Last Updated on October 21, 2025 by mcelik
Blood coagulation disorders, also known as coagulopathies, affect millions worldwide. These conditions make it hard for the body to form clots. This can lead to either too much bleeding or clotting. We will dive into the details of these disorders and their importance in public health.Our essential guide to any coagulation disease of blood reveals powerful facts. Learn about the most common disorders and their critical treatments.
Coagulopathy, a term for these disorders, includes many conditions that can be deadly if not managed right. It’s important to understand the basics of blood coagulation disorders to grasp their complexity.
Key Takeaways
- Coagulopathy refers to conditions that affect blood clotting.
- Blood coagulation disorders can lead to excessive bleeding or clotting.
- Understanding coagulopathy is key to managing these conditions.
- Coagulation disorders have a big impact on public health.
- Proper management of coagulopathy can save lives.
The Physiology of Blood Clotting

Understanding blood clotting is key to diagnosing and treating coagulation disorders. It involves many cells and proteins working together. They prevent too much bleeding when a blood vessel is hurt.
The Coagulation Cascade
The coagulation cascade is a series of chemical reactions that lead to clot formation. It includes clotting factors, proteins in the blood. These factors are labeled with Roman numerals (I through XIII) and have specific roles.
There are two main pathways: the intrinsic and extrinsic. The intrinsic pathway is triggered by damage inside the blood vessel. The extrinsic pathway is caused by external trauma that makes blood spill out.
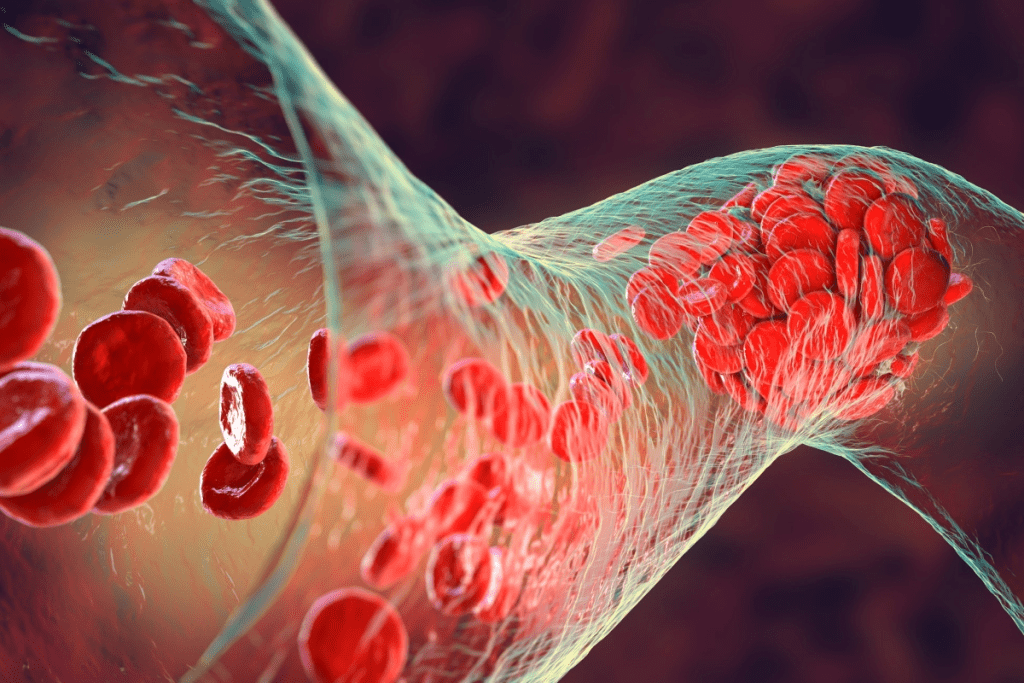
These pathways merge into a common pathway. This leads to the creation of a fibrin clot. This clot is vital for keeping the platelet plug in place until the injury heals.
