Last Updated on October 21, 2025 by mcelik
Hematology is the study of blood disorders and diseases. It’s a key part of medicine that affects millions globally. Did you know over 1 million people in the U.S. get diagnosed with a hematological disorder yearly?
We’ll explore the main blood diseases, their impact on health, and why hematology is crucial today.
Exploring hematology, we’ll check out the various conditions it covers. We’ll see why they matter in healthcare.
Key Takeaways
- Understanding hematology is key for diagnosing and treating blood-related diseases.
- Hematological disorders can greatly affect a person’s life quality.
- There are many types of blood diseases and disorders, each unique.
- Early detection and treatment of hematological disorders can lead to better outcomes.
- Hematology is always growing, with new research and treatments coming up.
The Science of Hematology
Hematology is the study of blood and its disorders. It’s a key part of modern medicine. This field helps diagnose, treat, and manage blood-related issues.
Definition and Scope of Hematological Medicine
Hematological medicine focuses on blood and its disorders. It also looks at organs that make blood. This field covers many conditions, like anemia and blood cancers.
Understanding hematological medicine is vital. It helps both doctors and patients. It’s important for improving life quality.
The Composition and Function of Blood
Blood is made up of cells and plasma. It carries oxygen, fights infections, and helps blood clot. The main parts are red blood cells, white blood cells, and platelets.
The way blood works is linked to health. Problems with blood can cause serious issues. That’s why hematology is key in diagnosing and treating these problems.
The Hematopoietic System
The hematopoietic system makes blood cells. It includes bone marrow, where stem cells turn into different blood cells. Knowing this system helps us understand blood disorders and how to treat them.
The hematopoietic system is vital for healthy blood. Problems here can cause many disorders. Studying this system is important in hematology.
Common Blood Disorders and Their Classification
Understanding blood disorders is key to knowing their causes and effects. They can be grouped by their origin, severity, and the blood parts they affect.
Inherited vs. Acquired Blood Diseases
Blood diseases can come from genes or develop over time. Inherited blood disorders are passed down through genes. Acquired blood diseases happen due to environment, lifestyle, or infections.
- Inherited conditions include sickle cell anemia and hemophilia.
- Acquired conditions include iron deficiency anemia and some leukemias.
Knowing if a blood disorder is inherited or acquired helps choose the right treatment.
Benign vs. Malignant Hematological Conditions

Blood disorders can also be benign or malignant. Benign hematological conditions are usually not serious and may not need aggressive treatment. Malignant hematological conditions are cancers that can be deadly if not treated quickly.
- Benign conditions include some anemias and thrombocytopenias.
- Malignant conditions include leukemia, lymphoma, and multiple myeloma.
Knowing if a condition is benign or malignant is important for treatment and outlook.
Impact on Global Health
Blood disorders affect millions worldwide, impacting global health. Their prevalence changes based on where you are and who you are.
The World Health Organization (WHO) says anemia affects over 1.6 billion people. Leukemia and lymphoma also add to the disease burden.
Grasping blood disorder classification and impact is key for better public health and patient care.
Red Blood Cell Disorders
Red blood cell disorders affect how red blood cells are made, work, and last. They can cause health problems, from mild to serious. We’ll look at common ones like anemia, polycythemia, and hemoglobinopathies.
Anemia: Types, Causes, and Symptoms
Anemia means not enough red blood cells or poor quality ones. This makes it hard for tissues to get enough oxygen. It can happen for many reasons, like not enough iron or vitamins, chronic diseases, or genetic issues.
Symptoms include feeling very tired, weak, and pale. You might also have trouble breathing.
There are many types of anemia. Iron deficiency anemia is the most common worldwide. It’s often because of not eating enough iron or losing blood too much. Vitamin deficiency anemia, like pernicious anemia, happens when you don’t get enough vitamin B12.
| Type of Anemia | Causes | Symptoms |
| Iron Deficiency Anemia | Inadequate iron intake, chronic blood loss | Fatigue, weakness, pale skin |
| Vitamin Deficiency Anemia | Lack of vitamin B12 or folate | Fatigue, weakness, neurological changes |
Polycythemia and Erythrocytosis
Polycythemia, or erythrocytosis, means too many red blood cells. This can make blood thicker and cause heart problems. Primary polycythemia, like polycythemia vera, is a type of cancer that makes too many red blood cells.
