Gastroenterology covers the digestive system. It focuses on diagnosing, treating, and managing conditions of the stomach, intestines, liver, and pancreas.
Send us all your questions or requests, and our expert team will assist you.

Cirrhosis represents the advanced, late-stage consequence of prolonged liver injury, characterized by the irreversible replacement of healthy, functioning liver tissue with non-functional scar tissue, a process known as fibrosis. In a physiologically healthy state, the liver possesses a remarkable and unique capacity to regenerate itself after damage. When liver cells (hepatocytes) are injured by toxins, viruses, or metabolic stress, they can usually repair the damage and restore normal function. However, when the injury is chronic, persistent, and repetitive over many years or decades, this repair process becomes dysregulated and pathological.
The liver attempts to wall off the injured areas, leading to the accumulation of excessive connective tissue. As this scar tissue builds up, it creates fibrous bands that encircle and isolate nodules of regenerating liver cells. This creates the classic “nodular” appearance of a cirrhotic liver. This architectural distortion fundamentally disrupts the liver’s microscopic structure and its macroscopic blood flow. The scar tissue compresses the liver’s internal vascular system, leading to high blood pressure within the liver (portal hypertension) and impairing the organ’s ability to perform its critical metabolic duties, such as detoxifying the blood, synthesizing vital clotting proteins, and regulating energy storage. At Liv Hospital, we approach cirrhosis not as a static end-point but as a dynamic clinical condition where precise management can stabilize the disease, preserve remaining function, and prevent life-threatening decompensation.
The transition from a healthy liver to a cirrhotic liver is a complex, gradual process driven by chronic inflammation and cellular transformation.

From a clinical and prognostic perspective, cirrhosis is categorized into two distinct functional stages. Understanding this distinction is crucial for management at Liv Hospital.

Cirrhosis is not a disease in itself but the result of various chronic liver injuries.
The most critical mechanical consequence of the architectural distortion in cirrhosis is the development of portal hypertension.

Send us all your questions or requests, and our expert team will assist you.
No, they are different concepts. Cirrhosis refers to the physical scarring of the liver tissue. Liver failure refers to the loss of liver function. A person can have cirrhosis (compensated) and still have a functioning liver, but decompensated cirrhosis often leads to liver failure.
The liver has immense regenerative power, and early fibrosis is reversible. However, once advanced cirrhosis with thick scarring and nodule formation is established, it is generally considered irreversible. Treatment focuses on preserving the remaining function rather than reversing the scar.
No. While alcohol is a major risk factor, only about 10 to 20 percent of heavy drinkers develop cirrhosis. Genetics, diet, and other factors like co-existing viral hepatitis play a significant role in susceptibility.
Fibrosis is the process of scar tissue formation. It is staged from F0 (no scarring) to F4. Cirrhosis is effectively stage F4 fibrosis, representing the most severe and extensive form of scarring that distorts the liver structure.
It is a serious, life-limiting condition if it progresses to the decompensated stage. However, patients with compensated cirrhosis who manage the underlying cause (e.g., stop drinking, cure Hepatitis C) can live for decades without reducing their life expectancy significantly.

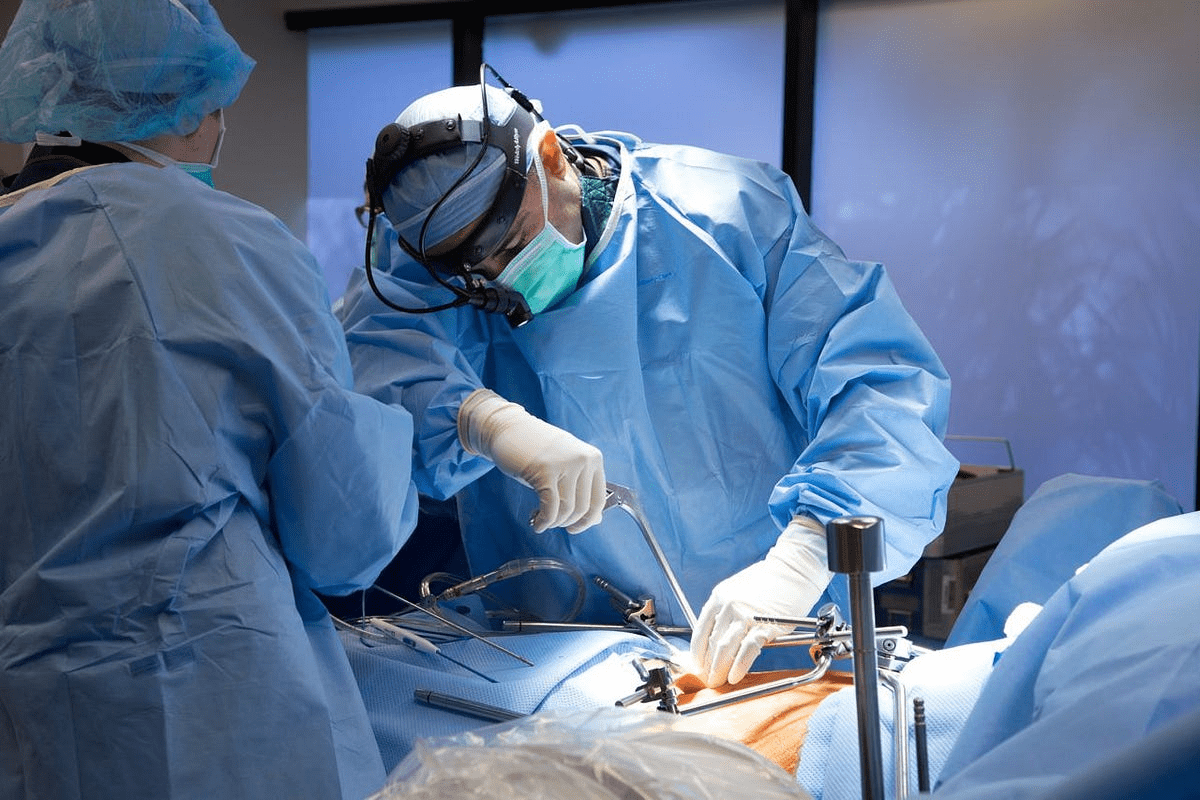
Cholangiocarcinoma is rare and aggressive; surgery is the only curative option when tumors are resectable, but only a minority qualify at diagnosis, so expert evaluation

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)