Platelets and Their Role
Platelets are key in starting the blood clotting process. When a blood vessel is damaged, platelets stick to the exposed tissue. They become activated and release signals that attract more platelets.
This forms a platelet plug that temporarily seals the damaged vessel. Platelets also provide a surface for the coagulation cascade to continue. This helps generate thrombin and fibrin.
Clotting Factors and Their Functions
Clotting factors are vital for the coagulation cascade. Each factor has a specific role in clot formation. For example, Factor VIII and Factor IX are important for the intrinsic pathway.
Deficiencies in these factors can cause bleeding disorders like Hemophilia A and B. The right balance of coagulation factors is essential. Defects can lead to clotting factor disorders, causing too much bleeding or inappropriate clotting.
Knowing how blood clotting works is key to diagnosing and treating blood clotting disorders. This knowledge helps in developing treatments for these disorders.
Coagulation Disease of Blood: Classification and Overview
Coagulopathy is a big deal in healthcare. It’s when blood doesn’t clot right, leading to too much bleeding or clots where they shouldn’t be. Knowing about these issues is key to treating them well.
Defining Coagulopathy
Coagulopathy means blood can’t clot well, making it hard to stop bleeding. It can happen for many reasons, like not enough clotting factors or problems with platelets. Finding out why is the first step to helping someone.
Hypocoagulable vs. Hypercoagulable States
Blood coagulation disorders fall into two main groups: hypocoagulable and hypercoagulable. Hypocoagulable means blood can’t clot, raising the risk of bleeding. Hypercoagulable means blood clots too easily, which can block blood vessels.
Hypocoagulable problems usually come from not enough clotting factors. Hypercoagulable issues might be genetic or caused by other factors. We must diagnose and treat these carefully to avoid bad outcomes.
Global Prevalence and Impact
Coagulation disorders affect millions worldwide, causing a lot of sickness, death, and cost. The number of people with conditions like hemophilia and von Willebrand disease varies. Knowing this helps plan for public health and resources.
These disorders don’t just hurt the person who has them. They also affect their families and the healthcare system. We need to improve how we find and treat these conditions to help everyone.
Hemophilia: A Major Bleeding Disorder
Hemophilia is a serious bleeding disorder found worldwide. It affects many people, impacting their quality of life. It happens when certain clotting factors are missing, which are key for blood to clot.
Factor VIII Deficiency: Hemophilia A
Hemophilia A, or classic hemophilia, is due to a lack of factor VIII. It’s the most common type and mainly affects males. The severity can vary, from mild to severe bleeding episodes.
Symptoms include prolonged bleeding after injuries and spontaneous bleeding in joints or muscles. Easy bruising is also common. Doctors diagnose it through tests that check factor VIII levels.
Factor IX Deficiency: Hemophilia B
Hemophilia B, or Christmas disease, is caused by a lack of factor IX. It also mainly affects males and is inherited in an X-linked recessive pattern. Symptoms are similar to Hemophilia A, including prolonged bleeding and joint damage.
Diagnosis involves measuring factor IX levels. Treatment aims to replace the missing factor IX to prevent or manage bleeding.
Factor XI Deficiency: Hemophilia C
Hemophilia C is a rare disorder due to a lack of factor XI. It affects both males and females, unlike Hemophilia A and B. Symptoms can be mild and not always obvious, making diagnosis hard.
Tests that check factor XI activity diagnose it. Treatment focuses on controlling bleeding, often with fresh frozen plasma or factor XI replacement.
It’s important to understand the different types of hemophilia and their causes. This helps healthcare providers give the right care. Understanding specific clotting factor deficiencies enables the creation of tailored treatment plans for each patient’s needs.
Von Willebrand Disease: The Most Common Inherited Bleeding Disorder
Von Willebrand disease is the most common inherited bleeding disorder. It happens when there’s not enough or working von Willebrand factor. This protein is key for blood clotting and sticking platelets together. We’ll look at its types, symptoms, and how hard it is to diagnose.
