We are dedicated to top-notch healthcare for international patients. Hematopoietic disorders like anemia, sickle cell disease, leukemia, and lymphoma affect millions. Recent studies show the number of hematologic malignancies is growing. In 2019, over 1.34 million new cases were reported globally.
These conditions harm hematopoietic cells, causing health problems. At our institution, we offer cutting-edge treatments and care. Our goal is to help those with hematologic disorders through advanced medical treatments and kindness.
Key Takeaways
- Hematopoietic disorders include anemia, sickle cell disease, leukemia, and lymphoma.
- The global burden of hematologic malignancies is increasing.
- Over 1.34 million new cases were reported worldwide in 2019.
- Hematopoietic cells are affected, leading to various health issues.
- Our institution provides complete care and innovative therapies.
Understanding the Hematopoietic System

It’s key to grasp the hematopoietic system to diagnose and treat related issues. This system is complex and vital for our survival. It produces blood cells that keep us alive.
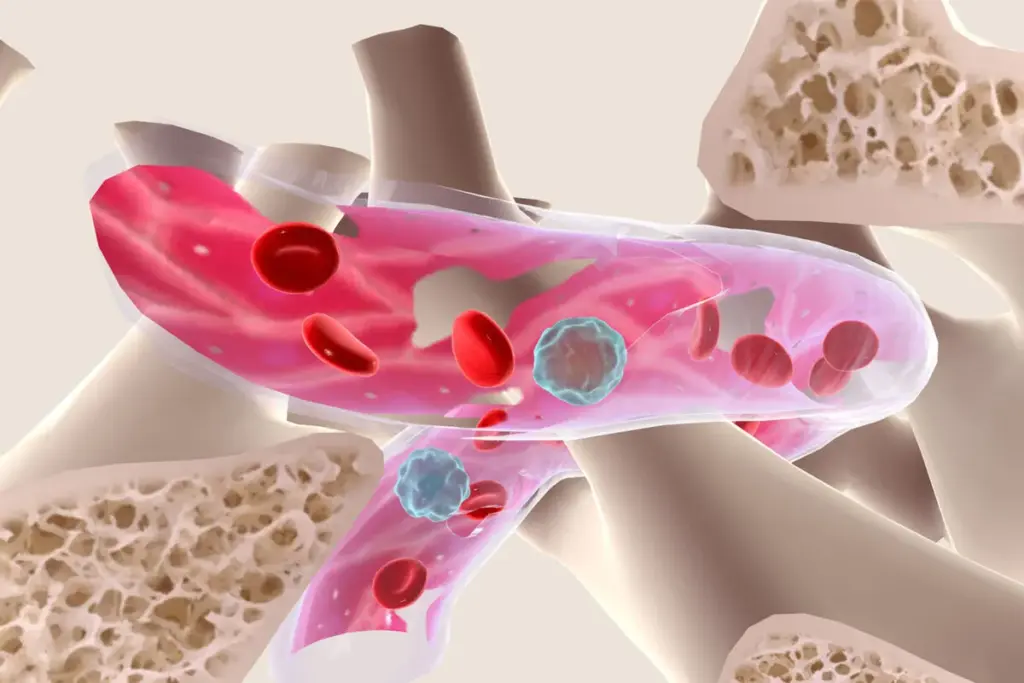
Function and Components of Hematopoietic Tissue
The bone marrow is where the hematopoietic system starts. Here, hematopoiesis, or blood cell production, happens. Stem cells in the bone marrow turn into different blood cells, like red and white blood cells, and platelets.
The main parts of hematopoietic tissue are:
- Stem Cells: These cells are the start of all blood cells.
- Stromal Cells: They help and feed the growing blood cells.
- Blood Vessels: They carry oxygen and nutrients to the bone marrow.
Normal Blood Cell Production Process
Blood cell production, or hematopoiesis, is carefully controlled. It makes sure we have the right blood cells in the right amounts. This process starts with hematopoietic stem cells and ends with mature blood cells.
The blood cell production process has several stages:
- Stem Cell Self-Renewal: Stem cells keep their numbers steady.
- Lineage Commitment: Stem cells decide to become specific blood cells.
- Maturation: Cells become fully functional blood cells in this stage.
Knowing these steps is vital for treating hematopoietic system disorders. At livhospital.com, our team uses the latest medical science to help patients. We aim to improve patient care and outcomes.
The Spectrum of Common Hematopoietic Disorders
Hematopoietic disorders cover a wide range, affecting different cell types and pathways. They are grouped by their causes, symptoms, and genetic roots.
