Last Updated on October 21, 2025 by mcelik
Hematology is a key medical field that studies blood and blood-forming organs. A blood doctor (hematologist) helps diagnose and treat many diseases, like anemia and leukemia. It also covers lymphoma and bleeding disorders.
Hematology is vital in medicine. It helps manage conditions that affect millions globally. By learning about hematology, we see its big role in healthcare and how it helps patients.
Key Takeaways
- Hematology is a medical specialty focused on blood-related disorders.
- Hematologists diagnose and treat various conditions, including anemia and leukemia.
- The field of hematology is critical for understanding and managing blood-related diseases.
- Hematology plays a significant role in patient care and treatment.
- Understanding hematology can help individuals better manage their health.
The Science of Hematology: Understanding Blood and Its Components
Hematology explores the details of blood and its parts. It looks at how these parts keep us healthy. This field is key for finding and treating blood problems.
Definition and Scope of Hematology
Hematology is a medical area that studies blood and its parts. It deals with diagnosing, treating, and managing blood issues. This makes it very important for patient care.
It’s not just about blood parts. It’s also about how they work together to keep us healthy. This includes looking at blood disorders and their causes and effects.
The Four Major Components of Blood
Blood has four main parts: red blood cells, white blood cells, platelets, and plasma. Each part has a special job that helps keep us healthy.
- Red blood cells carry oxygen to all parts of the body.
- White blood cells help fight infections and support the immune system.
- Platelets help blood to clot, stopping too much bleeding.
- Plasma is the liquid part of blood. It carries cells and proteins around the body.
How Blood Functions in the Human Body
Blood does many important jobs in our bodies. It carries oxygen and nutrients to cells, takes away waste, and helps keep body temperature stable. It also helps control blood pressure and supports the immune system.
Knowing how blood works is key to diagnosing and treating blood disorders. By studying blood components and their roles, hematologists can spot problems and find the right treatments.
What is a Blood Doctor? The Role and Expertise of Hematologists

Hematologists are doctors who focus on blood-related issues. They study blood, its problems, and the blood-making organs. They get a lot of training to be experts in this field.
Education and Specialized Training Requirements
To be a hematologist, one needs a lot of education and training. First, they go to medical school. Then, they do a residency in internal medicine or pediatrics. After that, they get more training in hematology through fellowship programs.
This long and hard path prepares them to handle complex blood disorders. Their hard work helps them give top-notch care to patients with blood diseases.
Differences Between Hematologists and Other Medical Specialists
Hematologists are different because they focus on blood disorders. General doctors or internists might handle simple blood issues. But hematologists deal with the tough cases.
They are experts in treating anemia, bleeding disorders, and blood cancers. They are key in the healthcare world.
Hematologists also work with oncologists. This team effort is important for patients with blood cancers.
Hematology-Oncology: Understanding the Connection
Hematology and oncology are closely linked. Many blood disorders are cancers, like leukemia and lymphoma. Hematology-oncology combines treating blood diseases and cancers.
Hematologist-oncologists are trained for both aspects. They give a complete care plan for patients. This integrated approach is vital for effective treatment.
Common Hematological Tests and Diagnostic Procedures
Hematological tests are key in diagnosing blood-related disorders. They help identify problems with blood cells and clotting. This information guides treatment and care for patients.
Complete Blood Count (CBC): The Fundamental Blood Test
A Complete Blood Count (CBC) is a common test. It checks the different parts of blood, like red and white cells, and platelets. It’s vital for spotting blood disorders, such as anemia and leukemia.
The CBC looks at hemoglobin, hematocrit, white blood cells, and platelets. Odd results can show issues like anemia or leukemia. We use these results to plan further tests and treatments.
Blood Smear Examination and Interpretation
A blood smear test spreads blood on a slide, stains it, and looks at it under a microscope. It helps see blood cell shapes, spotting issues not seen by machines alone.
This test is great for finding malaria parasites in red blood cells. It also spots odd white or platelet cells, hinting at blood disorders.