Types of Von Willebrand Disease
Von Willebrand disease has different types based on how much or how well von Willebrand factor works.
- Type 1: This is the most common and mild form, with a partial lack of von Willebrand factor.
- Type 2: This type has a qualitative defect in von Willebrand factor, causing it to not work right.
- Type 3: The most severe form, with no von Willebrand factor at all.
Clinical Manifestations
The symptoms of von Willebrand disease vary a lot. Common signs include:
- Easy bruising
- Nosebleeds
- Heavy menstrual bleeding in women
- Bleeding after surgery or dental procedures
These symptoms can really affect someone’s life, making it important to manage and treat them well.
Diagnostic Challenges
It’s hard to diagnose von Willebrand disease because it can show up differently in people. It also shares symptoms with other bleeding disorders.
- Medical history and physical examination
- Laboratory tests to measure von Willebrand factor levels and function
- Genetic testing in some cases
Here’s a quick look at the types of von Willebrand disease and what they mean:
| Type | Description | Severity |
| Type 1 | Partial deficiency of von Willebrand factor | Mild |
| Type 2 | Qualitative defect in von Willebrand factor | Moderate to Severe |
| Type 3 | Complete deficiency of von Willebrand factor | Severe |
Knowing how von Willebrand factor works helps us understand von Willebrand disease better.
We’ve covered the key points about von Willebrand disease. This includes its types, symptoms, and the challenges in diagnosing it. With this knowledge, doctors can better care for those with this condition.
Thrombophilia: Disorders of Excessive Clotting
Understanding thrombophilia is key to spotting those at risk of dangerous blood clots. Thrombophilia, or hypercoagulability, means a higher chance of blood clots. This can cause serious problems like deep vein thrombosis (DVT) and pulmonary embolism (PE).
Genetic mutations and deficiencies lead to thrombophilia. We’ll look at major factors like Factor V Leiden Mutation, Prothrombin G20210A Mutation, and Protein C, Protein S, and Antithrombin deficiencies.
Factor V Leiden Mutation
The Factor V Leiden mutation is a common cause of thrombophilia. It changes the factor V gene, making it hard for activated protein C to stop it. This leads to more blood clots. People with this mutation are at higher risk of DVT and PE, mainly during surgery or pregnancy.
Prothrombin G20210A Mutation
The Prothrombin G20210A mutation is another big factor in thrombophilia. It causes more prothrombin, a clotting factor, leading to a higher risk of blood clots. Like Factor V Leiden, it’s more common in Europeans and raises the risk of venous thromboembolism.
Protein C, Protein S, and Antithrombin Deficiencies
Deficiencies in natural anticoagulants like Protein C, Protein S, and Antithrombin are also key in thrombophilia. These proteins help control clotting, preventing too much clotting. Deficiencies, often inherited, increase the risk of blood clots. For example, Protein C deficiency can cause severe clotting and bleeding in its homozygous form.
Thrombophilia affects people differently, with some getting clots often and others not at all. Knowing about these conditions helps in managing and preventing them.
It’s also important to remember that sex can affect bleeding risk in thrombophilia. Some studies show differences in clotting risks between men and women, influenced by hormones.
Rare Factor Deficiencies and Combined Disorders
We face rare factor deficiencies and combined disorders in coagulation disorders. These are less common but need a deep understanding for diagnosis and treatment.
Factors I, II, V, VII, X, and XIII Deficiencies
Deficiencies in clotting factors like fibrinogen (Factor I) and prothrombin (Factor II) can cause serious bleeding. Each deficiency has its own symptoms and treatment plans.
For example, Factor XIII deficiency makes fibrin unstable, leading to delayed bleeding. Factor VII deficiency can cause bleeding in the skin and mucous membranes, and in severe cases, it can be life-threatening.
Combined Factor Deficiencies
Combined factor deficiencies add complexity to coagulation disorders. They can come from genetic mutations or acquired conditions that affect several clotting factors.