Classification of Blood Disorders
Blood disorders fall into main categories like anemias, leukemias, lymphomas, and myeloproliferative neoplasms. Knowing these groups helps in diagnosing and treating them.
- Anemias: A lack of red blood cells or hemoglobin.
- Leukemias: Cancers of white blood cells.
- Lymphomas: Cancers of the lymphatic system.
- Myeloproliferative neoplasms: Overproduction of blood cells.
For a detailed list of hereditary blood disorders, check out resources on.
Global Epidemiology and Burden
Hematologic malignancies are a big problem worldwide. They affect millions, causing a lot of sickness and death.
|
Condition |
Estimated Global Incidence |
Mortality Rate |
|---|---|---|
|
Leukemia |
437,000 new cases annually |
309,000 deaths annually |
|
Lymphoma |
544,000 new cases annually |
260,000 deaths annually |
|
Anemia |
Affects approximately 1.62 billion people |
Varies based on underlying cause |
The global epidemiology of hematopoietic disorders shows we need more research and better healthcare. Understanding these conditions helps us tackle global health challenges.
Anemia: The Most Prevalent Blood Disorder
Anemia is a common blood disorder that affects many people. It happens when there aren’t enough red blood cells or hemoglobin. This makes it hard for tissues to get enough oxygen.
It can be caused by not getting enough nutrients, chronic diseases, or genetic issues.
Iron Deficiency and Nutritional Anemias
Iron deficiency anemia is the most common type worldwide. It happens when the body doesn’t have enough iron for hemoglobin. Nutritional anemias, like those from vitamin B12 or folate deficiencies, are also common.
These often come from what we eat and can be fixed with better diet and supplements.
Treatment strategies for iron deficiency anemia include iron supplements and diet advice. For nutritional anemias, fixing the nutrient shortage is key.
Hemolytic and Aplastic Anemias
Hemolytic anemia is when red blood cells get destroyed too fast. This can be due to infections, medicines, or autoimmune diseases. Aplastic anemia is when the bone marrow can’t make enough blood cells.
These need different treatments, like medicines to stop the immune system in aplastic anemia.
Understanding the underlying cause is key to treating hemolytic and aplastic anemias well.
Treatment Strategies for Different Anemia Types
Treatment for anemia depends on the cause. For iron deficiency, iron supplements are often used. Nutritional anemias might need vitamin B12 shots or folate pills.
Hemolytic anemia treatment focuses on stopping red blood cell destruction. Aplastic anemia might need immune system suppressors or bone marrow transplants.
- Iron supplements for iron deficiency anemia
- Nutritional counseling for dietary adjustments
- Vitamin B12 injections for vitamin B12 deficiency
- Immunosuppressive therapy for aplastic anemia
We stress the need for personalized care in treating anemia. The best treatment is one that fits the person’s specific needs and condition.
Sickle Cell Disease: A Genetic Hematopoietic Disorder
<image3>
Sickle cell disease affects millions globally. It’s important to understand its causes for better treatment.
Pathophysiology and Genetic Basis
This disease comes from a gene mutation in the HBB gene. This mutation makes sickle hemoglobin (HbS). HbS changes shape in low oxygen, causing red blood cells to curve.
The disease is inherited in an autosomal recessive pattern. People with two copies of the HbS gene (HbS/HbS) have the disease. Those with one copy (HbA/HbS) are carriers and usually don’t show symptoms.
Clinical Manifestations and Complications
Sickle cell disease shows in many ways. Symptoms include pain episodes, anemia, infections, and damage to organs from blocked blood flow.
Complications can be serious. They include:
- Acute chest syndrome
- Stroke
- Splenic sequestration
- Priapism
Management and Emerging Therapies
Managing sickle cell disease involves prevention, treatment, and new treatments. These aim to lessen crisis frequency and improve life quality.
New treatments include:
|
Therapy |
Description |
Benefits |
|---|---|---|
|
CASGEVY |
Gene therapy that edits the HBB gene |
Potential cure by correcting the genetic mutation |
|
ENDARI |
Oral medication that reduces sickle cell crises |
Reduces frequency of painful crises |
|
Hydroxyurea |
Medication that increases fetal hemoglobin production |
Reduces frequency of crises and improves quality of life |
These new treatments are big steps forward. They offer hope for better lives for those with sickle cell disease.