Secondary polycythemia happens because of things like high altitude or heart disease. Symptoms include headaches, dizziness, and itching, often after taking a hot shower.
Hemoglobinopathies
Hemoglobinopathies are genetic problems with hemoglobin, a key protein in red blood cells. Sickle cell disease and thalassemia are common ones. Sickle cell disease makes red blood cells look like sickles, causing crises and other issues.
“Hemoglobinopathies represent a significant global health burden, requiring extensive management strategies to improve patient outcomes.” –
A leading hematologist
Thalassemia means not enough hemoglobin chains, leading to anemia and other problems. Treating hemoglobinopathies often includes blood transfusions, iron chelation therapy, and supportive care.
Knowing about these disorders is key to helping people with them. We’re working hard to improve diagnosis and treatment, giving hope for better lives.
White Blood Cell Disorders
White blood cell disorders are complex conditions that affect the immune system. They can cause mild infections to serious diseases. It’s important to understand these disorders to diagnose and treat them.
Neutropenia and Neutrophilia
Neutropenia is when you have too few neutrophils, a key white blood cell. Severe neutropenia makes you more likely to get infections. It often happens in people getting chemotherapy or with certain bone marrow issues. Neutrophilia is when you have too many neutrophils, usually because of an infection or stress.
Both conditions need careful attention to avoid problems. For neutropenia, patients might need to stay isolated to avoid infections. For neutrophilia, treating the cause is key.
Lymphocytopenia and Lymphocytosis
Lymphocytopenia means you have too few lymphocytes, another important white blood cell. It can be caused by viruses, HIV/AIDS, or some medicines. Lymphocytosis is when you have too many lymphocytes, often due to infections, autoimmune diseases, or cancers.
Diagnosing these conditions involves blood tests and sometimes bone marrow exams. This helps find the cause and the right treatment.
Leukocyte Adhesion Deficiencies
Leukocyte adhesion deficiencies (LAD) are rare genetic disorders. They make it hard for white blood cells to fight infections. LAD can cause severe infections and slow healing. It often needs aggressive treatment, like antibiotics and sometimes bone marrow transplants.
Myelodysplastic Syndromes
Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. They can lead to bone marrow failure. MDS can turn into acute myeloid leukemia (AML). Symptoms include anemia, neutropenia, or thrombocytopenia. Treatment depends on the risk level and may include supportive care, immunosuppressive therapy, or stem cell transplants.
Knowing about these white blood cell disorders is key to good care and better patient outcomes. New diagnostic and treatment methods are helping manage these complex conditions.
Platelet and Bleeding Disorders
Platelet and bleeding disorders are complex conditions. They affect how the body forms clots and stops bleeding. These disorders can be mild or severe and have many causes. These include genetics, environment, and other health issues.
Thrombocytopenia: Causes and Complications
Thrombocytopenia is when you have too few platelets in your blood. This makes it hard to form blood clots, leading to a lot of bleeding. It can be caused by many things, like bone marrow problems, certain medicines, and autoimmune diseases.
Complications of thrombocytopenia can be serious. They include bleeding easily, bruising, and in bad cases, life-threatening bleeding. Treating thrombocytopenia usually means fixing the cause. It might also involve medicines to help make more platelets or stop them from being destroyed.
Thrombocytosis and Essential Thrombocythemia
Thrombocytosis is when you have too many platelets. It can be a reaction to something else, like an infection. But it can also mean you have a rare disorder called essential thrombocythemia.
Essential thrombocythemia is a rare condition where your bone marrow makes too many platelets. This raises your risk of blood clots. To manage it, doctors might use medicines to lower platelet count and prevent clots.
Platelet Function Disorders
Platelet function disorders happen when platelets don’t work right. This makes it hard to clot blood. These disorders can be inherited or get worse over time. They can make you more likely to bleed.