Coagulation Studies and Bleeding Time Tests
Coagulation studies check if blood clots right. They measure clotting factors, helping spot bleeding disorders like hemophilia. Tests like prothrombin time (PT) and activated partial thromboplastin time (aPTT) are used.
Bleeding time tests see if the body can stop bleeding. Long times can mean platelet or clotting issues. These tests help find bleeding risks or clotting problems.
Bone Marrow Aspiration and Biopsy Procedures
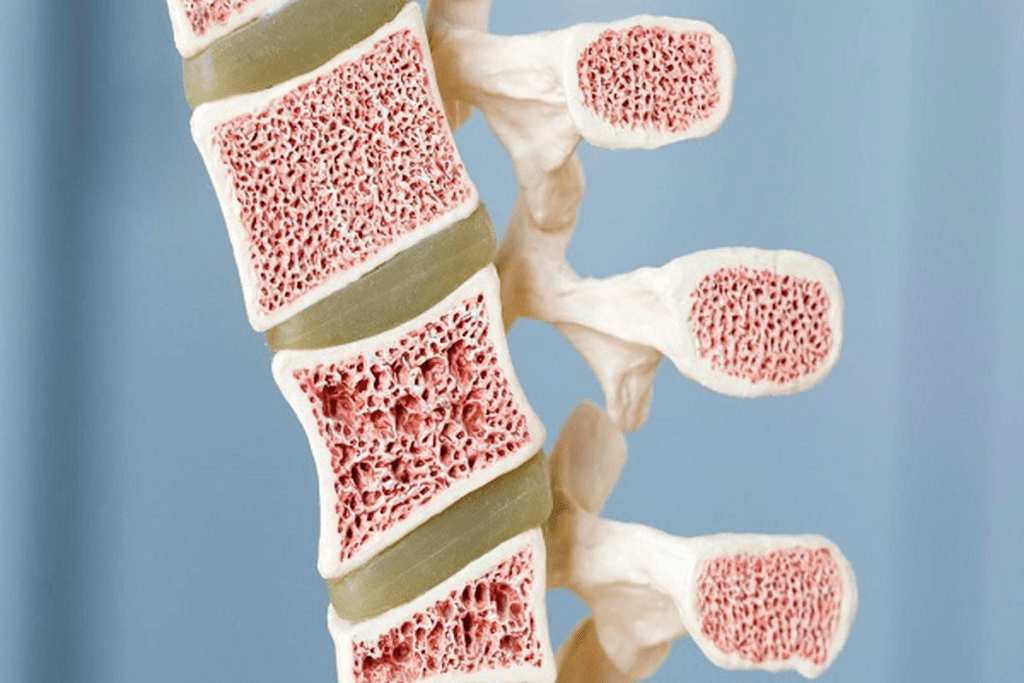
Bone marrow tests are deep into the bone marrow, where blood cells are made. They’re key for finding blood disorders like leukemia. Aspiration takes liquid marrow, and biopsy takes bone tissue for a closer look.
These tests give insights into blood cell production and function. They’re vital for diagnosing and treating blood disorders.
Red Blood Cell Disorders Detected Through Hematology
Hematology has made big strides in diagnosing and treating red blood cell disorders. These disorders, like anemia, affect how red blood cells are made or live. Doctors use tests and treatments to manage these conditions.
Iron Deficiency Anemia: Causes and Detection
Iron deficiency anemia is very common around the world. It happens when the body doesn’t have enough iron for hemoglobin. Causes include not getting enough iron in your diet, losing blood too much, and needing more iron during pregnancy or when you’re growing. Doctors find iron deficiency anemia by checking your blood for hemoglobin, MCV, and serum ferritin levels.
Vitamin B12 and Folate Deficiency Anemias
Vitamin B12 and folate deficiencies can also cause anemia. These vitamins are key for making DNA and for red blood cells to mature. Not getting enough of these vitamins can come from a bad diet, not being able to absorb them well, or taking certain medicines. Doctors check your blood for these vitamins and other signs of anemia.
