Last Updated on October 21, 2025 by mcelik
Sickle cell disease is the most common inherited blood disorder worldwide. It affects millions of people globally. This genetic disorder changes how the body makes hemoglobin, a key protein in red blood cells.
Understanding this condition is vital because it greatly affects patients’ lives. This is true, even more so in areas where healthcare is hard to get. We will look into its symptoms, how it’s passed down, and treatment options. This will help those wanting to learn more about it.
Key Takeaways
- Sickle cell disease is the most common inherited blood disorder globally.
- It is a genetic condition affecting hemoglobin production.
- The disorder significantly impacts patients’ quality of life.
- Understanding its genetics and management is key.
- Access to healthcare is vital in managing the condition.
Understanding Sickle Cell Disease
Sickle cell disease is a genetic disorder that affects how red blood cells carry oxygen. It’s caused by a problem with hemoglobin, a protein in red blood cells. This protein is key for delivering oxygen to the body’s parts.
Definition and Basic Mechanism
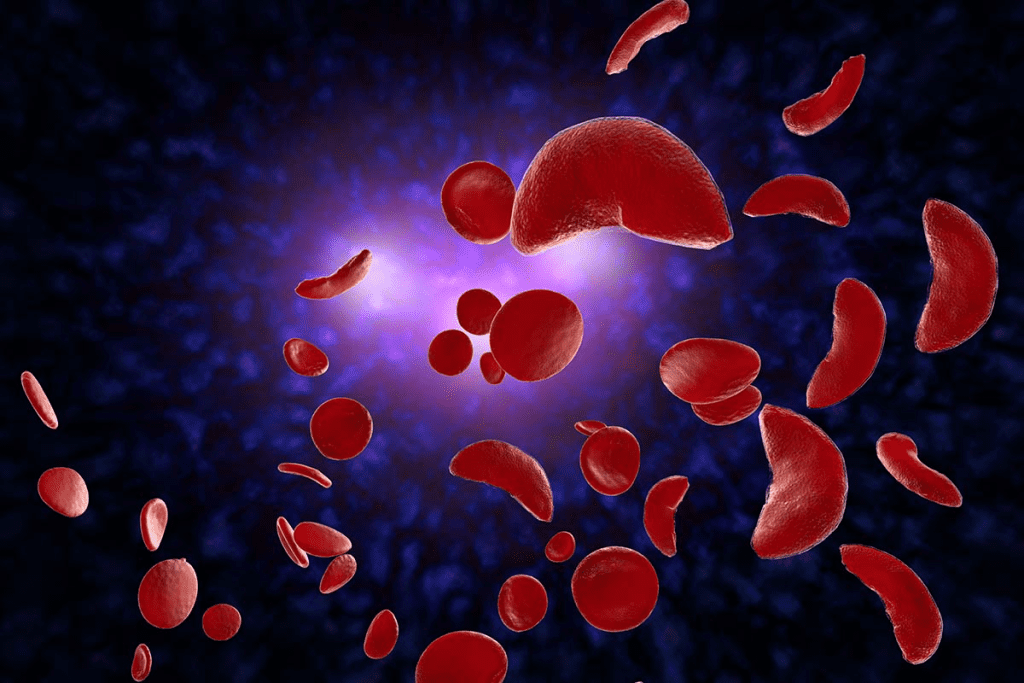
Sickle cell disease is marked by abnormal hemoglobin, called sickle hemoglobin or hemoglobin S. This abnormal hemoglobin makes red blood cells bend into a sickle shape under certain conditions. This shape change can cause health problems like anemia, pain episodes, and increased risk of infections.
The disease starts with a mutation in the HBB gene. This gene is responsible for the beta-globin subunit of hemoglobin. The mutation leads to hemoglobin S, which sticks together under low oxygen. This causes the red blood cells to sickle.
Historical Background
The history of sickle cell disease began in the early 20th century. It was first noted in medical literature back then. Over the years, we’ve learned a lot about its genetic and molecular roots.
| Year | Milestone |
| 1910 | First description of sickle cell disease |
| 1949 | Discovery of the genetic basis of sickle cell disease |
| 1970s | Advances in understanding the molecular mechanisms |
These key moments have helped us understand sickle cell disease better. They’ve also led to new treatments. These include blood transfusions, medications to reduce pain episodes, and emerging gene therapies.
