Urology treats urinary tract diseases in all genders and male reproductive issues, covering the kidneys, bladder, prostate, urethra, from infections to complex cancers.
Send us all your questions or requests, and our expert team will assist you.

The accurate diagnosis of a Urinary Tract Infection is the cornerstone of effective treatment and antibiotic stewardship. At Liv Hospital, the diagnostic pathway is designed to be rigorous and evidence-based, moving beyond empirical treatment to precise identification of the pathogen and the underlying anatomical status. While the diagnosis is often suspected based on clinical symptoms, confirmation requires objective laboratory testing. In cases of recurrent or complicated infections, advanced imaging and endoscopic evaluation become integral components of the workup to rule out structural anomalies or obstructions.
The diagnostic process begins with a comprehensive medical history and physical examination. The physician assesses the severity of symptoms, the duration of illness, and any potential complicating factors such as pregnancy, diabetes, or prior urological surgeries. Following this clinical assessment, a tiered approach to testing is employed.

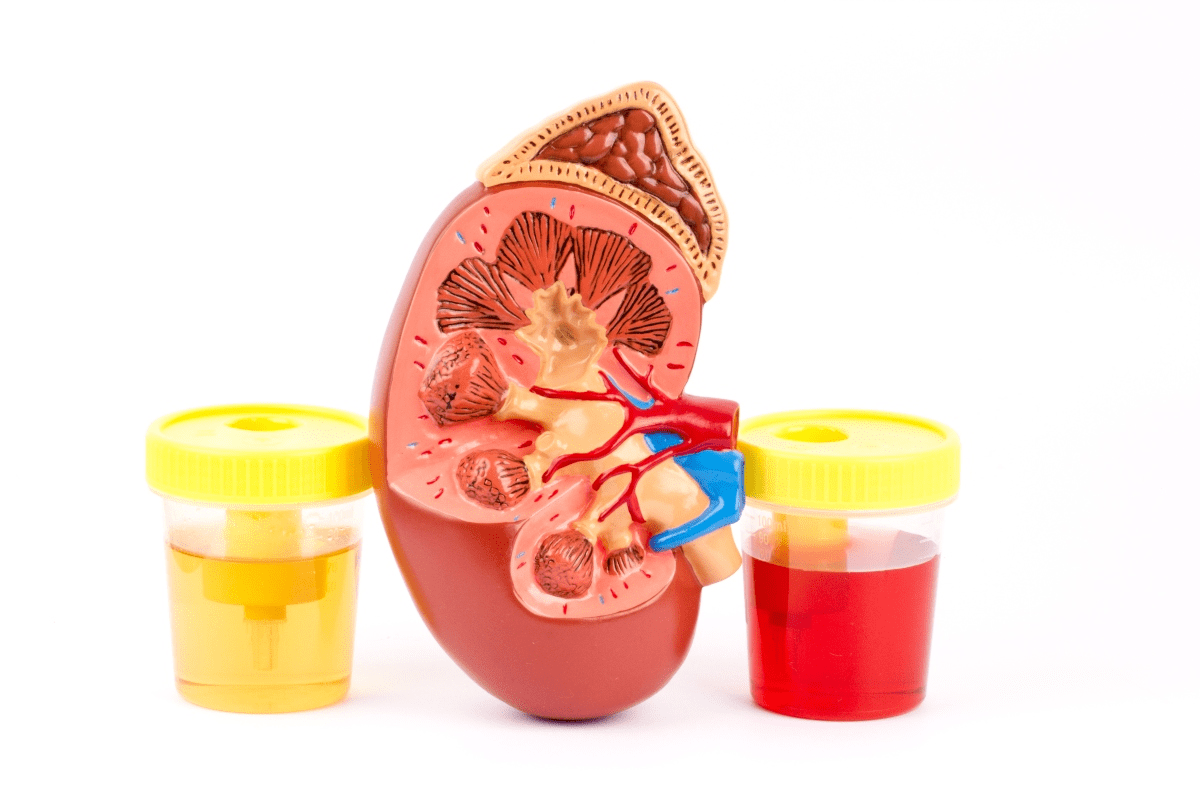
The primary tools for diagnosing an infection are laboratory analysis of the urine sample. It is imperative that a clean-catch midstream specimen is obtained to minimize contamination from skin flora.