Hemolytic Anemias: When Red Blood Cells Break Down Prematurely
Hemolytic anemias happen when red blood cells break down too early. This can be due to genetic issues, autoimmune diseases, infections, or certain drugs or toxins. Doctors find the cause by doing tests like the direct Coombs test, hemoglobin electrophoresis, and looking at the shape of red blood cells.
Aplastic Anemia and Bone Marrow Failure
Aplastic anemia is a rare but serious condition where the bone marrow can’t make blood cells. Causes include toxins, radiation, some medicines, and viral infections. Doctors diagnose it with a bone marrow biopsy to see if it’s working right. Treatment might include medicines to suppress the immune system or a bone marrow transplant.
Blood Clotting Disorders Diagnosed by Hematologists
Blood clotting is a delicate process. When it goes wrong, it can cause serious health problems. Hematologists are experts in diagnosing and treating these disorders. They help with both too much bleeding and too much clotting.
Hemophilia A and B: Testing and Diagnosis
Hemophilia A and B are genetic disorders. They happen when there’s not enough clotting factor VIII or IX. Diagnosis includes clinical checks, family history, and lab tests. These tests measure the clotting factor levels.
“Early diagnosis and proper treatment can greatly improve life for those with hemophilia,” says a hematologist. This highlights the importance of hematological care.
Von Willebrand Disease: The Most Common Inherited Bleeding Disorder
Von Willebrand disease is the most common inherited bleeding disorder. It’s caused by a lack of problem with the von Willebrand factor. Diagnosis uses tests like von Willebrand factor antigen and activity assays.
Thrombophilia and Hypercoagulable States
Thrombophilia means you’re more likely to form blood clots. Tests for thrombophilia look for genetic or acquired conditions that cause clotting.
A leading hematologist says, “Finding the cause of thrombophilia is key to preventing blood clots.”
Acquired Clotting Disorders
Acquired clotting disorders can come from many sources. These include medicines, health conditions, or lack of nutrients. Diagnosis needs a full clinical check and lab tests to find the cause.
We know managing blood clotting disorders needs a team effort. As hematologists, we are key players in this team.
White Blood Cell Disorders and Immune System Dysfunction
Understanding white blood cell disorders is key to treating immune system problems. White blood cells help fight infections and diseases. Disorders in these cells can cause health issues, from mild to severe.
Leukopenia and Neutropenia: When White Cell Counts Drop
Leukopenia is when white blood cell counts are too low. Neutropenia is a type of leukopenia with low neutrophils, important for fighting infections. We use a Complete Blood Count (CBC) test to diagnose these conditions.
Causes include bone marrow issues, certain drugs, and autoimmune diseases. Treatment aims to fix the cause and boost white blood cell production.
Leukocytosis: Elevated White Blood Cell Counts
Leukocytosis is when white blood cell counts are too high. It can be due to infections, inflammation, or stress. We use tests like blood smears and bone marrow biopsies to find the cause.
It can signal infections or serious diseases like leukemia. Treating the cause is essential.
Myelodysplastic Syndromes
Myelodysplastic syndromes (MDS) are disorders with poorly formed blood cells, leading to bone marrow failure. They can turn into acute myeloid leukemia (AML).
We diagnose MDS by examining bone marrow and blood cells. Treatment depends on the risk level and may include supportive care, medications, or bone marrow transplants.
Immune Deficiency Disorders
Immune deficiency disorders weaken the immune system’s ability to fight infections and diseases. They can be inherited or acquired due to infections, drugs, or aging.
Diagnosing these disorders involves various tests, including immunoglobulin level measurements. Treatment depends on the cause and may include immunoglobulin replacement therapy or antimicrobial prophylaxis.
| Condition | Description | Common Diagnostic Tests |
| Leukopenia | Low white blood cell count | CBC, Bone Marrow Biopsy |
| Leukocytosis | High white blood cell count | CBC, Blood Smear |
| Myelodysplastic Syndromes | Dysfunctional blood cells | Bone Marrow Biopsy, Cytogenetic Analysis |
| Immune Deficiency Disorders | Compromised immune system | Immunoglobulin Levels, Functional Immune Tests |
Platelet and Bleeding Disorders
Platelet disorders are key in hematology. They affect how blood clots and maintains hemostasis. We’ll dive into these disorders, covering their causes, diagnosis, and treatment.