Leukemia: Malignancies of the Hematopoietic System
<image4>
Leukemia is a serious disease that affects the blood-making system. It causes blood cells to grow out of control. This can lead to serious health problems. We will look at the different types of leukemia, how common they are, and what increases the risk of getting them.
Acute Leukemias
Acute leukemias are fast-growing cancers that need quick treatment. They are mainly two types: Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML).
Acute Lymphoblastic Leukemia (ALL) mostly affects kids. It’s caused by too many lymphoblasts. Finding and treating it early is key to survival.
Acute Myeloid Leukemia (AML) is more common in adults. It’s when myeloid cells grow too fast. Treatment often includes strong chemotherapy and sometimes a stem cell transplant.
Chronic Leukemias
Chronic leukemias grow slower and mostly affect adults. The two main types are Chronic Lymphocytic Leukemia (CLL) and Chronic Myeloid Leukemia (CML).
Chronic Lymphocytic Leukemia (CLL) is when lymphocytes build up slowly. Many people don’t show symptoms at first. Treatment starts when symptoms appear.
Chronic Myeloid Leukemia (CML) is when myeloid cells grow too much. Thanks to new treatments, CML is now a manageable condition.
Epidemiology and Risk Factors
Leukemia cases are increasing worldwide. Knowing the causes and risk factors is important for prevention and better treatment.
Things that increase the risk of leukemia include genes, certain chemicals, radiation, and past chemotherapy. Knowing these can help catch and treat leukemia early.
Our understanding of leukemia is growing. New research and treatments give hope for better outcomes for those with this disease.
Lymphoma: Disorders of Lymphoid Tissue
<image5>
Lymphoma is a serious disease that affects the lymphoid tissue. It’s important to know about the different types and how they impact care.
Hodgkin Lymphoma
Hodgkin lymphoma is known for Reed-Sternberg cells. Early diagnosis and treatment have greatly improved survival rates for those with it.
Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma includes many types of lymphoid cancers. Each type needs a specific treatment plan, based on the patient’s condition.
Survival Rates and Prognostic Factors
Thanks to new treatments, survival rates for lymphoma patients have gone up. Factors like age, diagnosis stage, and genetic markers are key in predicting outcomes. Knowing these helps tailor treatments.
Diagnosing and treating lymphoma can be tough. By understanding the types and factors that affect them, doctors can give better care to patients.
Multiple Myeloma: Plasma Cell Proliferation
<image6>
Understanding multiple myeloma means knowing how it affects plasma cells and blood health. This disease is complex. It involves the growth of bad plasma cells in the bone marrow.
Pathogenesis and Molecular Basis
The disease starts with genetic and epigenetic changes. Genetic abnormalities are key in its development. These changes affect how cells grow and survive.
The bone marrow also plays a role. It helps myeloma cells grow by supporting them.
Clinical Features and Complications
Multiple myeloma shows many symptoms. These include bone pain, anemia, kidney problems, and infections. Bone lesions are common, caused by an imbalance in bone cells.
Other issues like high calcium levels, broken bones, and spinal problems can really affect a person’s life. It’s important to watch for these and treat them quickly to help patients.
Current Treatment Paradigms
Treatment for multiple myeloma has gotten better. New drugs and combinations have helped. Proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies have improved results.
Doctors tailor treatments based on the patient. Hematopoietic stem cell transplantation is a chance for a cure for some. But, it’s also important to manage side effects with supportive care.
Clonal Hematopoiesis of Indeterminate Potentia
Clonal hematopoiesis of indeterminate potentia (CHIP) is a condition where hematopoietic stem cells grow with mutations. It’s seen as a step before many blood cancers and disorders.
Age-Related Clonal Expansion
CHIP gets more common with age, linking it to aging. Studies find more mutated stem cells in older people. This might be because of more genetic changes over time.
As we get older, our blood-making system changes. This can lead to CHIP. It’s thought that genetic changes and selection pressures in the blood system cause this.
Clinical Significance and Risks
CHIP raises the risk of blood cancers like myelodysplastic syndromes and acute myeloid leukemia. It also increases the risk of heart disease and death.
Knowing about CHIP’s risks is key to spotting high-risk people. Studies show CHIP can lead to blood cancers. So, it’s important to watch these people closely.
A study on the website sheds light on CHIP’s molecular basis and its implications.