For instance, deficiencies in vitamin K-dependent clotting factors (like Factors II, VII, IX, and X) can happen due to vitamin K deficiency or warfarin use. Managing these cases requires a detailed approach, focusing on the cause and providing supportive care.
Bernard-Soulier Syndrome and Glanzmann Thrombasthenia
Bernard-Soulier Syndrome and Glanzmann Thrombasthenia are rare inherited disorders affecting platelet function. Bernard-Soulier Syndrome causes thrombocytopenia, giant platelets, and poor platelet adhesion due to defects in the glycoprotein Ib-IX-V complex.
Glanzmann Thrombasthenia is caused by problems with the glycoprotein IIb/IIIa complex, which is key for platelet aggregation. Both conditions can lead to severe bleeding, requiring specific treatment plans that may include platelet transfusions.
It’s vital to understand these rare conditions to provide the best care. By knowing the unique traits of each, we can create targeted treatments to improve patient outcomes.
Acquired Coagulation Disorders
Acquired coagulation disorders are complex and need a deep understanding. They develop over time due to different factors. This makes them different from inherited bleeding disorders.
Vitamin K Deficiency
Vitamin K is key for making clotting factors in the liver. It helps make factors II, VII, IX, and X, and proteins C and S. Without enough vitamin K, blood clotting can be poor, leading to more bleeding.
Causes of vitamin K deficiency include:
- Nutritional deficiencies
- Malabsorption due to gastrointestinal disorders
- Use of certain medications, such as antibiotics and anticoagulants
We find vitamin K deficiency through tests like prothrombin time (PT) and international normalized ratio (INR). Treatment is vitamin K supplements, which quickly fixes the problem.
“Vitamin K is essential for the gamma-carboxylation of clotting factors, and its deficiency can lead to significant bleeding complications.”N Engl J Med
Liver Disease and Coagulation Impairment
The liver makes clotting factors and controls coagulation. Liver disease can mess with coagulation because of less clotting factors and fewer platelets.
| Liver Disease | Coagulation Impairment |
| Cirrhosis | Decreased clotting factor production |
| Acute liver failure | Impaired coagulation regulation |
We treat coagulopathy in liver disease with clotting factor replacement and fixing the liver issue.
Disseminated Intravascular Coagulation (DIC)
DIC is when there’s too much clotting and bleeding all over. It’s caused by a coagulation system imbalance.
Causes of DIC include:
- Sepsis
- Cancer
- Trauma
We find DIC through tests like platelet count, PT, and fibrinogen levels. Treatment aims at the cause and managing bleeding and clots.
Medication-Induced Coagulopathies
Some medicines can cause coagulopathies by affecting clotting or platelets.
Examples include:
- Anticoagulants, such as warfarin and direct oral anticoagulants (DOACs)
- Antiplatelet agents, such as aspirin and clopidogrel
We handle medication-induced coagulopathies by changing or stopping the medicine. Sometimes, we use reversal agents.
In conclusion, acquired coagulation disorders are complex and need a full understanding for good care. Knowing their causes and signs helps us help patients better.
Diagnostic Approaches for Blood Coagulation Disorders
Getting a correct diagnosis is key to managing blood coagulation disorders well. Doctors use a mix of clinical checks, lab tests, and genetic tests to find these conditions. We’ll look at how these methods help identify and treat blood coagulation disorders.
Screening Tests: PT, PTT, INR
Screening tests are the first step in finding coagulation disorders. The prothrombin time (PT) shows how long it takes for blood to clot. It checks the extrinsic and common coagulation pathways. The partial thromboplastin time (PTT) looks at the intrinsic and common pathways. The international normalized ratio (INR) is a PT-based measure, mainly for warfarin monitoring. These tests give a first look at a patient’s clotting status.
Understanding specific clotting factor deficiencies enables the creation of tailored treatment plans for each patient’s needs.