- Diagnosis often involves tests to check how platelets work.
- Treatment might include medicines that help platelets work better or lower bleeding risk.
Immune Thrombocytopenic Purpura
Immune thrombocytopenic purpura (ITP) is an autoimmune disease. It happens when your immune system attacks and destroys platelets. This can lead to a low platelet count and more bleeding.
ITP treatment might include corticosteroids to calm down your immune system. It might also include intravenous immunoglobulin (IVIG) to quickly raise platelet count. In some cases, removing the spleen might be needed.
Coagulation and Clotting Disorders
The body’s coagulation system is very precise. Disorders in this system can cause mild bleeding or severe blood clots. These conditions affect the balance between bleeding and clotting.
Hemophilia A and B
Hemophilia A and B are genetic disorders. They are caused by a lack of clotting factors VIII and IX. These conditions mainly affect males and can cause long-lasting bleeding in joints and muscles.
Key aspects of hemophilia include:
- Genetic inheritance pattern
- Severity based on factor levels
- Management through factor replacement therapy
Von Willebrand Disease
Von Willebrand disease is the most common hereditary coagulation abnormality. It is caused by a lack or dysfunction of von Willebrand factor (VWF). VWF is important for platelet adhesion and protecting factor VIII.
Symptoms can vary widely and may include easy bruising, nosebleeds, and heavy menstrual bleeding. Diagnosis involves laboratory tests to assess VWF levels and function.
Thrombophilia and Hypercoagulable States
Thrombophilia refers to conditions that increase the risk of thrombosis. This is due to an imbalance in the coagulation system, favoring clot formation. It can be hereditary or acquired.
Common causes include:
- Genetic mutations such as Factor V Leiden
- Antiphospholipid syndrome
- Acquired conditions like cancer or immobilization
Disseminated Intravascular Coagulation
Disseminated intravascular coagulation (DIC) is a serious condition. It is characterized by both widespread clotting and bleeding in the vascular system. It is often associated with severe underlying conditions such as sepsis or trauma.
Management of DIC involves:
- Treatment of the underlying cause
- Supportive care to manage bleeding or thrombosis
Understanding Blood Disorders: Causes and Risk Factors
It’s important to know the causes and risk factors of blood disorders. This knowledge helps in early diagnosis and treatment. Blood disorders affect how blood cells work.
Genetic and Hereditary Factors
Genetics play a big role in many blood disorders. For example, sickle cell anemia and thalassemia are inherited. This means you need two bad genes to have the disease.
Other diseases like Hemophilia A and B are linked to the X chromosome. This makes them more common in males. Knowing the genetic causes helps with family planning.
Environmental and Lifestyle Influences
Our environment and lifestyle choices can affect our risk of blood disorders. Exposure to toxins and chemicals can harm our bone marrow. This can lead to various blood-related problems.
Our diet and infections can also play a role. A bad diet can cause anemia. Some infections can lead to autoimmune hemolytic anemia.
Age and Gender-Related Risk Factors
Age and gender are important risk factors for blood disorders. For example, myelodysplastic syndromes are more common in older adults. Acute lymphoblastic leukemia often affects children.
Gender also matters. Some disorders are more common in men or women. For instance, iron deficiency anemia is more common in women of childbearing age.
Autoimmune Mechanisms
Autoimmune mechanisms are key in some blood disorders. In autoimmune hemolytic anemia, the immune system attacks the body’s red blood cells. This marks them for destruction.
In immune thrombocytopenic purpura, autoantibodies destroy platelets. This can lead to serious bleeding. Understanding these processes is important for finding effective treatments.
Hematologic Malignancies
Cancers of the blood and lymphatic system are known as hematologic malignancies. They are challenging to diagnose and treat. These cancers can be divided into several types, each with its own characteristics and symptoms.
