Urology treats urinary tract diseases in all genders and male reproductive issues, covering the kidneys, bladder, prostate, urethra, from infections to complex cancers.
Send us all your questions or requests, and our expert team will assist you.
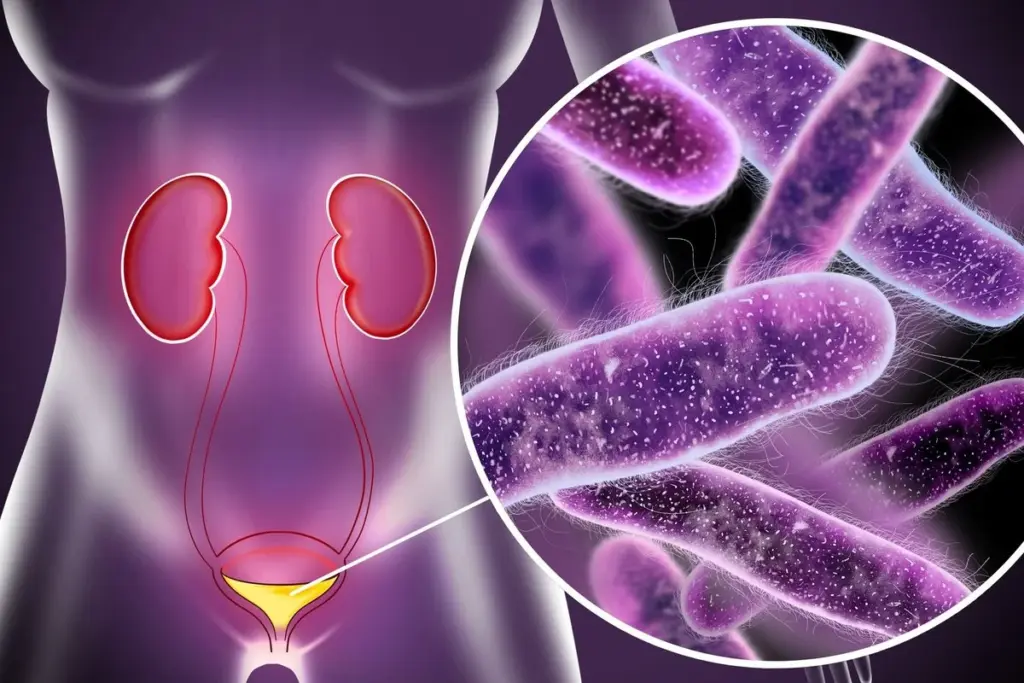
A Urinary Tract Infection is clinically defined as the presence of microbial pathogens within the urinary tract that induces an inflammatory response in the host. While bacteria are the most common etiological agents, fungi and viruses can also be causative organisms in specific patient populations. The infection can manifest anywhere along the urological axis, from the urethral meatus to the renal parenchyma. This anatomical distinction is critical for clinical management, as it dictates the severity of the condition, the potential for complications, and the required aggressiveness of the therapeutic regimen.
To provide a comprehensive overview, it is essential to categorize infections based on their anatomical location. The urinary tract is clinically divided into the lower and upper tracts, each presenting with distinct pathophysiological characteristics.
The etiology of infections is predominantly bacterial. Escherichia coli, a bacterium that normally resides in the intestinal tract, is responsible for the vast majority of community-acquired infections. These uropathogenic strains possess specific virulence factors, such as fimbriae, which allow them to firmly attach to the receptors on the bladder wall, resisting the mechanical flushing action of urination.
Beyond E. coli, other pathogens such as Klebsiella pneumoniae, Proteus mirabilis, and Enterococcus faecalis are frequently isolated, particularly in patients with structural abnormalities or those who have been hospitalized. In complex cases, multi-drug resistant organisms may be identified, necessitating advanced microbiological profiling. A rigorous definition of significant bacteriuria is employed to distinguish between mere contamination and true infection based on colony-forming units and the presence of pyuria.
Urinary Tract Infections represent one of the most prevalent infectious diseases worldwide, affecting millions of individuals annually. The epidemiology exhibits a marked gender disparity. Women are significantly more prone to infections due to anatomical factors, specifically the shorter length of the female urethra and its proximity to the anal verge, which facilitates the migration of fecal flora. It is estimated that a substantial proportion of women will experience at least one infection in their lifetime.
In contrast, infections in young men are relatively rare and often prompt an investigation for anatomical anomalies. However, the incidence in men rises with age, often correlated with prostatic enlargement which causes urinary stasis. In the pediatric population, infections can be a sentinel sign of congenital defects such as vesicoureteral reflux. Understanding these demographic nuances allows the medical team to tailor the diagnostic overview, ensuring that underlying causes are identified rather than simply treating the symptomatic infection.
A pivotal distinction in the clinical definition is the categorization of infections as uncomplicated or complicated. This classification guides the duration and type of therapy.