Thrombocytopenia: Causes and Diagnosis
Thrombocytopenia means having too few platelets. It can come from bone marrow failure, immune issues, or spleen problems. Diagnosing it involves a detailed blood count and sometimes a bone marrow test. These steps help us find the cause and plan treatment.
Thrombocytosis and Essential Thrombocythemia
Thrombocytosis is when you have too many platelets. It can be due to another condition or a rare disorder called essential thrombocythemia. Essential thrombocythemia makes the bone marrow produce too many platelets, raising the risk of blood clots. We use blood tests, bone marrow biopsies, and genetic tests to diagnose and manage it.
Qualitative Platelet Disorders
Qualitative platelet disorders affect how platelets work, even if their numbers are normal. These can be inherited or acquired and often lead to bleeding. Diagnosing them requires special tests like platelet aggregometry.
Vascular Purpuras and Vessel Wall Defects
Vascular purpuras and vessel wall defects are bleeding disorders related to blood vessel health. Conditions like hereditary hemorrhagic telangiectasia or senile purpura show how important blood vessel health is for hemostasis. We evaluate these conditions thoroughly, including clinical assessments and sometimes vascular imaging.
“Diagnosing and managing platelet and bleeding disorders need a deep understanding of hematology and a focus on the patient,” say top hematologists. We aim to give full care, using the latest in hematology to better patient results.
Blood Cancers: How Hematology Tests Detect Malignancies
Blood cancers, like leukemia and lymphoma, are tough to diagnose and treat. But, new advances in hematology have helped patients. These cancers affect the blood, bone marrow, and lymphatic system, needing special tests to find them.
Leukemia: Acute and Chronic Forms
Leukemia is a blood cancer with too many bad white blood cells. It’s either acute, which moves fast, or chronic, which grows slower. Doctors use tests like the Complete Blood Count (CBC) and bone marrow aspiration to spot leukemia.
Acute Leukemia: This needs quick action because it grows fast. Symptoms include feeling tired, getting sick easily, and bruising easily.
Chronic Leukemia: This might not show signs for years. It’s important to keep an eye on it and act fast when needed.
Lymphoma: Hodgkin and Non-Hodgkin Types
Lymphoma starts in the lymphatic system and has two main types: Hodgkin and non-Hodgkin. Doctors use lymph node biopsies and imaging to diagnose it.
Hodgkin Lymphoma: It has Reed-Sternberg cells and is treated with chemotherapy and radiation.
Non-Hodgkin Lymphoma: This group is more varied and treatment depends on the type and stage. It often includes chemotherapy, targeted therapy, or immunotherapy.
Multiple Myeloma and Plasma Cell Disorders
Multiple myeloma is a cancer of plasma cells in the bone marrow. Doctors find it by looking for monoclonal proteins in blood or urine and checking the bone marrow.
Treatment for multiple myeloma includes targeted therapies, chemotherapy, and stem cell transplants. Hematologists also handle plasma cell disorders like monoclonal gammopathy of undetermined significance (MGUS).
Myeloproliferative Neoplasms
Myeloproliferative neoplasms (MPNs) are diseases with too many blood cells. They include polycythemia vera, essential thrombocythemia, and primary myelofibrosis.
Diagnosing MPNs involves blood counts, genetic tests for JAK2 mutations, and bone marrow exams. Treatment tries to prevent problems like blood clots and turning into acute leukemia.
Genetic and Inherited Blood Disorders
Hematology deals with many genetic disorders that affect blood function. These conditions are passed down through genes and can greatly impact a person’s life. We will look at some common genetic blood disorders and their effects.
Sickle Cell Disease: Testing and Diagnosis
Sickle cell disease is a genetic disorder that changes hemoglobin, making red blood cells sickle-shaped. These cells can block small blood vessels, causing pain and serious health problems. A blood test checks for hemoglobin S to diagnose it.
To find sickle cell disease, we use tools like genetic testing. This helps us spot the mutation causing the condition. Finding it early is key to managing it well and improving health outcomes.
