Urology treats urinary tract diseases in all genders and male reproductive issues, covering the kidneys, bladder, prostate, urethra, from infections to complex cancers.
Send us all your questions or requests, and our expert team will assist you.

The treatment of Urinary Tract Infections at Liv Hospital is guided by the principles of antimicrobial stewardship, personalized medicine, and comprehensive supportive care. The primary objective is to eradicate the pathogenic organism, alleviate symptoms, and prevent the ascension of the infection to the kidneys. However, the management strategy extends beyond the immediate prescription. It involves selecting the appropriate therapeutic agent based on local resistance patterns, patient history, and the specific classification of the infection. The medical team emphasizes compliance and follow-through to ensure complete resolution and minimize the risk of recurrence or the development of resistant bacterial strains.
Treatment protocols are distinct for uncomplicated cystitis, complicated infections, and pyelonephritis. Each requires a tailored approach regarding the choice of medication, the duration of therapy, and the level of monitoring required.
Antibiotics remain the cornerstone of treatment. For uncomplicated cystitis in women, short-course regimens are the standard of care. First-line agents often include nitrofurantoin, trimethoprim-sulfamethoxazole, or fosfomycin. These drugs are chosen for their efficacy in concentrating in the urine and their minimal impact on the body’s natural flora.
For complicated infections or pyelonephritis, the treatment regimen is more aggressive. Fluoroquinolones or cephalosporins are frequently utilized, often for a duration of 7 to 14 days. In cases of severe systemic illness, intravenous antibiotics may be initiated in a hospital setting until the patient is stable enough to transition to oral medication. The choice of antibiotic is always refined once culture sensitivity results are available, allowing for de-escalation to the most narrow-spectrum agent that is effective, thereby reducing collateral damage to the microbiome.

While antibiotics target the bacteria, immediate relief of symptoms is a priority for patient comfort. Urinary analgesics, such as phenazopyridine, may be prescribed for a short period to anesthetize the mucosal lining of the urinary tract, effectively reducing burning and urgency. However, patients are advised that these medications only mask symptoms and do not cure the infection.
Hydration is a critical component of supportive care. Increasing fluid intake helps to mechanically flush bacteria and inflammatory debris from the bladder. Patients are encouraged to void frequently and completely. In cases of severe pain or fever, antipyretics and NSAIDs are used to manage systemic symptoms.
For patients suffering from recurrent infections, defined as three or more episodes in a year, the treatment strategy shifts from episodic care to long-term prevention.

If diagnostic testing reveals a structural or functional cause for the infection, medical therapy alone is often insufficient. Surgical or procedural intervention may be required to resolve the root cause.
Liv Hospital is acutely aware of the global threat of antibiotic resistance. The urology department adheres to strict protocols to avoid the overuse of broad-spectrum antibiotics. Treatment decisions are data-driven, relying on local antibiograms which are charts showing local bacterial resistance patterns. In cases of multi-drug resistant organisms, infectious disease specialists are consulted to design complex combination therapies or utilize intravenous agents in an outpatient or inpatient setting. This vigilant approach ensures that effective treatment options remain available for future needs.
A crucial aspect of treatment is ensuring patient adherence to the prescribed regimen. Patients are educated on the importance of completing the full course of antibiotics, even if symptoms resolve early. Stopping treatment prematurely can lead to the survival of resistant bacteria and a more severe relapse. Clear instructions on medication timing and potential side effects are provided to maximize compliance.

Send us all your questions or requests, and our expert team will assist you.
Feeling better usually indicates that the bacterial load has been reduced, but not necessarily eliminated. Stopping antibiotics prematurely allows the strongest, most resistant bacteria to survive and multiply. This can lead to a relapse of the infection that is much harder to treat because the surviving bacteria are now resistant to the medication. Completing the full course ensures eradication.
Urinary analgesics are medications designed to numb the lining of the urinary tract. They provide rapid relief from the burning, pain, and urgency associated with an infection. However, they do not kill bacteria or cure the infection. They are used solely for symptom management during the first day or two while waiting for the antibiotics to take effect.
After menopause, the lack of estrogen causes the vaginal tissue to thin and the pH to rise, killing off healthy bacteria. Vaginal estrogen cream restores the health of the tissue and lowers the pH, allowing beneficial bacteria to return. These good bacteria create a natural barrier that prevents harmful bacteria like E. coli from growing and causing infections.
Hospitalization is typically required for severe upper tract infections where the patient exhibits signs of sepsis, such as high fever, rapid heart rate, or low blood pressure. It is also necessary if the patient is unable to keep down oral medications due to vomiting, is pregnant, or has complicating factors like a kidney stone obstruction requiring urgent drainage.
Yes, several non-antibiotic strategies are effective. These include taking D-mannose supplements, cranberry extracts containing proanthocyanidins, and probiotics to maintain healthy flora. Lifestyle changes like increased hydration and localized estrogen therapy are also key non-antibiotic preventive measures.