Monitoring and Management Approaches
Managing CHIP means watching for signs of blood cancers and fixing risk factors. Doctors use blood tests and bone marrow checks to keep an eye on CHIP patients.
|
Monitoring Strategy |
Description |
Frequency |
|---|---|---|
|
Complete Blood Count (CBC) |
Measures various components of blood, including white blood cell count. |
Every 6-12 months |
|
Bone Marrow Examination |
Involves the analysis of bone marrow cells to detect abnormalities. |
As clinically indicated |
|
Molecular Testing |
Identifies genetic mutations associated with CHIP and hematologic malignancies. |
At diagnosis and as needed |
Spotting CHIP early and acting fast is key to managing it. By understanding CHIP’s risks and using the right monitoring, we can help those with it.
Myelodysplastic and Myeloproliferative Disorders
It’s important to understand myelodysplastic and myeloproliferative disorders to help patients. These conditions affect how blood cells are made, leading to different symptoms.
Myelodysplastic Syndromes
Myelodysplastic syndromes (MDS) are a group of disorders. They cause problems with blood cell production, leading to low blood counts. This can also increase the risk of developing acute myeloid leukemia (AML).
Key Features of MDS:
- Ineffective hematopoiesis
- Cytopenias (anemia, neutropenia, thrombocytopenia)
- Morphological dysplasia in bone marrow cells
- Risk of progression to AML
|
MDS Subtype |
Characteristics |
Prognosis |
|---|---|---|
|
Refractory Anemia |
Anemia with minimal blasts |
Variable |
|
Refractory Anemia with Excess Blasts |
Increased blasts in bone marrow |
Poor |
Myeloproliferative Neoplasms
Myeloproliferative neoplasms (MPNs) are disorders where blood cells grow too much. The main types are polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
Clinical Features of MPNs:
- Splenomegaly
- Thrombosis and hemorrhage
- Constitutional symptoms
- Risk of transformation to myelofibrosis or AML
Overlap Syndromes and Rare Variants
Some patients have features of both MDS and MPNs, known as MDS/MPN overlap syndromes. Examples include chronic myelomonocytic leukemia (CMML) and atypical chronic myeloid leukemia (aCML).
Characteristics of Overlap Syndromes:
- Mixed features of MDS and MPN
- Variable clinical presentation
- Challenging diagnosis and management
We understand the complexity of these disorders. A detailed approach to diagnosis and treatment is needed. By grasping the specifics of myelodysplastic and myeloproliferative disorders, we can offer better care to our patients.
Diagnostic Approaches for Hematopoietic Disorders
Understanding how to diagnose hematopoietic disorders is key for doctors to care for their patients well. Getting the diagnosis right is the first step to treating a patient effectively.
Complete Blood Count and Peripheral Smear
The first step in diagnosing blood disorders is often a Complete Blood Count (CBC). A CBC shows the health of different blood parts like red and white blood cells and platelets. A peripheral smear also helps by showing the shape and size of blood cells, helping spot problems.
|
Parameter |
Normal Range |
Significance |
|---|---|---|
|
Hemoglobin (Hb) |
13.5-17.5 g/dL (men), 12-16 g/dL (women) |
Low levels indicate anemia |
|
White Blood Cell Count (WBC) |
4,500-11,000 cells/μL |
Abnormal counts suggest infection or leukemia |
|
Platelet Count |
150,000-450,000 platelets/μL |
Low counts may indicate thrombocytopenia |
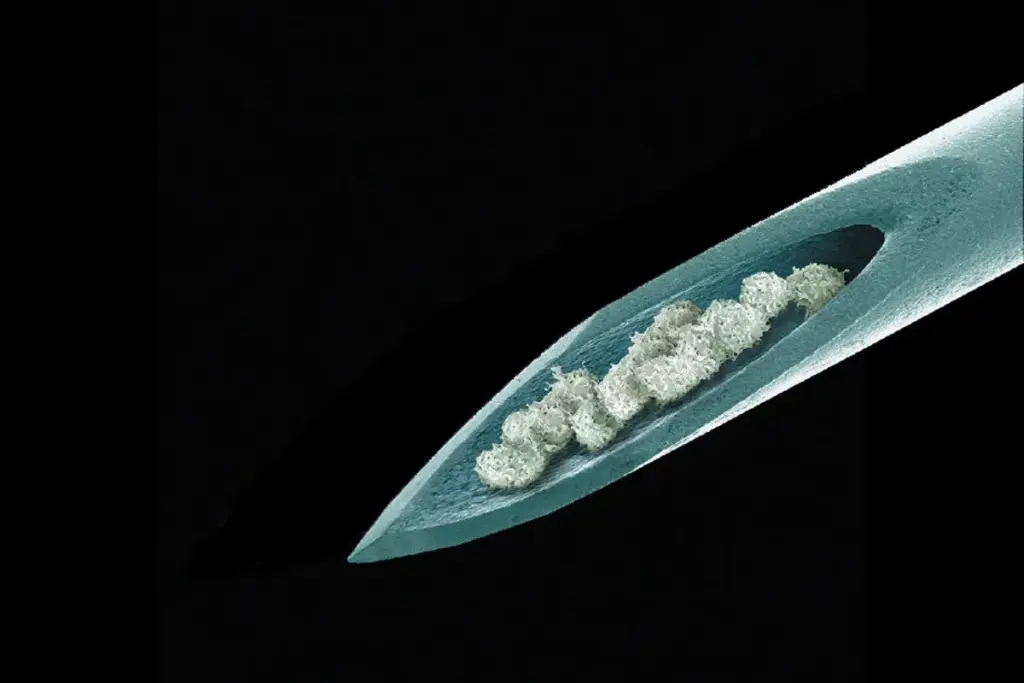
Bone Marrow Examination
A bone marrow examination is a key tool for diagnosing blood disorders. It involves taking a sample from the hip bone. This helps check how blood cells are made and can spot diseases like leukemia.