The Prevalence of Sickle Cell Disease
Sickle cell disease is found in different parts of the world. Its spread varies because of genetics and history. The sickle cell gene has been passed down through generations.
Global Distribution
This disease is common in tropical and subtropical areas. It’s found where malaria used to be a big problem. The sickle cell trait helps protect against malaria.
Demographics in the United States
In the U.S., sickle cell disease affects some groups more than others. It’s most common among African Americans. But it also affects Hispanics, people from the Middle East, and South Asia.
About 100,000 Americans have this disease. It affects about 1 in 365 African Americans. Knowing who gets sickle cell disease helps doctors and policymakers. It’s key to improving health for everyone.
Genetics of Sickle Cell Disease
Learning about the genetics of sickle cell disease is key. It helps us understand how it’s passed down and how it affects people. Sickle cell disease is a genetic disorder that messes with hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen.
Inheritance Patterns
Sickle cell disease follows an autosomal recessive pattern. This means a person needs two defective hemoglobin genes, one from each parent, to have the disease. If someone has only one defective gene, they can carry the disease but usually don’t show symptoms.
People who carry the disease are called carriers. They often live normal lives but can pass the defective gene to their kids. If both parents are carriers, there’s a 25% chance with each child that they’ll get sickle cell disease.
| Parental Status | Chance of Child Having Sickle Cell Disease | Chance of Child Being a Carrier |
| Both parents are carriers | 25% | 50% |
| One parent is a carrier, the other has sickle cell disease | 50% | 50% |
| Both parents have sickle cell disease | 100% | 0% |
Genetic Mutations
The genetic mutation causing sickle cell disease affects the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. The mutation leads to abnormal hemoglobin, known as sickle hemoglobin or HbS.
This abnormal hemoglobin causes red blood cells to bend into a sickle shape. This happens under low oxygen levels.
A leading geneticist explains, “The mutation in the HBB gene changes glutamic acid to valine at the sixth position of the beta-globin chain. This causes red blood cells to sickle.”
“The genetic basis of sickle cell disease is well understood, and ongoing research into gene therapy offers promising avenues for future treatment options.”
Knowing the genetics of sickle cell disease helps in diagnosing and managing it. It also opens doors for genetic counseling and future gene therapies.
Sickle Cell Trait vs. Sickle Cell Disease
Sickle cell trait and sickle cell disease are two related but different conditions. They both affect how the body makes hemoglobin. But they have different effects on health.
Differences and Similarities
Sickle cell disease is a genetic disorder that causes abnormal hemoglobin. This leads to red blood cells sickling under certain conditions. Sickle cell trait, on the other hand, happens when someone has one normal and one sickle hemoglobin gene. They can pass the sickle gene to their kids but usually don’t show symptoms.
People with sickle cell disease often face severe symptoms like pain and anemia. Those with sickle cell trait usually don’t have these problems. But, they might face health issues in extreme conditions like high altitudes or intense exercise.
Health Implications of Sickle Cell Trait
Even though sickle cell trait is usually harmless, there are some health concerns. For example, it can lead to sickle cell crisis under extreme stress or dehydration. It’s important for those with sickle cell trait to know these risks and take steps to prevent them.
Also, sickle cell trait can affect family planning. Carriers of the sickle gene should consider the chance of passing it to their kids. This could lead to sickle cell disease if the other parent is also a carrier. So, genetic counseling is advised for those with sickle cell trait planning a family.
For sickle cell treatment and management, people with sickle cell trait usually don’t need as much medical help. But, knowing about the condition is key. Research on sickle cell is ongoing. It might lead to better ways to manage and treat both sickle cell trait and disease.
Pathophysiology of Sickle Cell
Sickle cell disease changes how red blood cells work and affects overall health. It’s a genetic disorder that alters red blood cells’ shape and function. This leads to various health problems.