Understanding specific clotting factor deficiencies enables the creation of tailored treatment plans for each patient’s needs.
Genetic Testing and Family Screening
Genetic testing is vital for inherited coagulation disorders. It finds specific mutations, like those causing hemophilia or von Willebrand disease. Family screening is also key. It spots carriers and affected family members, leading to early action and planning.
Point-of-Care Testing Advancements
New point-of-care testing (POCT) has made diagnosing coagulation disorders easier. POCT devices can check PT/INR right at the patient’s side. This gives quick results for immediate treatment decisions, which is great in emergencies or for long-term anticoagulation therapy.
Clinical Presentation of Bleeding Disorders
It’s key to know how bleeding disorders show up to manage them well. These disorders can affect different parts of the body. This impacts patients’ lives a lot. We’ll look at how they can show up, like in the skin, joints, brain, and after surgery or injuries.
Mucocutaneous Bleeding
Mucocutaneous bleeding is common in bleeding disorders, like von Willebrand disease. It happens in the skin and mucous membranes. Symptoms include easy bruising, nosebleeds (epistaxis), and bleeding gums. Women might also have heavy menstrual bleeding (menorrhagia), which can really affect their life.
Joint and Muscle Bleeding
Hemophilia, a severe disorder, causes bleeding in joints and muscles. This can lead to chronic joint pain, swelling, and limited mobility. Muscle bleeding causes a lot of pain. If not treated, joints can get damaged and disabled.
Intracranial Hemorrhage
Intracranial hemorrhage is a serious issue in bleeding disorders. It’s when blood bleeds into the skull. This can cause brain damage and even death. Quick diagnosis and treatment are vital to avoid brain damage and save lives.
Post-Surgical and Traumatic Bleeding
People with bleeding disorders face higher risks of bleeding after surgery or injuries. Post-surgical bleeding is hard to manage and might need special care. Traumatic bleeding in these patients can be severe and last longer. It needs quick and effective treatment to avoid serious problems.
In summary, bleeding disorders show up in many ways. Knowing these signs is key to giving the right care. By understanding these different bleeding types, doctors can help patients better.
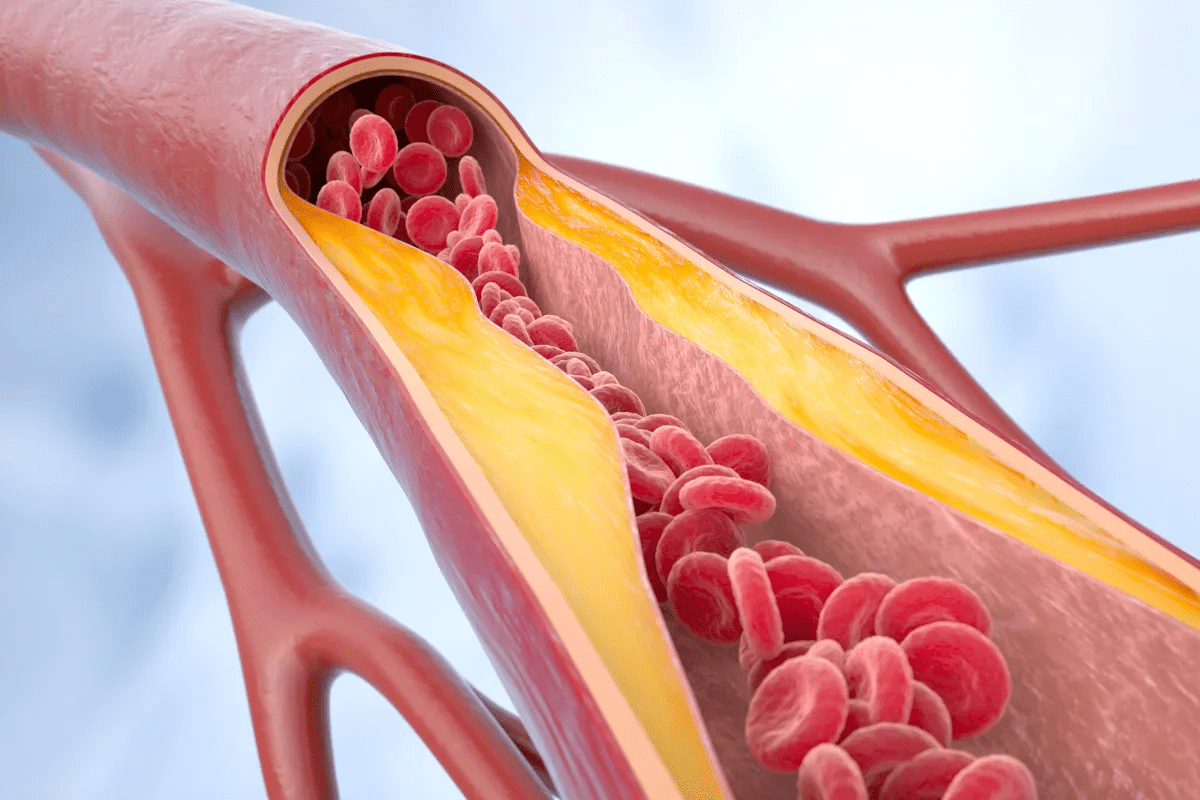
Clinical Presentation of Thrombotic Disorders
It’s important to know how thrombotic disorders show up. These disorders happen when blood clots too much or in the wrong places. They can affect different parts of the body.
