Last Updated on October 21, 2025 by mcelik
Recent studies show that hematologic disorders affect millions globally. They impact not just the patients but also their families and communities. Hematology is the study of blood and blood diseases. It covers a wide range of conditions that affect the blood and bone marrow.
We aim to provide detailed information on these conditions. We’ll help you understand the complexities of hematology disorders and their health effects.
It’s important to grasp these conditions to improve treatment options and patient outcomes. We’ll dive into the different aspects of hematologic disorders. We’ll share the latest research and medical breakthroughs.
Key Takeaways
- Hematologic disorders are conditions that affect the blood and bone marrow.
- These disorders can have a significant impact on patients and their families.
- Advancements in hematology are key to better treatment options.
- Understanding hematologic disorders is vital for improving patient care.
- Comprehensive support is essential for patients with hematology disorders.
Understanding Hematology and Blood Composition
Hematology is a branch of medicine that studies blood and related disorders. It helps us understand blood’s makeup and how it keeps us healthy.
The Role of Hematology in Medicine
Hematology is vital in medicine. It helps doctors find and treat blood issues. This includes problems like anemia and leukemia.
As experts in the field, we see how important hematology is. Hematologists look at blood samples to find problems. Then, they create treatment plans for each patient.
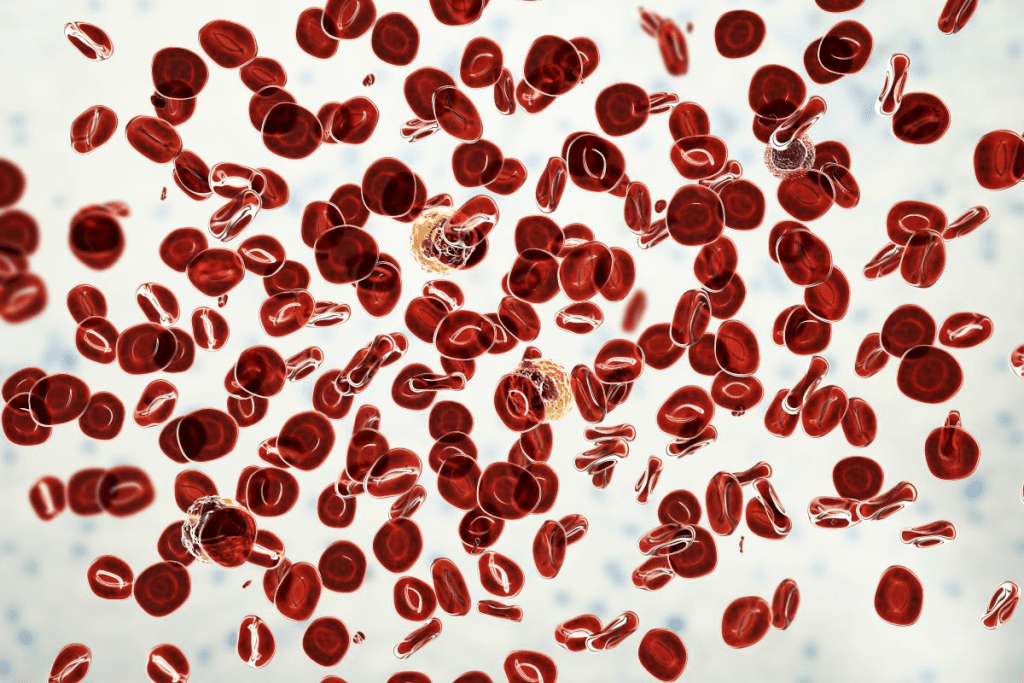
Components of Blood and Their Functions
Blood is made up of several important parts. Each part has its own job. The main parts are:
- Red blood cells, which carry oxygen
- White blood cells, key to our immune system
- Platelets, important for clotting
- Plasma, the liquid part that carries cells and proteins
| Blood Component | Function |
| Red Blood Cells | Carry oxygen throughout the body |
| White Blood Cells | Play a vital role in the immune system |
| Platelets | Essential for blood clotting |
| Plasma | Transports cells, proteins, and other vital substances |
The Bone Marrow’s Role in Blood Production
The bone marrow is a key part of our bones. It makes blood cells, like red and white blood cells, and platelets.