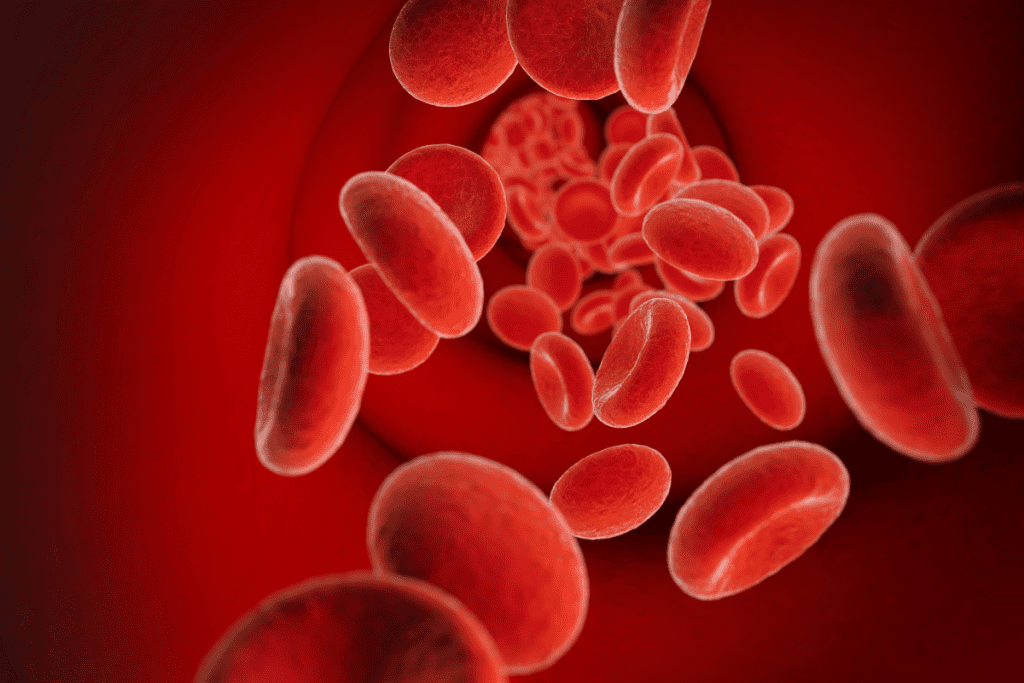
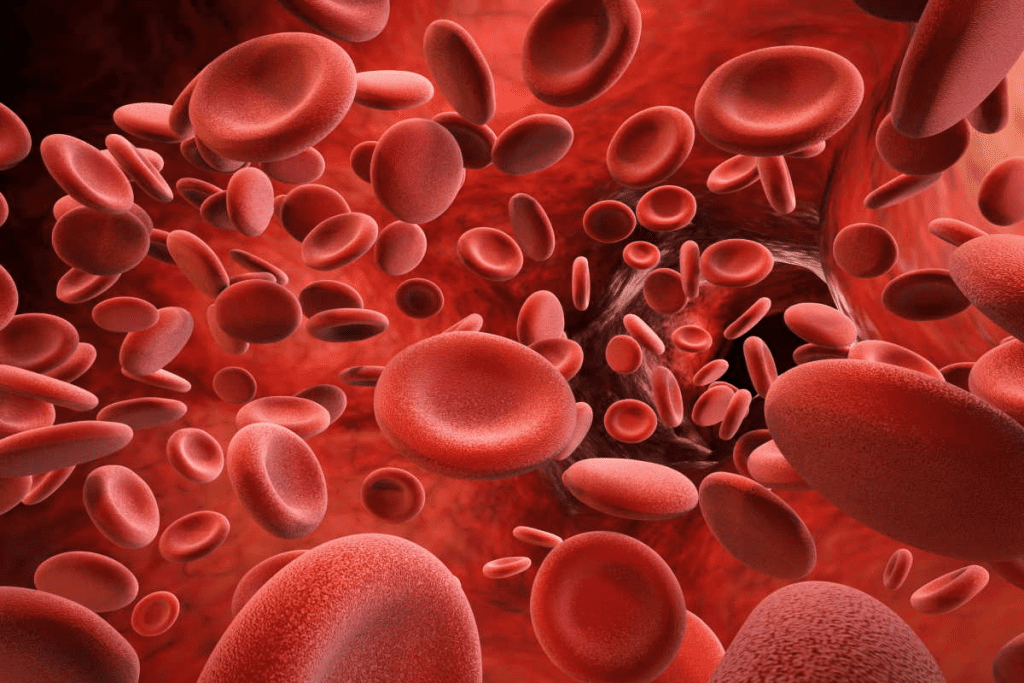
How Normal Blood Cells Work
Normal red blood cells are flexible and carry oxygen around the body. They have a protein called hemoglobin, which is key for oxygen transport. Their flexibility lets them move through small blood vessels, ensuring oxygen reaches everywhere.