Deep Vein Thrombosis
Deep Vein Thrombosis (DVT) is when a blood clot forms in deep veins, usually in the legs. You might feel swelling, pain, and warmth in the leg. Things that increase your risk of DVT include being stuck in one place for a long time, having surgery, and having a family history.
Pulmonary Embolism
Pulmonary Embolism (PE) is when a clot breaks loose and goes to the lungs. It can block blood flow. Symptoms can be mild, like shortness of breath, or severe, like chest pain and sudden death. How bad PE is depends on the size and where the clot is.
Arterial Thrombosis
Arterial thrombosis is when clots form in arteries. This can cut off blood to important organs. Symptoms vary based on where the clot is and can include stroke, heart attack, or problems with limbs. It’s often linked to atherosclerosis.
Recurrent Pregnancy Loss
Recurrent Pregnancy Loss (RPL) can be caused by thrombotic disorders, like antiphospholipid syndrome. Clots in the placenta can cause pregnancy problems, like miscarriage and slow growth of the fetus.
The table below shows how different thrombotic disorders present:
| Condition | Common Symptoms | Risk Factors |
| Deep Vein Thrombosis | Swelling, pain, warmth in the affected limb | Prolonged immobilization, surgery, genetic predispositions |
| Pulmonary Embolism | Shortness of breath, chest pain, sudden death | DVT, immobilization, surgery |
| Arterial Thrombosis | Stroke, myocardial infarction, limb ischemia | Atherosclerosis, hypertension, smoking |
| Recurrent Pregnancy Loss | Miscarriage, fetal growth restriction | Antiphospholipid syndrome, thrombophilia |
Knowing how these disorders show up is key to treating them right. Catching them early can really help patients.
Modern Treatment Approaches for Bleeding Disorders
The treatment for bleeding disorders is getting better with new therapies. These advancements have greatly improved how we manage these conditions. This has led to better lives for those affected.
Factor Replacement Therapies
Factor replacement therapy is key for treating bleeding disorders like hemophilia A and B. It involves giving patients the clotting factor they lack. Recombinant factor products are now the top choice because they are safer and more available. The goal is to keep the factor levels right, stopping or treating bleeding.
Extended Half-Life Products
Extended half-life (EHL) factor products have changed treatment by allowing less frequent injections. This makes treatment easier for patients and could save money in the long run. EHL products work by making the factor last longer in the blood, thanks to new technologies.