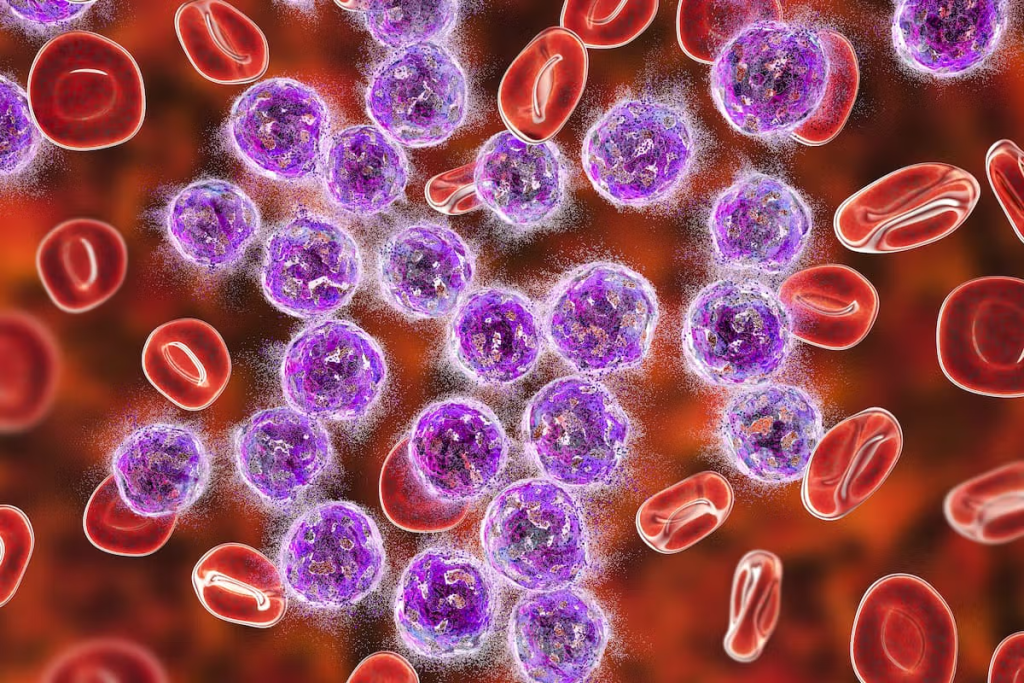
Leukemia: Blood Cell Cancer
Leukemia affects the blood and bone marrow, causing an abnormal increase in white blood cells. It has different subtypes, like ALL, AML, CLL, and CML. The symptoms and treatment depend on the type and the patient’s health.
Diagnosis of leukemia involves blood tests, bone marrow aspiration, and genetic testing. Treatment may include chemotherapy, targeted therapy, or stem cell transplantation.
Lymphoma: Cancer of the Lymphatic System
Lymphoma starts in the lymphatic system. It has two main types: Hodgkin lymphoma and non-Hodgkin lymphoma (NHL). NHL is more common. Symptoms include swollen lymph nodes, fever, and weight loss.
The diagnosis of lymphoma uses imaging studies and biopsies. Treatment includes chemotherapy, radiation, and immunotherapy.
Multiple Myeloma and Plasma Cell Disorders
Multiple myeloma is a cancer of plasma cells in the bone marrow. It causes anemia, bone pain, and infections. Diagnosis involves finding abnormal proteins in blood or urine and examining bone marrow.
Treatment for multiple myeloma includes targeted therapies, chemotherapy, and stem cell transplantation. Managing symptoms and preventing complications are also key.
Myeloproliferative Neoplasms
Myeloproliferative neoplasms (MPNs) are diseases with excessive blood cell production. Common types are polycythemia vera, essential thrombocythemia, and primary myelofibrosis. MPNs raise the risk of blood clots and can lead to more severe conditions.
The management of MPNs aims to prevent complications. This is done through medications and, in some cases, procedures like phlebotomy.
Rare and Hereditary Blood Diseases
Rare and hereditary blood diseases are complex and challenging to diagnose and treat. They are caused by genetic issues and affect many people worldwide. Understanding their causes and symptoms is key.
Fanconi Anemia
Fanconi anemia is a rare genetic disorder. It causes bone marrow failure, birth defects, and a higher risk of cancer. It’s inherited in an autosomal recessive pattern, meaning both parents must carry the mutated gene.