How Sickle Cells Form
Sickle cells form from a gene mutation. This mutation creates abnormal hemoglobin, or HbS. When red blood cells with HbS face low oxygen, they change shape to sickle-shaped. These cells are more likely to break down and block small blood vessels.
Effects on Blood Flow and Oxygen Delivery
The stiff sickle cells can block small blood vessels. This reduces blood flow and oxygen to tissues. It can cause tissue damage and pain, known as sickle cell crises. The lack of oxygen can also lead to long-term organ damage.
Key effects of sickle cell disease on blood flow and oxygen delivery include:
- Reduced flexibility of red blood cells, leading to increased risk of blood vessel obstruction.
- Increased risk of pain episodes due to tissue ischemia.
- Chronic organ damage due to repeated episodes of ischemia and infarction.
The pathophysiology of sickle cell disease is complex. It involves genetics, biochemistry, and physiology. Understanding these factors is key to finding effective treatments and management strategies.
Common Symptoms of Sickle Cell Disease
Knowing the symptoms of sickle cell disease is key to better care and outcomes. This genetic disorder affects how red blood cells are made. It leads to cells that are shaped wrong, causing health problems.
Pain Episodes (Sickle Cell Crisis)
Pain episodes, or sickle cell crises, are a major symptom. These happen when sickled cells block blood vessels. This reduces blood flow and oxygen to organs and tissues. The pain can be very bad and unpredictable.
Managing pain episodes often means staying hydrated, taking pain meds, and sometimes needing hospital care. This helps control severe pain and prevent worse problems.
Chronic Complications
People with sickle cell disease face chronic issues too. Anemia is common because sickled cells don’t last long. This leads to tiredness and other signs of low red blood cell count.
They’re also more likely to get infections, like pneumonia, because their spleen doesn’t work right. Regular doctor visits and preventive steps, like vaccines, are important to lower these risks.
Symptoms in Children vs. Adults
Sickle cell disease shows up differently in kids and adults. Kids might first get symptoms like dactylitis, or hand-foot syndrome. This is a painful swelling of the hands and feet.
As kids grow, they face more infections and other problems. Adults often deal with more serious issues, like organ damage and stroke risk. Knowing these differences helps doctors give better care for each age group.
By understanding the symptoms of sickle cell disease and how they differ, doctors can offer better support and treatment plans.
Diagnosing Sickle Cell Disease
Diagnosing sickle cell disease involves several steps. This includes newborn screening and various tests. Early detection is key to managing the disease well.
Newborn Screening
Newborn screening for sickle cell disease is very important. It’s a simple blood test done in the first few days of life. This test looks for abnormal hemoglobin, a sign of the disease.
We suggest that all newborns get this screening. It helps start treatment early. Early detection can lower the risk of complications and improve life quality.
Diagnostic Tests
For those not screened at birth or showing symptoms, several tests can confirm sickle cell disease. These include:
- Hemoglobin Electrophoresis: This test separates blood hemoglobin types to find abnormal ones linked to sickle cell disease.
- High-Performance Liquid Chromatography (HPLC): HPLC measures blood hemoglobin types to detect abnormal ones.