Thalassemia Syndromes: Alpha and Beta Types
Thalassemia is a genetic disorder that affects hemoglobin production. It has two main types: alpha and beta thalassemia, each with different levels of severity. Blood tests and genetic testing help diagnose it.
- Alpha Thalassemia: Caused by mutations in one or more of the four genes that code for alpha-globin.
- Beta Thalassemia: Results from mutations in one or both of the two genes that code for beta-globin.
Hereditary Spherocytosis and Membrane Defects
Hereditary spherocytosis makes red blood cells sphere-shaped instead of the usual disk shape. This shape problem stops them from passing through small blood vessels, leading to early destruction. Diagnosis often involves family history, physical checks, and lab tests.
We find hereditary spherocytosis through tests like the osmotic fragility test and genetic analysis. These tests look for mutations in proteins of the red blood cell membrane.
G6PD Deficiency and Enzymatic Disorders
G6PD deficiency is an enzymatic disorder that makes red blood cells more likely to break down under certain conditions. We diagnose it by testing for G6PD enzyme activity in red blood cells.
Key points about G6PD deficiency:
- Affects mostly males due to its X-linked recessive inheritance pattern.
- Can cause hemolytic anemia in response to certain triggers like infections or specific medications.
- Management involves avoiding known triggers and, in some cases, supportive care during hemolytic episodes.
Pediatric Hematology: Blood Disorders in Children
Blood disorders in kids are a big challenge. Pediatric hematology works hard to help. We know kids need special care because of their unique needs.
Neonatal Blood Disorders and Screening
Newborns can have blood disorders. These are often found through early tests. Conditions like hemolytic disease of the newborn need quick action.
| Condition | Description | Screening Method |
| Hemolytic Disease of the Newborn | A condition where maternal antibodies destroy newborn red blood cells. | Blood typing and Coombs test |
| Neonatal Thrombocytopenia | Low platelet count in newborns, potentially leading to bleeding. | Complete Blood Count (CBC) |
Childhood Anemias and Their Unique Presentations
Anemia in kids can come from many sources. It’s different from adults because of how it shows up. Iron deficiency anemia is common, often from not eating enough iron or losing blood too much.
Pediatric Blood Cancers
Pediatric blood cancers, like leukemia and lymphoma, are serious. Acute lymphoblastic leukemia (ALL) is the top cancer in kids. Thanks to new treatments, more kids are surviving.
- Acute Lymphoblastic Leukemia (ALL)
- Acute Myeloid Leukemia (AML)
- Lymphoma
Developmental Hematological Disorders
Developmental hematological disorders happen when the blood-making system is forming. They affect how blood cells are made or work. Knowing about these is key to helping kids.
We aim to give the best care to kids with blood disorders. We use the newest research in pediatric hematology to help them get better.
When to Consult a Blood Doctor: Signs You Need a Hematologist
Knowing when to see a blood doctor is key to good health. Hematologists specialize in blood and its parts. If you notice certain symptoms, it’s time to see a hematologist.
Unexplained Fatigue, Weakness, and Pallor
Feeling tired, weak, or pale without reason could mean anemia or other blood issues. Don’t ignore these signs.
Common causes include:
- Iron deficiency
- Vitamin B12 or folate deficiency
- Bone marrow disorders
Abnormal Bleeding, Bruising, and Clotting
Seeing too much bruising or bleeding, or clotting too much? It might be a sign of a platelet or clotting problem. Hemophilia or thrombophilia need a hematologist’s help.
| Symptom | Possible Condition |
| Frequent bruising | Platelet disorder |
| Prolonged bleeding | Clotting factor deficiency |
| Recurrent clots | Thrombophilia |
Recurrent Infections and Immune Concerns
Getting sick a lot? It could be a sign of a white blood cell problem. Hematologists can help with immune system issues.
“The role of a hematologist is not just to treat blood disorders but to understand the intricacy of blood components and their health impact.” – Expert in Hematology
Understanding Referrals from Primary Care Physicians
Your primary care doctor might send you to a hematologist if they think you have a blood issue. Knowing why can help you get the right care.