A leading hematologist said,
“The bone marrow is the factory where blood cells are produced, and any disruption in this process can lead to various blood disorders.”
Knowing how the bone marrow makes blood is key. It helps doctors diagnose and treat blood problems. By looking at bone marrow samples, doctors can find the cause of blood issues.
Overview of Blood Disorders and Their Classification

Hematologic disorders include both malignant and non-malignant conditions. They affect different parts of the blood, like red and white blood cells, and platelets. Each part has its own role and can have its own disorders.
Blood disorders are divided into two main types: malignant and non-malignant. Malignant blood disorders involve abnormal cell growth, leading to diseases like leukemia. Non-malignant blood disorders include anemia and bleeding disorders, but they don’t involve cancer.
Malignant vs. Non-Malignant Blood Disorders
Malignant blood disorders have cancerous cells in the blood or bone marrow. They can cause problems like anemia and infections. Non-malignant disorders, though not cancerous, can also affect a person’s life quality.
Prevalence of Blood Disorders in the United States
Blood disorders affect millions in the United States. Anemia, leukemia, and lymphoma are among the most common. Knowing how common these are helps plan healthcare better.
The chance of getting certain blood disorders varies. Age, gender, and where you live can play a part. For example, some anemias are more common in certain groups, and leukemia risk goes up with age.
Risk Factors for Developing Hematologic Conditions
Several things can raise the risk of getting blood disorders. Genetics, exposure to chemicals or radiation, and infections are some. Knowing these risks helps catch problems early.
- Genetics are key in some disorders, like sickle cell anemia.
- Exposure to toxins and radiation can lead to cancerous blood disorders.
- Infections, like HIV, can also raise the risk of certain blood conditions.
Understanding blood disorders helps doctors plan better care. This includes how to diagnose, treat, and prevent these conditions. A detailed approach is key to better patient outcomes.
Red Blood Cell Disorders
Red blood cell disorders affect how red blood cells are made, work, and last. They can cause mild fatigue to serious health problems. We’ll look at the different types, their causes, symptoms, and treatments.
Anemia and Its Various Types
Anemia means not enough red blood cells or poor quality ones. This makes it hard for tissues and organs to get enough oxygen. There are many types, like iron-deficiency anemia and vitamin deficiency anemia.
Iron-deficiency anemia is common. It’s often due to not eating enough iron, losing blood, or needing more iron. Vitamin deficiency anemia happens when you lack vitamins like B12 or folate, which are key for making red blood cells.
| Type of Anemia | Causes | Symptoms |
| Iron-Deficiency Anemia | Inadequate dietary intake, chronic blood loss | Fatigue, weakness, pale skin |
| Vitamin Deficiency Anemia | Lack of vitamin B12 or folate | Fatigue, weakness, neurological changes |
| Anemia of Chronic Disease | Chronic diseases such as rheumatoid arthritis or cancer | Fatigue, weakness, shortness of breath |
Polycythemia and Erythrocytosis
Polycythemia and erythrocytosis mean having too many red blood cells. This can make blood thicker and cause heart problems. Polycythemia vera is a rare disorder that affects red and white blood cells and platelets.
Erythrocytosis can be genetic or caused by not enough oxygen. Symptoms include headaches, dizziness, and itching, often after taking a hot shower.
Hemolytic Disorders
Hemolytic disorders cause red blood cells to break down too early. This can be due to genes, infections, medicines, or autoimmune diseases. Symptoms include jaundice, fatigue, and shortness of breath.
Hemolytic anemia can be sudden or long-term. Treatment focuses on fixing the cause, reducing cell breakdown, and managing side effects.
We’ve talked about red blood cell disorders like anemia, polycythemia, erythrocytosis, and hemolytic disorders. Knowing about these conditions helps with diagnosis and treatment.
White Blood Cell Disorders
White blood cells are key to our immune system. Disorders affecting these cells can have big health effects. These conditions can either weaken or overactivate our immune response.
Leukopenia and Neutropenia

Leukopenia is when there are fewer white blood cells, making us more likely to get sick. Neutropenia is a type of leukopenia where there are fewer neutrophils. Neutrophils help fight bacterial infections, and not having enough can cause serious infections.
We find out if someone has leukopenia or neutropenia by checking their blood. The treatment depends on what’s causing it, like bone marrow problems or certain medicines.