- Genetic Testing: This analyzes genes for hemoglobin to find mutations linked to sickle cell disease. It’s great for confirming diagnosis and finding carriers.
| Diagnostic Test | Purpose | Key Findings |
| Hemoglobin Electrophoresis | Separates different types of hemoglobin | Presence of HbS (sickle hemoglobin) |
| HPLC | Measures different types of hemoglobin | Quantifies HbS and other abnormal hemoglobin |
| Genetic Testing | Analyzes genes for hemoglobin | Identifies mutations associated with sickle cell disease |
Genetic Counseling
Genetic counseling is vital for managing sickle cell disease. It informs families about genetic risks and the condition’s implications for their children. Counselors also discuss family planning and the risks of another child with the disease.
Genetic counseling supports and guides families affected by sickle cell disease. It helps them make informed health and family planning decisions.
Complications of Sickle Cell Disease
Sickle cell disease can cause both sudden and ongoing health problems. These issues can affect many parts of a person’s health. It’s important to manage these problems well to improve life quality for those with this condition.
Acute Complications
Acute complications of sickle cell disease happen suddenly and need quick medical help. Some major acute complications include:
- Pain Crises: These happen when sickled red blood cells block blood vessels. This causes pain and tissue damage.
- Acute Chest Syndrome: A serious condition with chest pain, fever, and breathing problems. It often needs hospital care.
- Splenic Sequestration: Sickled red blood cells pile up in the spleen. This can cause severe anemia and spleen damage.
- Stroke: Sickle cell disease raises the risk of stroke. This is because sickled red blood cells can block brain blood vessels.
Chronic Complications
Chronic complications come from repeated sickling episodes. They can damage organs over time. Some key chronic complications are:
- Organ Damage: Repeated crises can harm organs like the kidneys, liver, and heart.
- Avascular Necrosis: The hip and shoulder joints can suffer from avascular necrosis. This is due to poor blood supply.
- Chronic Anemia: Ongoing hemolysis can cause chronic anemia. This lowers energy and affects overall health.
- Pulmonary Hypertension: High blood pressure in the pulmonary arteries can cause right-sided heart failure.
Managing both acute and chronic complications is key for sickle cell disease care. A team approach is best. This includes regular checks, prevention, and quick action for sudden problems.
Treatment Approaches for Sickle Cell Disease
Treatment for sickle cell disease aims to lessen symptoms and improve life quality. We’ll look at medicines, blood transfusions, and oxygen therapy.
Medications
Medicines are key in managing sickle cell disease. They help with pain, prevent infections, and lower the risk of complications.
Common Medications:
- Hydroxyurea: Helps reduce pain episodes and may cut down on blood transfusions.
- Penicillin: Prevents infections in kids with sickle cell disease.
- Pain-relieving meds: Like NSAIDs or opioids, for pain during crises.
Blood Transfusions
Blood transfusions are vital in managing sickle cell disease. They increase normal red blood cells, lowering complication risks.
| Type of Transfusion | Purpose | Benefits |
| Simple Transfusion | Increase normal red blood cell count | Reduces risk of complications like stroke |
| Exchange Transfusion | Replace sickled red blood cells with normal ones | Reduces risk of iron overload and other complications |
Supplemental Oxygen
Supplemental oxygen is used to boost oxygen to tissues and organs. It’s helpful during crises or when oxygen levels are low.
Understanding these treatments helps healthcare providers tailor plans for each patient. This addresses their unique needs in managing sickle cell disease.