Symptoms include anemia, infections, and physical abnormalities like short stature and skeletal malformations. Diagnosis involves genetic testing and bone marrow exams. Treatment includes hematopoietic stem cell transplantation and supportive care to manage symptoms.
Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired disease. It causes red blood cell destruction, bone marrow failure, and blood clotting. It’s caused by mutations in the PIGA gene, leading to protein deficiencies on blood cells.
Symptoms include hemoglobinuria, fatigue, and abdominal pain. Diagnosis uses flow cytometry to detect protein deficiencies. Treatment involves eculizumab and supportive care to manage complications.
Gaucher Disease and Other Storage Disorders
Gaucher disease is a genetic disorder caused by a deficiency of the enzyme glucocerebrosidase. This leads to the buildup of glucocerebroside in cells and organs. Symptoms include anemia, fatigue, and bone pain.
- Enzyme replacement therapy (ERT) is a mainstay of treatment, helping to manage symptoms and improve quality of life.
- Substrate reduction therapy is another treatment approach that can help reduce the accumulation of glucocerebroside.
Hereditary Spherocytosis
Hereditary spherocytosis is a disorder where red blood cells are abnormal and prone to premature destruction. Symptoms include anemia, jaundice, and splenomegaly. Diagnosis is made through blood smears and family history.
Treatment often involves splenectomy, which can significantly improve or even cure the condition by removing the spleen. Other management strategies include folate supplementation to support red blood cell production.
Diagnosis of Hematological Disorders
Diagnosing blood disorders needs a detailed approach. We use many tests and evaluations to find and treat these conditions. This method helps us accurately identify and manage blood disorders.
Complete Blood Count and Blood Smears
A complete blood count (CBC) is key in hematology. It shows the makeup of blood, like red and white cells, and platelets. It helps spot issues like anemia, infections, and leukemia.
A blood smear is also important. It looks at blood under a microscope to find cell problems.
Bone Marrow Aspiration and Biopsy
Bone marrow aspiration and biopsy take samples from bone marrow. These tests are key for diagnosing diseases like leukemia and lymphoma. They give insights into blood cell production and function.
Genetic and Molecular Testing
Genetic and molecular testing are essential in diagnosing blood disorders. Tests like PCR and FISH find genetic mutations. This helps doctors diagnose and plan treatments more accurately.
Imaging Studies in Hematology
Imaging studies like X-rays and CT scans help diagnose and track blood disorders. They show how far the disease has spread and how well treatments are working. They’re great for spotting conditions like lymphoma and multiple myeloma.
Treatment Approaches for Blood Disorders
Managing blood disorders needs a mix of treatments. Each treatment is chosen based on the condition, its severity, and the patient’s health. This ensures the best care for each person.
Medication Therapies and Targeted Treatments
Medicine is key in treating many blood disorders. For example, anticoagulant medications stop blood clots. Antiplatelet drugs prevent platelets from sticking together. Tyrosine kinase inhibitors have changed how we treat some blood cancers.
- Immunosuppressive drugs for conditions like aplastic anemia
- Iron chelators for managing iron overload in transfusion-dependent patients
- Growth factors to stimulate the production of blood cells
Blood Transfusions and Blood Products
Blood transfusions are vital for treating many blood disorders. Red blood cell transfusions increase healthy red blood cells. Platelet transfusions help prevent or treat bleeding.
We also use fresh frozen plasma and cryoprecipitate to manage coagulation disorders.
Stem Cell and Bone Marrow Transplantation
Stem cell transplantation, including bone marrow transplantation, can cure some blood disorders. It replaces the patient’s diseased bone marrow with healthy stem cells.
- Autologous transplantation using the patient’s own stem cells
- Allogeneic transplantation using stem cells from a donor
Surgical Interventions and Splenectomy
Surgery is sometimes needed. Splenectomy, or removing the spleen, can treat certain blood disorders. This includes hereditary spherocytosis or immune thrombocytopenic purpura.
Other surgeries may be needed to manage complications or treat underlying causes.
Living with and Managing Blood Disorders
Managing blood disorders is more than just medical treatment. It’s about creating a supportive environment for well-being. Living with a blood disorder can be tough, but with the right strategies and support, people can live fulfilling lives.