The burden of Urinary Tract Infections extends beyond physical symptoms. Recurrent infections can lead to significant psychological distress, anxiety regarding sexual activity, and disruption of daily routines. The fear of an impending episode can lead to maladaptive behaviors, such as excessive fluid restriction or avoidance of social situations. In the elderly, the confusion and lethargy associated with infections can lead to falls, fractures, and loss of independence.
Therefore, the operational definition of care involves a holistic assessment of the patient’s well-being. It is not sufficient to merely sterilize the urine; the goal is to restore the patient’s confidence and prevent the infection from dominating their life. This requires a patient-centered approach that educates the individual on the nature of their condition and empowers them with strategies for prevention.

Send us all your questions or requests, and our expert team will assist you.
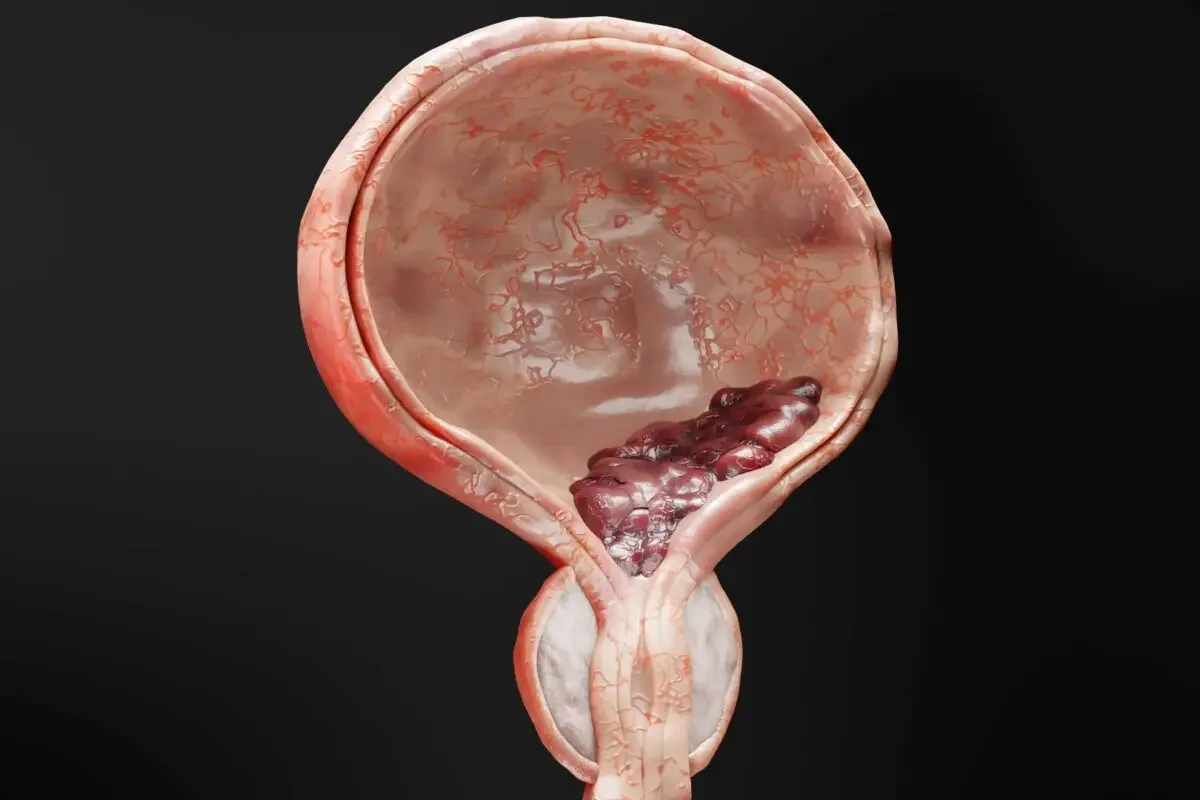
A lower urinary tract infection, commonly known as cystitis, is confined to the bladder and urethra, causing local symptoms like burning and frequency. An upper urinary tract infection, or pyelonephritis, involves the kidneys and ureters and is generally more severe, often accompanied by systemic symptoms such as high fever, chills, flank pain, and nausea, requiring more aggressive treatment to prevent kidney damage.
Women have a distinct anatomical predisposition due to the significantly shorter length of the female urethra compared to the male urethra. This shorter distance allows bacteria from the external environment to travel more easily to the bladder. Additionally, the urethral opening in women is located in closer proximity to the rectum, which serves as a natural reservoir for bacteria like E. coli.
A complicated infection is defined as an infection occurring in a patient with a structural or functional abnormality of the urinary tract, or in the presence of an underlying disease that interferes with host defense mechanisms. This includes infections in men, pregnant women, patients with kidney stones, diabetes, immunosuppression, or indwelling catheters, necessitating a more comprehensive treatment approach.
Yes, the urinary tract has several innate defense mechanisms. The primary defense is the regular voiding of urine, which mechanically flushes out bacteria. Additionally, the urine itself has specific chemical properties like acidity that inhibit bacterial growth. The lining of the bladder also secretes protective proteins and has an immune response layer that prevents bacteria from adhering to the bladder wall.
No, the presence of bacteria in the urine, known as bacteriuria, does not always constitute an active infection. In many cases, particularly in the elderly or those with catheters, bacteria may exist in the bladder without causing symptoms or tissue invasion. This is called asymptomatic bacteriuria and generally does not require antibiotic treatment unless the patient is pregnant or undergoing a urological procedure.