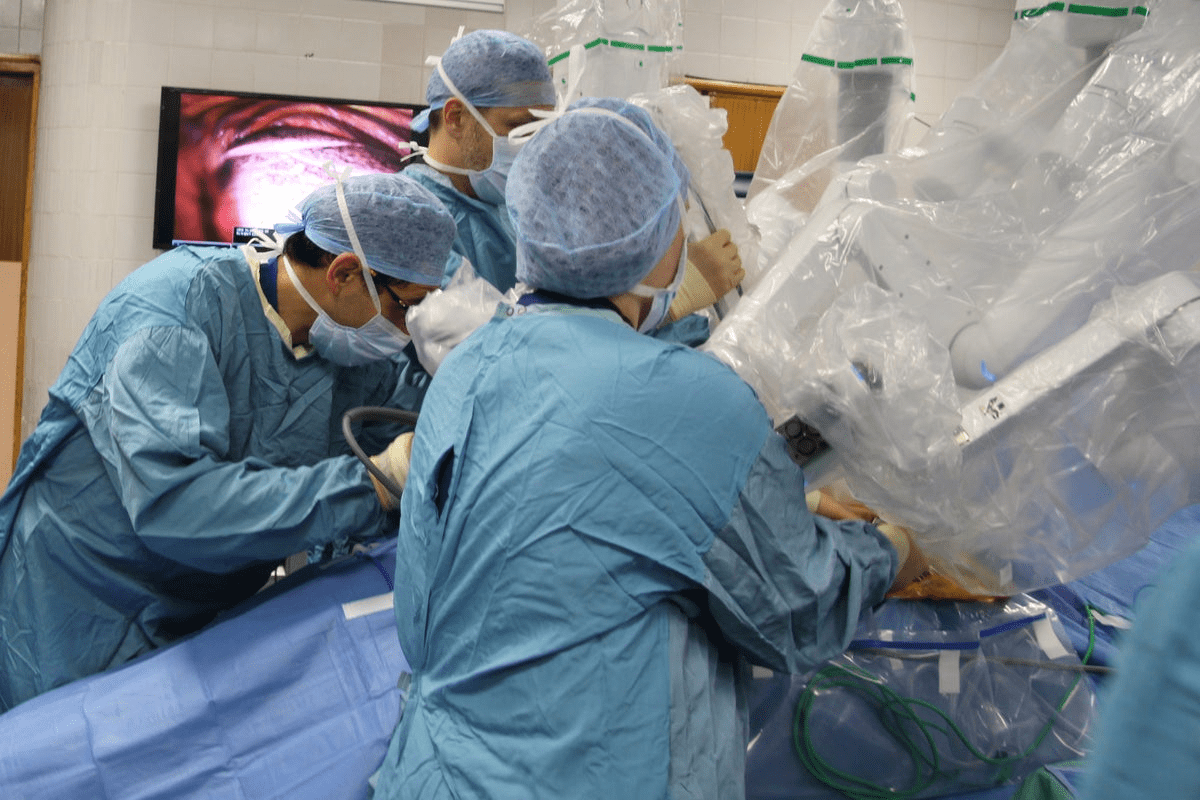
Stem Cell Transplantation and Gene Therapy
For those with sickle cell disease, stem cell transplantation and gene therapy bring new hope. These treatments aim to fix the genetic issue at the root of the disease.
Bone Marrow Transplantation
Bone marrow transplantation is a type of stem cell treatment. It replaces the patient’s bone marrow with healthy marrow from a donor. This could cure sickle cell disease by giving the patient normal hemoglobin-making cells.
The process starts with making the patient’s immune system weak. Then, the donor’s stem cells are infused. While it can cure the disease, it comes with big risks like graft-versus-host disease (GVHD).
| Aspect | Bone Marrow Transplantation | Gene Therapy |
| Procedure | Replacing patient’s bone marrow with donor’s marrow | Modifying patient’s genes to produce normal hemoglobin |
| Risks | GVHD, infection, organ damage | Off-target effects, insertional oncogenesis |
| Benefits | Potential cure, eliminates sickle cell crises | Potential cure, preserves patient’s immune system |
Emerging Gene Therapies
Gene therapy is a new way to treat sickle cell disease. It changes the patient’s genes to make normal hemoglobin. This is done using lentiviral vectors to carry the HBB gene into stem cells.
New gene therapies might avoid the risks of traditional bone marrow transplants. But, they also have their own dangers like off-target effects and insertional oncogenesis.
Research is moving fast, and gene therapies for sickle cell disease are getting better. These treatments give hope for a future where patients can live without this disease’s heavy burden.
Living with Sickle Cell Disease
Living with sickle cell disease can be tough, but making lifestyle changes can help a lot. We’ll look at key changes that can manage the disease well.