Symptom Management Strategies
Effective symptom management is key for those with blood disorders. It combines medical treatments and lifestyle changes. For example, people with anemia might need to pace themselves and get enough rest to fight fatigue. Medications like iron supplements or erythropoiesis-stimulating agents can also help.
For bleeding disorders, preventing injuries and bleeding is essential. This means avoiding contact sports, wearing protective gear, and being careful with medications that might increase bleeding risk.
Dietary and Lifestyle Considerations
Diet is important for managing blood disorders. For instance, those with iron deficiency anemia might need to eat more iron-rich foods. A balanced diet with essential nutrients is vital for health and symptom management.
Making lifestyle changes, like regular exercise that fits your condition, can improve your quality of life. Stress management techniques like meditation and yoga can also help with the emotional side of chronic conditions.
Psychosocial Impact and Support Resources
Blood disorders can affect mental health and social interactions. Access to support resources, such as counseling and support groups, is vital for emotional well-being.
Connecting with others who understand the challenges of blood disorders can offer emotional support and practical advice. Patient advocacy organizations often provide resources and support specific to blood disorders.
Monitoring and Follow-up Care
Regular monitoring and follow-up care are essential for managing blood disorders. This includes regular blood tests and check-ups with healthcare providers to track the condition and adjust treatments as needed.
For some conditions, ongoing monitoring for complications is necessary. For example, people with certain anemias might need regular checks for iron overload.
Conclusion
Understanding hematology is key for diagnosing and treating blood disorders. We’ve looked at different blood diseases, their causes, symptoms, and treatments. Each condition needs a detailed approach to manage it well.
Exploring blood disorders shows how complex and varied they are. Good management of these diseases comes from knowing hematology well. This helps healthcare providers give better treatments and improve patient results.
Managing blood diseases requires a mix of treatments, including medicines and lifestyle changes. Knowing about hematology helps patients and doctors create personalized plans. This improves life quality for those with blood disorders.
As we move forward in hematology, staying updated on new research and treatments is vital. This way, we can better care for people with blood diseases. It helps us improve health outcomes and offer complete care.
FAQ
What is hematology?
Hematology is the study of blood and its diseases. It’s a branch of medicine.
What are the main components of blood?
Blood has red blood cells, white blood cells, platelets, and plasma. Each part has its own role.
What is the hematopoietic system?
The hematopoietic system makes blood cells. It includes red blood cells, white blood cells, and platelets.
What are the different types of blood disorders?
Blood disorders can be inherited or acquired. They can be benign or malignant. They affect different parts of blood.
What is anemia?
Anemia is when you don’t have enough red blood cells or hemoglobin. It causes fatigue, weakness, and shortness of breath.
What are the symptoms of leukemia?
Leukemia symptoms include fatigue, weight loss, and frequent infections. You might also bleed or bruise easily.
How are blood disorders diagnosed?
Doctors use complete blood counts and bone marrow aspiration to diagnose blood disorders. They also use genetic testing and imaging studies.
What are the treatment options for blood disorders?
Treatment options include medication, blood transfusions, and stem cell transplantation. Surgery might also be needed, depending on the condition.
How can blood disorders be managed?
Managing blood disorders involves managing symptoms and making lifestyle changes. It also includes psychosocial support and regular check-ups.
What is thrombocytopenia?
Thrombocytopenia is when you have low platelet count. It causes bleeding and bruising.
What is hemophilia?
Hemophilia is a genetic disorder. It affects blood clotting, leading to prolonged bleeding.
What are the risks associated with blood transfusions?
Blood transfusions can cause reactions and transmit diseases. They can also lead to iron overload.
Can blood disorders be prevented?
Some blood disorders can’t be prevented. But, avoiding toxins and living a healthy lifestyle can help reduce risks.
What is the importance of genetic testing in hematology?
Genetic testing helps diagnose and manage blood disorders. It identifies genetic mutations and abnormalities.
References
British Society for Haematology. (n.d.). British Journal of Haematology. https://onlinelibrary.wiley.com/journal/13652141