Leukocytosis and Infections
Leukocytosis is when there are too many white blood cells. This can happen due to infections, inflammation, or stress. While it’s a normal response, very high counts can mean there’s something wrong, like an infection or leukemia.
Infections often cause leukocytosis because the body makes more white blood cells to fight off germs. We treat leukocytosis by fixing the cause, like using antibiotics for bacterial infections.
Leukemia: Types and Characteristics
Leukemia is a cancer of white blood cells. It’s mainly divided into acute and chronic types, based on how fast it grows. Acute leukemia needs quick treatment because it grows fast, while chronic leukemia grows slower.
Leukemia is also classified by the type of white blood cell affected, like lymphoid or myeloid cells. Knowing the exact type of leukemia is key to finding the right treatment. This can include chemotherapy, targeted therapy, or bone marrow transplantation.
Platelet and Clotting Disorders
The body needs to form blood clots to stay healthy. Problems with this process can cause big issues. Disorders in platelet and clotting can make it hard for the body to stop bleeding, leading to serious health problems.
Thrombocytopenia
Thrombocytopenia means you have too few platelets in your blood. Platelets are key for blood clotting. Without enough, you might bleed more and bruise easily. It can be caused by bone marrow issues, some medicines, or autoimmune diseases.
Thrombocytosis
Thrombocytosis is when you have too many platelets. This can raise your risk of blood clots. Blood clots can cause heart problems. It can be caused by a bone marrow issue or another health problem.
Hemophilia and Other Clotting Factor Deficiencies
Hemophilia is a genetic disorder that makes it hard for the body to clot blood. It’s caused by a lack of clotting factors VIII or IX. Other clotting factor issues can also affect blood clotting.
Von Willebrand Disease
Von Willebrand disease affects blood clotting too. It’s due to a problem with the von Willebrand factor protein. Symptoms include easy bruising and heavy menstrual bleeding in women.
It’s important to understand these disorders to manage and treat them well. We’ll look at how to diagnose and treat them next.
Lymphatic System Disorders
It’s important to understand lymphatic system disorders to diagnose and treat conditions like lymphoma and lymphadenopathy. The lymphatic system is key to our immune function. Disorders here can seriously affect our health.
Lymphoma: Hodgkin and Non-Hodgkin
Lymphoma is a cancer that starts in the lymph system, part of our immune system. There are two main types: Hodgkin lymphoma and non-Hodgkin lymphoma.
Hodgkin Lymphoma: This type has Reed-Sternberg cells. It’s usually treated with chemotherapy and radiation.
Non-Hodgkin Lymphoma: More common, its treatment depends on the subtype and stage.
Multiple Myeloma
Multiple myeloma is a cancer of plasma cells in the bone marrow. It can cause anemia, bone pain, and infections.
Symptoms include:
- Bone pain or fractures
- Fatigue and anemia
- Infections
- Hypercalcemia
Lymphadenopathy
Lymphadenopathy means enlarged lymph nodes. It can be due to infections, autoimmune disorders, or cancers.
| Causes | Characteristics |
| Infections | Tender lymph nodes, often with fever and other infection symptoms |
| Cancer | Painless lymph node enlargement, possibly with weight loss |
| Autoimmune Disorders | Lymph node enlargement with conditions like rheumatoid arthritis |
It’s vital to find the cause of lymphadenopathy for the right treatment.
Bone Marrow Disorders
Understanding bone marrow disorders is key to diagnosing and treating blood cell production issues. These disorders can cause serious health problems, affecting a person’s quality of life. We will look at the different types of bone marrow disorders and their characteristics.
Myelodysplastic Syndromes
Myelodysplastic syndromes (MDS) are disorders where blood cells are poorly formed or don’t work right. This can cause anemia, infections, and bleeding. MDS is linked to genetic mutations and can turn into acute myeloid leukemia (AML).
Myeloproliferative Neoplasms
Myeloproliferative neoplasms (MPNs) are when the body makes too many blood cells. This can cause polycythemia vera, essential thrombocythemia, and primary myelofibrosis. MPNs can raise the risk of blood clots and turning into AML.
Bone Marrow Failure Syndromes
Bone marrow failure syndromes happen when the bone marrow can’t make enough blood cells. This leads to aplastic anemia, where the bone marrow can’t make new blood cells. It can be caused by genetics or other factors.