Lifestyle Modifications
Changing your lifestyle can make a big difference in managing sickle cell disease. These changes include:
- Dietary Changes: Eating a balanced diet with lots of fruits, vegetables, and whole grains.
- Hydration: Drinking lots of water to stay hydrated and prevent sickle cell crises.
- Exercise: Doing the right physical activities to keep your health up.
Nutrition and Hydration
Nutrition and hydration are key in managing sickle cell disease. A balanced diet keeps you healthy, and enough water prevents dehydration. Dehydration can lead to sickle cell crises.
Important nutritional tips include:
- Eating foods rich in antioxidants, like berries and leafy greens.
- Adding lean proteins like chicken, fish, and beans to your meals.
- Limiting processed foods and sugars.
Exercise Considerations
Exercise is vital in managing sickle cell disease. But, it’s important to know your limits and avoid too much physical activity.
Good exercises are:
- Low-impact activities like walking, swimming, and yoga.
- Stretching exercises to boost flexibility.
It’s also key to listen to your body and rest when needed. Too much activity can lead to a sickle cell crisis.
Managing Sickle Cell Crisis
Managing sickle cell crisis needs a full plan. This includes spotting early signs, using home care, and knowing when to go to the emergency room. A sickle cell crisis happens when sick red blood cells block blood flow. This causes pain and tissue damage.
Recognizing Early Signs
Spotting a sickle cell crisis early is key. Common early signs are sudden pain, fever, swelling, and a fast heart rate. Knowing your normal health helps you notice when something is off.
Home Management Strategies
Home care for sickle cell crisis is important. Drinking lots of water helps prevent dehydration. Pain relief meds are also key, as prescribed by a doctor. Rest and avoiding hard activities also help.
- Stay hydrated by drinking plenty of water
- Use pain relief medications as prescribed
- Get plenty of rest
- Avoid strenuous activities
When to Seek Emergency Care
Some sickle cell crisis needs urgent medical help. Severe pain not helped by home care, trouble breathing, high fever, and signs of infection mean you should go to the emergency room. Also, seek help for chest pain, severe headache, or changes in the brain.
Knowing the early signs, using home care, and knowing when to go to the emergency room helps manage this serious condition. This way, patients and their caregivers can handle it better.
Sickle Cell Disease in Pregnancy
Women with sickle cell disease face higher risks during pregnancy. They need special care. Pregnancy can cause problems for both the mother and the baby.
Risks and Complications
Pregnancy can lead to sickle cell crises, pre-eclampsia, and other issues. The risk of maternal mortality is higher. Babies may face growth restriction and preterm birth.
Management During Pregnancy
Managing sickle cell disease in pregnancy requires a team effort. It’s important to monitor both the mother and the fetus closely. This includes regular blood tests and fetal ultrasounds.
Using prophylactic blood transfusions can help prevent sickle cell crises. Keeping the mother healthy through good nutrition and hydration is also key. Pregnant women with sickle cell disease should stay in close contact with their healthcare providers.
Advances in Sickle Cell Research
The field of sickle cell disease research has seen big breakthroughs. These breakthroughs are leading to new treatments and better care for patients. They offer hope to those affected by this condition.
Recent Breakthroughs
Recently, we’ve made great strides in understanding sickle cell disease. Gene editing technologies like CRISPR/Cas9 are showing promise in curing the disease. Researchers are also finding new ways to treat symptoms and complications.
Some key breakthroughs include:
- Advances in gene therapy: Scientists are working on changing genetic material in cells to fight disease.
- Improved pain management: New treatments are being developed to better handle pain crises.
- Enhanced understanding of disease complications: Research is helping us understand complications better, leading to better treatments.
Promising Clinical Trials
There are many clinical trials looking at new treatments for sickle cell disease. These trials are important for bringing research to practice. Some promising areas include:
- Gene therapy trials: Trials are exploring gene therapy as a cure for sickle cell disease.
- Novel pharmacological agents: New drugs are being tested to reduce pain crises and other complications.
- Hematopoietic stem cell transplantation: Trials are looking at stem cell transplants as a cure.