Non-Factor Replacement Options
New treatments are coming that don’t use factor replacement. These include monoclonal antibodies and small interfering RNA. These options could make treatment simpler and offer hope for those with inhibitors or other issues.
Gene Therapy: Current Status and Future Prospects
Gene therapy could be a cure for bleeding disorders. It aims to fix the gene problem so the body can make the clotting factor. Early trials show promise, but there are challenges ahead. Despite these, gene therapy is a bright spot for the future of treating bleeding disorders.
In summary, new treatments for bleeding disorders are making a big difference. From factor replacement to gene therapy, there are more options than ever. These advancements are improving lives and giving hope to those affected.
Therapeutic Strategies for Thrombotic Disorders
There are many ways to treat thrombotic disorders. These methods aim to stop clots from forming while avoiding bleeding. Treatments range from medicines to mechanical procedures.
Anticoagulant Medications
Anticoagulants are key in fighting thrombotic disorders. They stop the body’s clotting process. This prevents new clots and stops existing ones from growing. Drugs like warfarin, dabigatran, and rivaroxaban are used.
The right drug depends on the patient’s condition and other factors.
Table: Comparison of Anticoagulant Medications
| Anticoagulant | Mechanism of Action | Monitoring Required |
| Warfarin | Vitamin K antagonist | Yes (INR monitoring) |
| Dabigatran | Direct thrombin inhibitor | No |
| Rivaroxaban | Factor Xa inhibitor | No |
| Apixaban | Factor Xa inhibitor | No |
Antiplatelet Therapy
Antiplatelet therapy is vital for preventing arterial clots. It stops platelets from sticking together. Drugs like aspirin and clopidogrel are used.
Dual antiplatelet therapy combines aspirin with another drug. It’s used for heart attacks or after stent placement.
Thrombolytic Agents
Thrombolytics dissolve clots in emergencies. They are used for strokes, pulmonary embolisms, or heart attacks. Alteplase and tenecteplase are examples.
Mechanical Interventions
Sometimes, mechanical methods are needed. Thrombectomy removes clots. IVC filters prevent pulmonary embolisms in some cases.
Healthcare providers can create personalized treatment plans. This approach improves outcomes for patients with thrombotic disorders.
Living with Coagulation Disorders: Management Strategies
Coagulation disorders need a detailed management plan. This includes prophylactic treatments, tailored physical activity, and nutritional advice. With the right approach, people can reduce risks and live better lives.
Prophylactic Treatment Regimens
Prophylactic treatment is key for managing coagulation disorders, like hemophilia. It involves regular doses of clotting factor concentrates to stop bleeding.
We suggest patients team up with their healthcare provider to create a custom prophylaxis plan. This plan should fit the person’s condition, lifestyle, and bleeding risk.
Physical Activity Guidelines
Exercise is important for health, but it must be safe for those with coagulation disorders. Low-impact activities like swimming, cycling, and yoga are good choices.
We recommend talking to a healthcare provider before starting any new exercise. This makes sure the activities are safe and right for their condition.
Nutritional Considerations
Eating well is essential for those with coagulation disorders. It’s important to keep vitamin K levels up for blood clotting and to get enough other nutrients.
| Nutrient | Role in Coagulation | Food Sources |
| Vitamin K | Essential for blood clotting | Leafy greens, fish, meat |
| Iron | Crucial for healthy red blood cells | Red meat, poultry, beans |
Psychological and Social Support
Dealing with a coagulation disorder can affect mental and social health. Counseling, support groups, and educational resources can help a lot.
We encourage patients to look for these resources and talk openly with their healthcare team about their needs and worries.
Special Populations and Considerations
Exploring coagulation disorders, we must focus on special populations. Each group faces unique challenges that need specific care plans.
Pediatric Patients
Dealing with coagulation disorders in kids is different. Their bodies react differently to treatments. It’s important to adjust prophylactic treatment regimens based on their age, weight, and activity level.