The following table summarizes the key characteristics of these bone marrow disorders:
| Disorder | Key Characteristics | Potential Complications |
| Myelodysplastic Syndromes (MDS) | Poorly formed or dysfunctional blood cells | Anemia, infection, bleeding, progression to AML |
| Myeloproliferative Neoplasms (MPNs) | Overproduction of blood cells | Thrombosis, transformation to AML, myelofibrosis |
| Bone Marrow Failure Syndromes | Failure to produce sufficient blood cells | Aplastic anemia, infections, bleeding |
Diagnosing and treating bone marrow disorders needs a detailed approach. This includes lab tests, bone marrow biopsies, and genetic analysis. Treatment options depend on the disorder and may include medicines, blood transfusions, and stem cell transplants.
Genetic and Inherited Blood Disorders
It’s important to know about genetic blood disorders to help those affected. These disorders change how blood works, often because of gene mutations. They affect blood cell production or maintenance.
These conditions are tough because they run in families. “They can be passed down from parents to kids, making family history key for diagnosis,” says a top hematologist.
Hemoglobinopathies
Hemoglobinopathies are genetic disorders that mess with hemoglobin. This protein is vital for carrying oxygen in red blood cells. Sickle cell disease and hemoglobin C disease are examples, each with its own symptoms and treatments.
Thalassemias
Thalassemias are genetic disorders that lead to less hemoglobin. They’re split into alpha-thalassemia and beta-thalassemia, based on which globin chain is affected. The severity can range from mild to severe, needing blood transfusions.
Hereditary Spherocytosis
Hereditary spherocytosis affects the red blood cell membrane. It makes red blood cells abnormally shaped, leading to early destruction. This can cause anemia, jaundice, and an enlarged spleen. Treatment often involves removing the spleen to slow down red blood cell destruction.
G6PD Deficiency
G6PD deficiency is a genetic disorder that makes red blood cells more likely to break down. This happens under certain conditions, like infections or specific drugs. Managing it means avoiding triggers and treating acute episodes.
In summary, genetic and inherited blood disorders are complex. Knowing their genetic causes is key to proper care. As genetic research and diagnostics improve, so does the care for those affected.
Diagnosing Blood Disorders
To find out what’s wrong with blood, doctors use many tests. These include complete blood counts and bone marrow biopsies. Getting the right diagnosis is key for good treatment and care.
Complete Blood Count and Other Laboratory Tests
A Complete Blood Count (CBC) is a common test for blood disorders. It checks the blood for red and white cells, hemoglobin, and platelets. If the results are off, it might mean anemia, infection, or leukemia.
Other tests like blood smears and reticulocyte counts help too. They give clues about the blood’s makeup and can spot specific problems.
| Laboratory Test | Purpose | Indications |
| Complete Blood Count (CBC) | Measures blood components | Anemia, infection, leukemia |
| Blood Smear | Examines blood cell morphology | Abnormal cell shapes, infections |
| Reticulocyte Count | Assesses bone marrow activity | Anemia, bone marrow disorders |
Bone Marrow Biopsy and Aspiration
A bone marrow biopsy takes a small bone marrow sample for study. It’s key for finding issues like myelodysplastic syndromes and leukemia. Bone marrow aspiration gives more details about the marrow’s cells.
“Bone marrow examination is a critical diagnostic tool in hematology, providing insights into the production and function of blood cells.”
” Hematologist
Genetic Testing for Blood Disorders
Genetic testing is vital for inherited blood disorders like sickle cell disease and thalassemia. It looks at genes to find mutations that cause these conditions. This helps doctors give the right treatment.
Imaging Studies in Hematology
Imaging studies like X-rays and MRI help see how far a disease has spread. They check for things like big lymph nodes or spleen, signs of lymphoma or other cancers.
By using all these tests, doctors can accurately diagnose and treat blood disorders. This leads to better health outcomes for patients.
Treatment Approaches for Blood Disorders
Treating blood disorders is complex and requires different methods for each condition. These disorders include anemia, clotting issues, and cancers like leukemia and lymphoma. Each one needs a special treatment plan.
Medication Therapies
Medicine is key in managing many blood disorders. Chemotherapy is used to fight leukemia and lymphoma by targeting fast-growing cancer cells. Targeted therapy aims at specific molecules in cancer cells, aiming for fewer side effects.