Molecular and Genetic Testing
Molecular and genetic testing are very important in diagnosing blood disorders. Tests like PCR, FISH, and next-generation sequencing find genetic changes linked to blood diseases. These tests are key for diagnosing conditions like CML and finding disease leftovers.
By using these methods together, doctors can accurately diagnose and treat blood disorders. This leads to better care for patients.
Advanced Treatment Modalities in Hematopoietic Medicine
New treatments are changing how we manage blood disorders. They offer better and more focused ways to help patients. These changes are key to better patient results and a better life for them.
Hematopoietic Stem Cell Transplantation
Hematopoietic stem cell transplantation (HSCT) can cure many blood disorders. This method replaces a patient’s sick blood-making system with healthy stem cells. These stem cells can come from the patient or a donor.
The success of HSCT depends on many things. These include the patient’s health, the disease stage, and how well the donor and patient match. Thanks to better transplant methods and care, more patients are doing well after HSCT.
Targeted Therapies and Immunotherapy
Targeted therapies and immunotherapy are big steps forward. These treatments aim at specific parts of blood disorders. They are often less harsh than old chemotherapy.
Immunotherapy uses the body’s immune system to fight cancer. Monoclonal antibodies, CAR-T cell therapy, and checkpoint inhibitors are some of these treatments. They have greatly helped patients.
Supportive Care Strategies
Supportive care is key in managing blood disorders. It aims to ease symptoms, prevent problems, and improve life quality. It includes preventing infections, blood transfusions, and managing side effects.
Psychosocial support and rehabilitation are also important. They help patients deal with the whole treatment and recovery process.
Prevention and Risk Reduction Strategies
Preventing and reducing risks are key to fighting hematopoietic disorders. We can lessen their impact by understanding what causes them. This way, we can create plans to lower their occurrence and severity.
Genetic Counseling for Hereditary Disorders
Genetic counseling is vital for managing hereditary hematopoietic disorders. It helps figure out the risk of passing on genetic conditions to future generations. It also guides on family planning choices.
For those with a family history of these disorders, genetic counseling is essential. It helps identify those at higher risk. It also gives them the info to make smart health choices.
Key aspects of genetic counseling include:
- Risk assessment for genetic conditions
- Discussion of family planning options
- Guidance on genetic testing
- Support for individuals and families affected by genetic disorders
Lifestyle Modifications and Environmental Factors
Making lifestyle changes and avoiding harmful environments can lower the risk of hematopoietic disorders. This is true for certain types.
|
Lifestyle Modification |
Benefit |
|---|---|
|
Avoiding exposure to toxins |
Reduces risk of aplastic anemia and other bone marrow disorders |
|
Maintaining a balanced diet |
Supports healthy blood cell production |
|
Regular exercise |
Enhances overall health and well-being |
Screening Recommendations
Screening early is key to managing hematopoietic disorders. The right screening depends on age, family history, and other risk factors.
For instance, those with sickle cell disease or other genetic disorders in their family should get screened early. This helps spot those at risk.
By using these prevention and risk reduction strategies, we can lessen the impact of hematopoietic disorders. This improves the lives of those affected.
Living with Chronic Hematopoietic Conditions
Living with chronic hematopoietic conditions is tough. It affects not just the person but their family too. To manage it well, you need good medical care, lifestyle changes, and strong support.