If you’re showing signs of blood problems, see a doctor fast. Early treatment can make a big difference.
The Hematology Diagnostic Process: From Consultation to Diagnosis
The hematology diagnostic process is complex and involves several steps. It aims to accurately diagnose blood disorders. Hematologists follow a detailed pathway to gather all needed information for an accurate diagnosis.
Initial Consultation and Medical History
The journey starts with an initial consultation. We collect a detailed medical history from the patient. This step is key as it gives insights into symptoms, family history, and past medical conditions.
We also discuss lifestyle, diet, and medications during the consultation. This approach helps us understand the patient’s health context and its relation to their blood disorder.
Physical Examination for Blood Disorders
A thorough physical examination follows. We look for signs like pallor, jaundice, or bruising. These signs guide further testing.
For example, a suspected anemia patient may show fatigue or shortness of breath. These signs help us assess the condition’s severity and the next steps.
Laboratory Testing Sequences
Laboratory testing is a key part of the process. We start with a Complete Blood Count (CBC) to overview blood cell counts. Based on CBC results, we may do more tests like blood smear examinations or coagulation studies.
- A CBC evaluates red and white blood cell counts and platelet count.
- Blood smear examinations visually check blood cells for abnormalities.
- Coagulation studies assess blood clotting mechanisms.
Advanced Diagnostic Techniques and Genetic Testing
In some cases, we use advanced techniques like genetic testing. This helps diagnose specific blood disorders. Genetic testing looks for inherited conditions like sickle cell disease or thalassemia.
Molecular testing is also used to detect genetic mutations or abnormalities. This is key in diagnosing and managing blood cancers like leukemia or lymphoma.
Conclusion: Advances in Hematology and Future Directions
Hematology has made big strides, leading to better diagnosis and treatment of blood disorders. Research keeps pushing the field forward. This means doctors can now give patients more effective care.
Looking ahead, hematology will focus on personalized medicine. This means treatments will be tailored to each patient based on their genetic makeup. Gene editing, like CRISPR, could be a game-changer for genetic blood disorders.
New treatments and diagnostic tools are on the horizon. Our understanding of blood cells and the immune system will deepen. This will lead to more precise and effective treatments.
Hematology is set for more innovation. We’re excited for the breakthroughs that will enhance patient care and quality of life.
FAQ
What is hematology?
Hematology is a medical field that studies blood disorders and diseases. It involves diagnosing and treating these conditions.
What does a hematologist do?
A hematologist is a doctor who deals with blood disorders. They treat conditions like anemia, bleeding issues, and blood cancers.
What are the common tests used in hematology?
Tests like the Complete Blood Count (CBC) and blood smears are common. They also do coagulation studies and bone marrow tests.
What are the symptoms that may require a hematologist’s care?
Symptoms like fatigue, weakness, and abnormal bleeding are signs you might need a hematologist. Also, bruising, clotting, and frequent infections.
What is the difference between a hematologist and an oncologist?
Hematologists focus on blood disorders. Oncologists deal with cancer. Hematology-oncology combines both, treating blood cancers.
How long does it take to become a hematologist?
It takes about 11-12 years after college. First, you need to finish medical school, then an internal medicine residency, and a hematology fellowship.
What are some common blood disorders diagnosed by hematologists?
Hematologists treat anemia, bleeding disorders, and blood cancers. This includes hemophilia, thrombophilia, and leukemia.
Can a primary care physician refer me to a hematologist?
Yes, primary care doctors often refer patients to hematologists. This is when they suspect a blood disorder.
What is the role of genetic testing in hematology?
Genetic testing is key for diagnosing inherited blood disorders. It helps with sickle cell disease, thalassemia, and some cancers.
Are hematologists involved in cancer treatment?
Yes, hematologists, including those in hematology-oncology, are vital in cancer treatment. They work with leukemia, lymphoma, and multiple myeloma.
References
- National Academies of Sciences, Engineering, and Medicine (NASEM). (2023). Techniques for hematological disorders. In Blood and bone marrow diseases. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK593683/