Finding blood clots in urine without pain can be scary. It’s a sign that needs quick medical help. This issue, known as hematuria with visible
Hematuria, or the presence of blood clots in urine, is a condition that can be alarming. It affects a significant portion of the adult population.

Hematuria, or blood in the urine, can be scary, even more so without pain or during non-menstrual periods. Seeing blood in your urine can be
Hematuria, or the presence of blood in urine, is a condition that affects nearly one in five people globally. It can be a sign of
Seeing occult blood in your urine test results can be scary. But knowing what it means is the first step to better health. We’re here
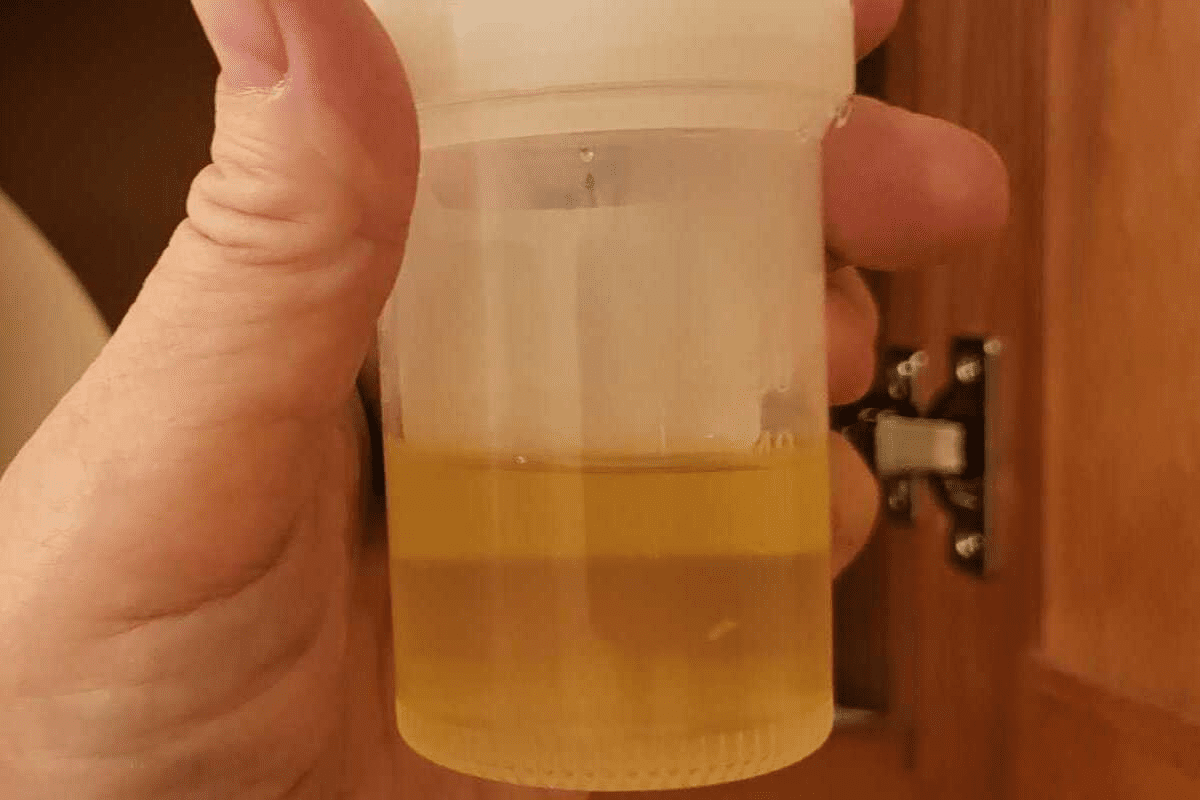
Seeing a change in urine color can worry you. But knowing why it happens is the first step to feeling better. We’ll look at why

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)