Gastroenterology covers the digestive system. It focuses on diagnosing, treating, and managing conditions of the stomach, intestines, liver, and pancreas.
Send us all your questions or requests, and our expert team will assist you.

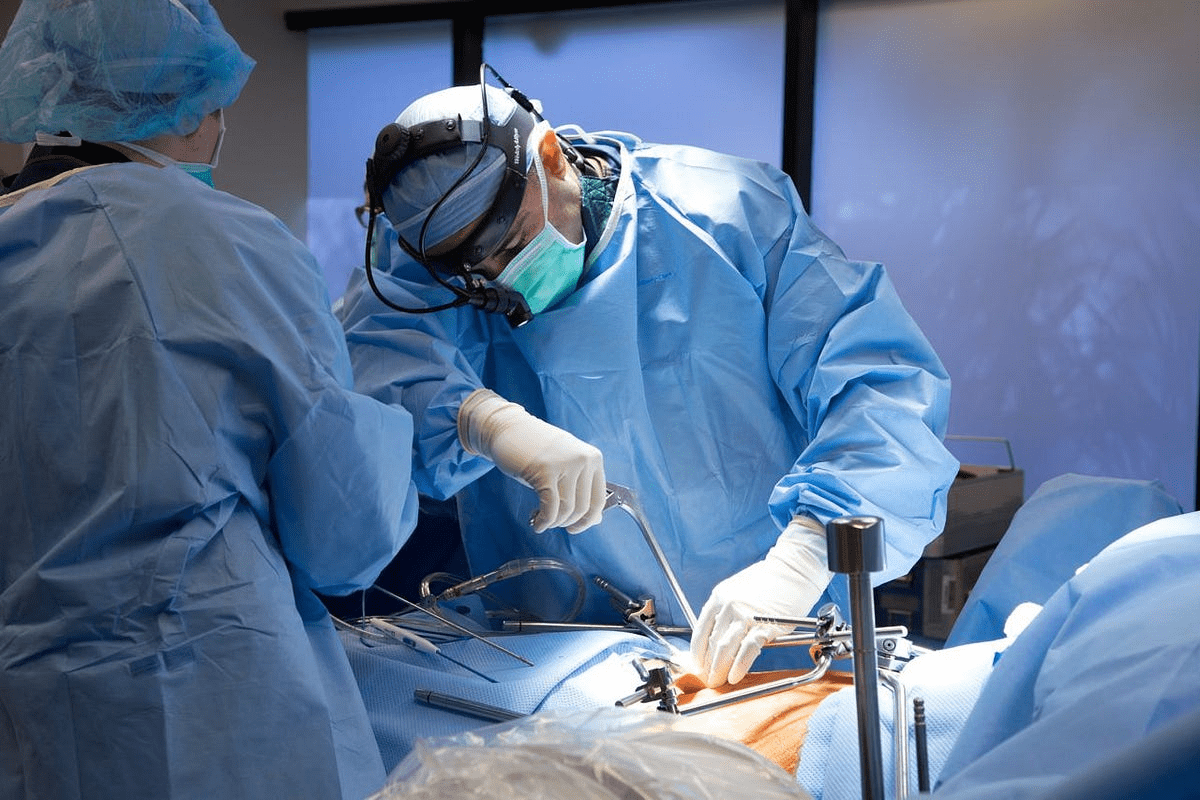
Diagnosing cirrhosis involves a multi-modal approach aimed at confirming the presence of advanced fibrosis, assessing the remaining synthetic function of the liver, and screening for the dangerous complications of portal hypertension. Because the disease can be asymptomatic for decades, incidental findings on routine blood work or imaging often trigger the initial investigation. At Liv Hospital, we utilize a comprehensive diagnostic pathway that combines non-invasive elastography, advanced imaging, and functional serology to accurately stage the disease without defaulting to invasive biopsies unless absolutely necessary.

Routine blood tests provide the foundational data for assessing liver injury and function.

Modern hepatology has moved away from biopsy as the sole method of diagnosis, favoring non-invasive technologies.
Imaging is crucial for visualizing the morphology of the liver and detecting complications.


Prognostic models are calculated to determine the stage of disease and transplant priority.

Send us all your questions or requests, and our expert team will assist you.
No, FibroScan is a completely painless, non-invasive procedure. It feels like a gentle flicker or tap on the skin over the liver. It takes about 10 to 15 minutes and requires no sedation.
Varices (swollen veins) in the esophagus cause no pain or symptoms until they burst. An endoscopy is the only way to see them before a catastrophic bleed occurs, allowing doctors to treat them preventatively.
The MELD score is a statistical number that tells doctors how urgently you need a liver transplant. It reflects how likely a patient is to survive the next three months without a new liver. It is recalculated regularly as lab values change.
Blood tests can strongly suggest cirrhosis (e.g., low platelets combined with high INR), but they are not definitive proof on their own. They must be combined with imaging (like FibroScan or Ultrasound) or biopsy for a confirmed diagnosis.
Surveillance is lifelong. Typically, you will need blood tests and a liver ultrasound (to screen for cancer) every 6 months. Endoscopy frequency depends on whether varices are found and how large they are.

Cholangiocarcinoma is rare and aggressive; surgery is the only curative option when tumors are resectable, but only a minority qualify at diagnosis, so expert evaluation

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)