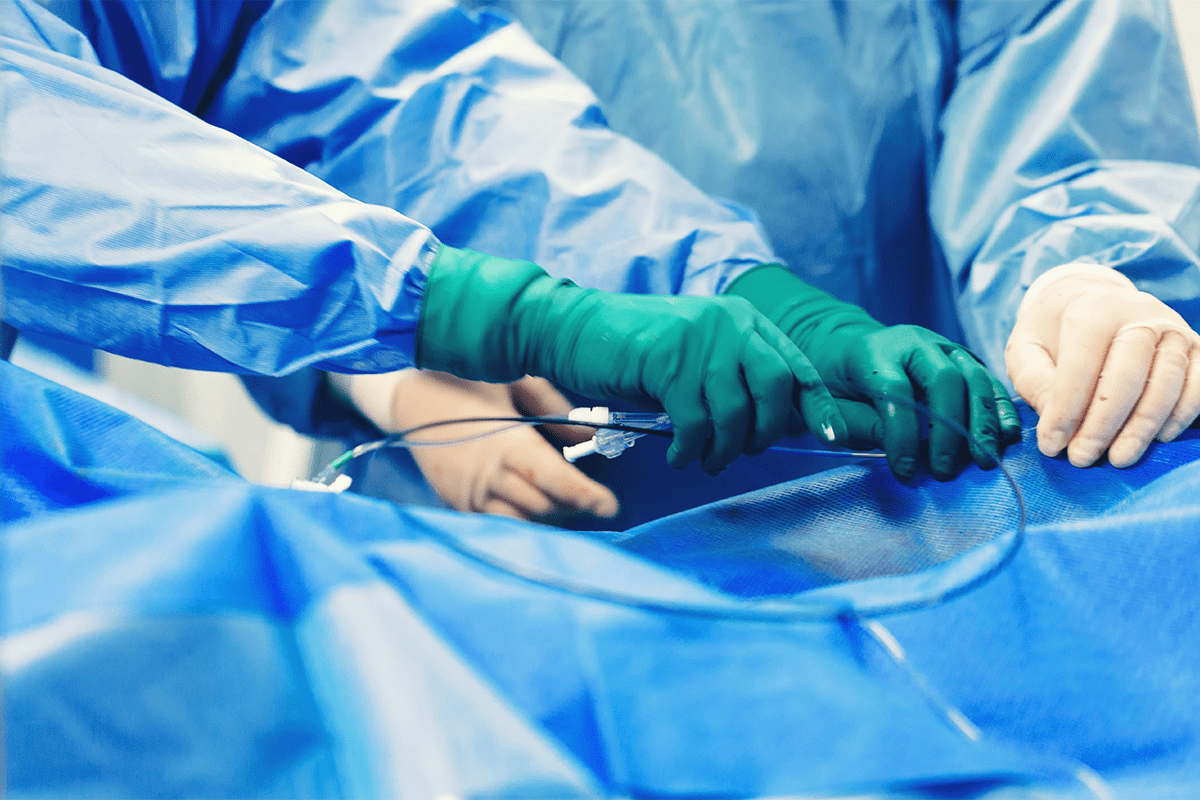
Every year, thousands of patients worldwide get help for blocked heart arteries. Choosing between minimally invasive treatments is a big decision. At Liv Hospital, we

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)