- Keeping an eye on clotting factor levels is key.
- As kids grow, their doses may need to change.
- Working with pediatric specialists is vital for their care.
Women’s Health Issues
Women with coagulation disorders have special needs, like during pregnancy and menstruation. Menstrual management might include hormonal treatments for heavy bleeding. Pregnancy planning is critical due to the risk of blood clots.
- Assessing the risk of bleeding and blood clots is important.
- Monitoring closely during pregnancy is essential.
- Postpartum care may include blood clot prevention.
Aging with Coagulation Disorders
Older adults with coagulation disorders face extra challenges. They often have other health issues and take many medications, which can lead to drug interactions. Anticoagulant therapy must be closely watched to avoid bleeding or blood clots.
- It’s important to regularly check their medications.
- Watching for signs of bleeding or blood clots is critical.
- Working with geriatric specialists can improve care.
Perioperative Management
Patients with coagulation disorders need careful management before, during, and after surgery. This includes checking the risk of bleeding, managing blood thinners, and ensuring enough clotting factors. Multidisciplinary collaboration is key to good outcomes.
- Before surgery, check the patient’s blood clotting status.
- During surgery, clotting factors might be replaced.
- After surgery, watch for signs of bleeding.
Conclusion: The Future of Coagulation Disorder Management
Coagulation disorders affect how blood clots. Managing these disorders is key to avoiding complications. It also improves life quality for those affected.
New diagnostic tools and treatments have greatly helped patients. Gene therapy and extended half-life factor products are promising. They could change how we manage coagulation disorders.
Research into blood coagulation is ongoing. This will lead to new treatments. Healthcare providers can then offer better care. This will greatly improve the lives of those with coagulation disorders.
FAQ
What is a blood coagulation disorder?
A blood coagulation disorder, also known as coagulopathy, is a condition. It affects how blood clots. This can lead to either too much bleeding or clotting.
What are the main types of coagulation disorders?
There are two main types. Hypocoagulable states increase the risk of bleeding. Hypercoagulable states increase the risk of harmful clots.
What is hemophilia, and how is it treated?
Hemophilia is a bleeding disorder. It’s caused by a lack of specific clotting factors. Treatment includes replacing these factors and new methods like gene therapy.
What is von Willebrand disease?
Von Willebrand disease is the most common inherited bleeding disorder. It’s caused by a lack or dysfunction of von Willebrand factor. This protein is key for blood clotting.
What is thrombophilia?
Thrombophilia is a disorder that leads to too much clotting. It’s often caused by genetic mutations or a lack of natural anticoagulants like protein C and antithrombin.
How are coagulation disorders diagnosed?
Diagnosis includes tests like prothrombin time (PT) and partial thromboplastin time (PTT). It also involves specific factor assays and genetic testing.
What are the clinical manifestations of bleeding disorders?
Bleeding disorders can show as mucocutaneous bleeding or joint and muscle bleeding. They can also cause intracranial hemorrhage or bleeding after surgery or injuries.
How are thrombotic disorders treated?
Treatment for thrombotic disorders includes anticoagulant medications and antiplatelet therapy. It also includes thrombolytic agents and mechanical interventions like thrombectomy.
Can individuals with coagulation disorders lead active lives?
Yes, with proper management, individuals with coagulation disorders can lead active lives. This includes following treatment regimens, staying physically active, and getting nutritional and psychological support.
Are there special considerations for managing coagulation disorders in different populations?
Yes, different populations have unique needs. This includes pediatric patients, women with health issues, aging individuals, and those needing perioperative management. Each group requires a tailored approach.
What is the future of coagulation disorder management?
The future looks bright with ongoing advances. New treatments like gene therapy and emerging options are improving outcomes for those with coagulation disorders.
References
National Bleeding Disorder Foundation. (2004). Types of inheritable blood and bleeding disorders. https://www.bleeding.org/bleeding-disorders-a-z/types