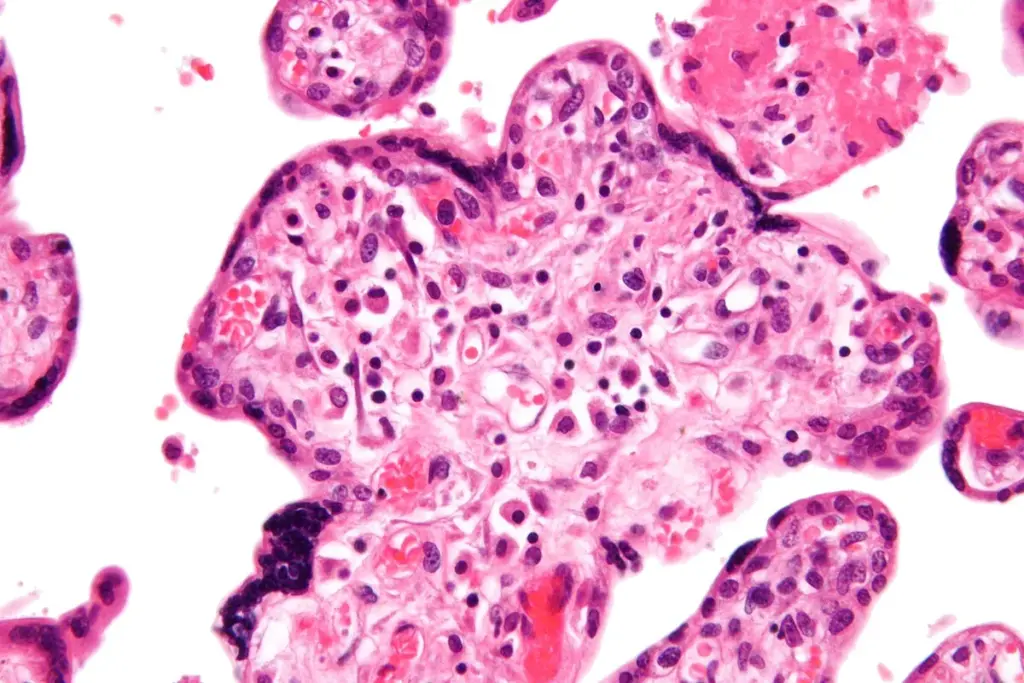
Seeing blood in your urine can be scary. But knowing why it happens is the first step to getting better. Blood in urine, or hematuria,

Hematuria, or blood in urine, is common. It means red blood cells are in your urine. This can be a sign of many health issues.

Our bodies send important messages, and light pink urine color is a key way they do it. When urine color changes, it can mean a

Blood clots in urine, also known as hematuria, can point to several problems in the urinary system. Finding blood clots in your urine can be

Seeing blood in urine can be scary, but knowing why it happens is key. Hematuria, the term for this, is quite common, affecting up to

Hematuria, or blood in the urine, can be scary, even more so without pain or during non-menstrual periods. Seeing blood in your urine can be

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)