Quality of Life Considerations
Keeping a good quality of life is key for those with chronic conditions. It means getting the right medical care and making lifestyle changes. These changes help reduce the condition’s impact on daily life.
Patients might need to eat healthier, exercise regularly, and find ways to reduce stress. Support from healthcare providers, family, and friends is very important. It helps patients adjust to these changes.
Patient Support Systems and Resources
Patient support systems are essential for those with chronic conditions. These include family, friends, support groups, and online communities. They offer emotional support, practical help, and a sense of connection.
There are also many resources available. These include educational materials, counseling services, and advocacy groups. They help patients understand their conditions, manage symptoms, and navigate the healthcare system.
Navigating Healthcare Systems
Dealing with healthcare systems can be overwhelming. It’s important to know the services available, how to get them, and how to coordinate care.
Patients and caregivers should be able to ask questions, seek second opinions, and fight for the care they need. Using patient navigators or care coordinators can also help manage healthcare complexities.
Conclusion
Hematopoietic disorders cover a wide range of blood and bone marrow issues. These include anemia, sickle cell disease, leukemia, and lymphoma. These conditions can greatly affect a person’s life quality.
Understanding the hematopoietic system and its disorders is key. It helps in diagnosing and treating these conditions effectively.
At livhospital.com, we focus on top-notch healthcare for international patients. Our goal is to offer advanced treatments and caring support for those with hematopoietic disorders. We use the latest research and technology to better patient care.
Improving our knowledge of these disorders is vital. A team effort is needed to manage these complex conditions. Working together, we can find better treatments and improve lives.
FAQ
What are hematopoietic disorders?
Hematopoietic disorders affect how blood cells are made. This includes anemia, sickle cell disease, and leukemia. They impact the body’s ability to make blood cells.
What is the hematopoietic system?
The hematopoietic system is a network of organs that make blood cells. It includes the bone marrow, spleen, and lymph nodes. It’s key for health, helping fight infections and carry oxygen.
What are the symptoms of bone marrow failure?
Symptoms of bone marrow failure may include fatigue, weakness, pale skin, and shortness of breath. Severe cases can lead to anemia and other serious problems.
How are hematopoietic disorders diagnosed?
Doctors use tests like complete blood counts and bone marrow exams to diagnose these disorders. These tests find problems in blood cell production and genetic mutations.
What are the treatment options for hematopoietic disorders?
Treatments vary by disorder. They might include stem cell transplants or targeted therapies. Our team atlivhospital.com helps patients choose the best treatment.
Can hematopoietic disorders be prevented?
Some disorders are caused by genetics, but others can be prevented. Eating well and avoiding toxins can help. Genetic counseling can also identify risk.
How can I manage my quality of life with a chronic hematopoietic condition?
Managing a chronic condition requires a holistic approach. This includes quality of life care and support systems. Our team atlivhospital.com offers personalized support.
What is clonal hematopoiesis?
Clonal hematopoiesis is when a single clone of cells grows in the bone marrow. It raises the risk of disorders. Monitoring and management can prevent complications.
What are myelodysplastic and myeloproliferative disorders?
These disorders affect blood cell production in the bone marrow. They can cause anemia and increase leukemia risk. Symptoms include anemia and thrombocytopenia.
References
- Zhang, N., Wu, J., Wang, Q., Liang, Y., Li, X., Chen, G., Ma, L., Liu, X., & Zhou, F. (2023). Global Burden of Hematologic Malignancies and Evolution Patterns over the Past 30 Years. Blood Cancer Journal, 13(1), 82. https://doi.org/10.1038/s41408-023-00853-3 PubMed+1
- Caiado, F., et al. (2025). Clonal Hematopoiesis: Impact on Health and Disease. Frontiers / PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12167641/ PMC
- ASH Research Collaborative. (2025, June). SCD Data Hub Report 2025. Washington, DC. ASH Research Collaborative. https://www.ashresearchcollaborative.org/wp-content/uploads/2025/06/SCD-Data-Hub-Report-2025.pdf ASH Research Collaborative
- [Author(s)]. (2025). [Title Unknown]. CA: A Cancer Journal for Clinicians. https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21871
- Common Blood Disorders: Causes, Symptoms, and Treatments. (2025, June 9). Comprehensive Hematology & Oncology. https://comphemonc.com/2025/06/09/common-blood-disorders-causes-symptoms-and-treatments/