Future Treatment Directions
As research keeps advancing, we’ll see even better treatments for sickle cell disease. Future directions include:
- Personalized medicine approaches: Treatments will be tailored to each patient based on their genetic profiles.
- Combination therapies: Using multiple treatments together for better results.
- Regenerative medicine: Exploring therapies to repair or replace damaged tissues and cells.
These advances in sickle cell research are bringing us closer to a future where patients can live healthier lives. As we keep pushing the boundaries of medical knowledge and technology, the outlook for improving patient outcomes is brighter than ever.
Support Resources for Patients and Families
Sickle cell disease needs more than just medical care. It also needs a strong support network. This network is available through many resources. It helps manage the disease by treating symptoms and supporting overall well-being.
Organizations and Support Groups
Many organizations and support groups help those with sickle cell disease. They offer a place to share experiences and get emotional support. For example, the Sickle Cell Disease Association of America provides support through advocacy, education, and research funding.
Support groups, both in-person and online, are key. They connect people with others who face similar challenges. These groups reduce feelings of loneliness and offer a community to share and learn from each other.
Educational Resources
Understanding sickle cell disease is important for patients and families. Organizations like the National Heart, Lung, and Blood Institute offer detailed information. They cover treatment options and lifestyle tips.
There are many educational materials available. These include brochures, online content, workshops, and webinars. They empower patients and families with the knowledge to manage the disease.
Financial Assistance Programs
Dealing with sickle cell disease can be expensive. It includes costs for medications, hospital stays, and treatments. Financial help is available to reduce these costs.
For example, patient assistance programs (PAPs) from pharmaceutical companies can lower medication costs. Non-profit organizations also offer grants and financial aid for medical expenses and travel. It’s important for patients and families to look into these options to manage the financial burden.
Conclusion
Sickle cell disease is a complex condition that needs a lot of care and support. We’ve looked at many parts of the disease, like its genetics and how it’s treated. We’ve also talked about how to manage it.
It’s important for patients, families, and doctors to understand sickle cell disease. A thorough review of the key points emphasizes the importance of continued research and improved patient care strategies for managing sickle cell disease. This helps improve life for those affected.
Looking ahead, keeping up with new research is vital. This includes new gene therapies and stem cell transplants. By doing this, we can give the best care to those with sickle cell disease. This will help them live better lives.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic disorder. It affects the hemoglobin in red blood cells. This makes them misshapen and break down, leading to health problems.
What are the symptoms of sickle cell disease?
Symptoms include pain episodes and anemia. Infections and damage to organs like the kidneys and liver are also common. Children and adults have different symptoms.
How is sickle cell disease inherited?
It’s inherited in an autosomal recessive pattern. A person needs two abnormal hemoglobin genes, one from each parent, to have the disease.
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait means having one abnormal gene. This makes a person a carrier. Sickle cell disease means having two abnormal genes, causing the condition.
How is sickle cell disease diagnosed?
Newborn screening is the first step. Then, tests like hemoglobin electrophoresis or genetic testing confirm the diagnosis.
What are the treatment options for sickle cell disease?
Treatments include medications and blood transfusions. Oxygen therapy and sometimes stem cell transplantation or gene therapy are also used.
How can sickle cell crisis be managed?
Early signs should be recognized. Home management strategies are helpful. Emergency care is needed when necessary.
What lifestyle modifications can help manage sickle cell disease?
Eating a healthy diet and staying hydrated are key. Regular exercise and avoiding extreme temperatures also help manage the condition.
Are there any support resources available for patients and families?
Yes, there are organizations and support groups. Educational resources and financial assistance programs are also available for those affected by sickle cell disease.
What is the current state of research on sickle cell disease?
Research is ongoing. Recent breakthroughs and clinical trials offer hope for new treatments and possibly a cure.
Can sickle cell disease be cured?
Currently, stem cell transplantation is the only cure. Gene therapy is being researched as a possible future treatment.
References
Lippi, G., & Mattiuzzi, C. (2020). Updated Worldwide Epidemiology of Inherited Erythrocyte Disorders. Acta Haematol, 143(3), 196-203.