Other drugs help with symptoms or complications. For example, anticoagulants stop blood clots in clotting disorders. Iron chelators reduce iron buildup in patients getting many blood transfusions.
Blood Transfusions and Blood Products
Blood transfusions are a common treatment for anemia or low blood cell counts. Red blood cell transfusions boost healthy red blood cells, improving oxygen delivery. Platelet transfusions help prevent or treat bleeding in patients with low platelets.
Stem Cell Transplantation
Stem cell transplantation, or bone marrow transplantation, can cure some blood disorders. It replaces the patient’s bad bone marrow with healthy stem cells. These can come from the patient (autologous) or a donor (allogeneic).
Surgical Interventions
Some blood disorders need surgical intervention. For instance, removing the spleen (splenectomy) might be needed for certain conditions. Surgery can also help diagnose or treat complications, like lymph node biopsies in lymphoma.
The Role of Hematology Specialists
Hematology specialists play a key role in managing blood disorders. They are doctors who focus on blood-related conditions. They handle both simple and complex blood issues.
What Hematologists Do
Hematologists diagnose and treat blood disorders like anemia and blood cancers. They use tests and biopsies to find the cause. Then, they create a treatment plan for each patient.
They work with other doctors to give full care. Their goal is to find the best treatments and improve patients’ lives.
When to See a Hematologist
See a hematologist if you’re tired a lot, get sick often, or bruise easily. If you have a blood disorder or a family history, it’s also a good idea.
Early treatment can make a big difference. Hematologists help patients understand their condition and plan their treatment.
The Hematology-Oncology Connection
Hematology and oncology often overlap, as many blood disorders are cancers. Hematologist-oncologists can handle both blood disorders and cancer.
We work with oncologists to give full care to patients with blood cancers.
Finding the Right Hematology Specialist
Look for a hematologist with the right qualifications and experience. Ask your doctor or friends for recommendations.
Patients should ask questions about their care. Working with a qualified hematologist helps manage blood disorders well.
Living with Blood Disorders
Managing a chronic blood disorder needs a full plan. This includes medical care, lifestyle changes, and emotional support. It’s key to know how these conditions affect our daily lives.
Managing Daily Life with a Chronic Blood Condition
Life with a blood disorder can be tough. But, there are ways to handle it well. Patients often talk about adapting to a new way of living.
People with bleeding disorders might stay away from activities that could hurt them. Those with anemia might need to slow down to avoid getting tired. Managing it well means treating it medically, making lifestyle changes, and keeping an eye on it.
Support Resources for Patients
Right support can make life better for those with blood disorders. Support groups, online or in-person, let patients share and learn. They find out they’re not alone.
Also, many groups offer educational stuff, counseling, and help in speaking up. Connecting with these resources helps patients manage their condition better.
Nutrition and Lifestyle Considerations
Nutrition is key in managing blood disorders. Eating right can help symptoms or make treatments work better. For example, people with iron deficiency anemia might eat more iron.
Staying away from things that could make the condition worse is also important. Eating well and living healthy can really help your health.
Psychological Impact and Coping Strategies
Chronic blood disorders can really affect your mind. It’s common to feel anxious, depressed, or stressed.
Finding ways to cope is vital. This could mean talking to a counselor, learning to relax, or doing things that make you happy. By tackling the mental side, you can live better despite your health issues.
In conclusion, dealing with blood disorders needs a whole approach. Knowing your condition, getting support, making smart lifestyle choices, and dealing with the mental side can help you live well.
“The greatest wealth is health.” – Virgil
Conclusion
Understanding blood disorders is key to managing and treating them. This article has covered the basics of blood, different disorders, how to diagnose them, and treatment options.
Blood disorders can be either malignant or non-malignant. Their occurrence changes among different groups of people. Hematology specialists play a big role in diagnosing and treating these conditions. More research is needed to better help patients.
In short, knowing about blood disorders is very important. By learning about causes, symptoms, and treatments, patients and doctors can improve life quality for those with blood disorders.
As we move forward in hematology, focusing on patient care is critical. We must also support research and raise awareness about blood disorders. This will help improve patient outcomes and save lives.
FAQ
References
Varon, J. (2016). Hematologic disorders. In Critical Care Medicine (pp. xx-xx). The University of Texas Health Science Center at Houston. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7122868/