For patients with uncomplicated cystitis, imaging is rarely necessary. However, for those with recurrent infections, symptoms of pyelonephritis, or suspected anatomical abnormalities, imaging is vital to visualize the urinary tract architecture.
In cases of recurrent infections, hematuria without infection, or suspected bladder pathology, a cystoscopy may be indicated. This procedure involves the insertion of a thin, flexible telescope through the urethra into the bladder.
Cystoscopy allows the urologist to directly inspect the mucosal lining of the urethra and bladder. It is invaluable for identifying anatomical causes of infection that do not show up on scans, such as urethral strictures, bladder diverticula, small bladder tumors, or interstitial cystitis. It also allows for the assessment of the bladder neck and prostate in men. This direct visualization completes the diagnostic picture, ensuring that no physical abnormality is perpetuating the infection cycle.
For patients whose infections are linked to voiding dysfunction, such as incomplete emptying or high-pressure voiding, urodynamic testing may be performed. This functional study measures how the bladder stores and releases urine. It assesses bladder pressure, flow rates, and muscle activity. Identifying functional issues like neurogenic bladder or detrusor sphincter dyssynergia is critical, as treating the infection without addressing the voiding dysfunction will likely result in failure.
When dealing with recurrent infections, the diagnostic strategy shifts from simply identifying the bacteria to identifying the reservoir. This may involve metabolic evaluations to check for stone-forming risks, hormonal profiling in post-menopausal women to assess atrophy, or specialized bacterial localization tests in men to rule out chronic bacterial prostatitis. The goal is to uncover the underlying cause behind the recurrence, not just the pathogen.
Part of the diagnostic process involves educating the patient on proper sample collection techniques. Contaminated samples can lead to false positives and unnecessary antibiotic use. Patients are instructed on hygiene measures prior to providing a sample to ensure the accuracy of the culture results. This partnership between patient and laboratory is essential for diagnostic precision.


Send us all your questions or requests, and our expert team will assist you.
While a dipstick test provides a rapid indication of infection by detecting markers like nitrites and white blood cells, it does not identify the specific bacteria causing the infection. A urine culture is necessary to grow the organism in the laboratory, identify it precisely, and test its susceptibility to various antibiotics. This ensures that the correct medication is prescribed and helps prevent antibiotic resistance.
A diagnostic cystoscopy is generally well-tolerated and is typically performed under local anesthesia using a numbing gel. Most patients describe the sensation as a mild discomfort or a strong urge to urinate rather than acute pain. The procedure is quick, usually lasting only a few minutes, and provides critical visual information about the bladder that cannot be obtained through other tests.
A clean catch urine sample is collected midstream after cleaning the genital area with a sterile wipe. This method is crucial because it flushes away bacteria that naturally reside on the skin and urethra, ensuring that the sample represents the urine inside the bladder. A standard sample without this preparation is likely to be contaminated with skin flora, leading to inaccurate diagnostic results.
A CT scan is generally not required for a simple bladder infection. It is indicated when there are signs of a severe kidney infection that is not responding to treatment, or if there is a suspicion of complications such as kidney stones, abscesses, or blockage in the urinary tract. It provides a detailed anatomical view to identify the root cause of the complication.
If you have symptoms like burning and urgency but a negative culture, it may indicate a condition other than a standard bacterial UTI. Possibilities include interstitial cystitis, sexually transmitted infections, vaginal infections, or inflammation caused by kidney stones. In such cases, further testing is required to determine the non-bacterial cause of the symptoms.

Hematuria, or the presence of blood in urine, is a condition that affects nearly one in five people globally. It can be a sign of

Hematuria, or blood in the urine, can be scary, even more so without pain or during non-menstrual periods. Seeing blood in your urine can be
Seeing a change in urine color can worry you. But knowing why it happens is the first step to feeling better. We’ll look at why

Seeing blood in urine can be scary, but knowing why it happens is key. Hematuria, the term for this, is quite common, affecting up to
Finding blood clots in urine without pain can be scary. It’s a sign that needs quick medical help. This issue, known as hematuria with visible
Seeing blood in your urine can be scary. But, knowing if it will go away by itself needs a doctor’s check-up. Hematuria, the term for

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)