Last Updated on October 21, 2025 by mcelik
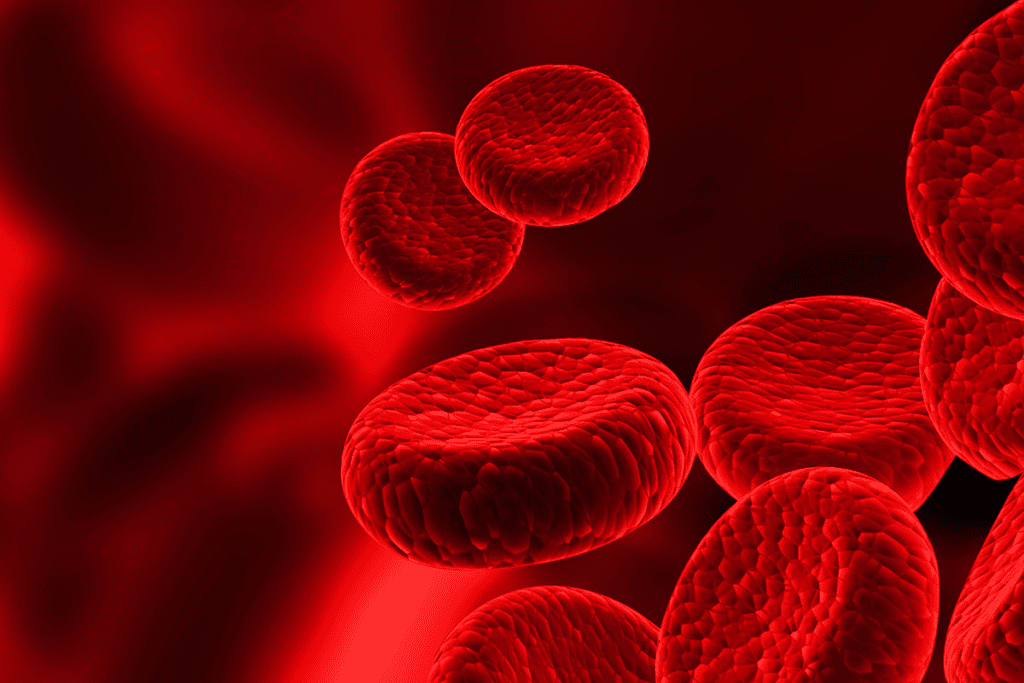
Polycythemia is a rare blood disorder that can lead to serious complications if left untreated. A significant increase in red blood cells can cause the blood to thicken. This leads to a range of symptoms.
Understanding the red flags of this condition is key for early diagnosis and effective management. Symptoms can be subtle. They often include persistent fatigue, headaches, and itching, which get worse after showering or bathing.
Recognizing these red flags early can significantly improve patient outcomes. We will explore the common symptoms and diagnostic approaches to identify polycythemia vera.
Key Takeaways
- Polycythemia vera is a rare blood disorder characterized by excessive red blood cell production.
- Early diagnosis is critical to prevent serious complications.
- Common symptoms include fatigue, headaches, and itching.
- Understanding red flags can improve patient outcomes.
- Diagnostic approaches are essential for identifying the condition.
Understanding Polycythemia Vera: A Blood Disorder Overview

Polycythemia vera is a condition where the bone marrow makes too many blood cells. This includes red blood cells, white blood cells, and platelets. It happens when the bone marrow overproduces these cells, leading to several problems.
What Happens in the Body with Polycythemia Vera
The bone marrow in polycythemia vera makes too many red blood cells, white blood cells, and platelets. This makes the blood thicker and more sticky. It can increase the risk of blood clots and heart problems.
- Increased blood viscosity
- Higher risk of blood clots
- Potential for cardiovascular complications
It’s important to understand how polycythemia vera works. Knowing this helps spot the warning signs early. It also highlights the need for quick medical help.
The Science Behind Polycythemia: Causes and Mechanisms

At the heart of polycythemia vera lies a critical mutation that drives its progression. This condition is a myeloproliferative disorder. It causes too many red blood cells, white blood cells, and platelets. Knowing the causes and mechanisms is key to diagnosing and managing it well.
The JAK2 Mutation: Primary Cause of Polycythemia Vera
The JAK2 mutation is a genetic change that plays a big role in polycythemia vera. The JAK2 V617F mutation changes the JAK2 gene. This change activates a signaling pathway that makes cells grow without normal signals.
Research shows the JAK2 mutation is common in polycythemia vera patients. It’s a key marker for diagnosing the condition. This mutation helps tell polycythemia vera apart from other causes of too many red blood cells.
Secondary Polycythemia vs. Polycythemia Vera
It’s important to know the difference between primary and secondary polycythemia. Both have too many red blood cells, but they have different causes.
| Characteristics | Polycythemia Vera | Secondary Polycythemia |
| Cause | Primary myeloproliferative disorder, often associated with JAK2 mutation | Secondary to another condition (e.g., chronic hypoxia, renal cell carcinoma) |
| Erythropoietin Level | Often low | Often elevated |
| Bone Marrow | Hypercellular with trilineage hyperplasia | Variable, depending on the underlying cause |
Knowing the differences is key for accurate diagnosis and treatment. The difference between polycythemia vera and secondary polycythemia affects treatment plans and patient outcomes.
Early Warning Signs: Recognizing Polycythemia Vera Symptoms
The first signs of polycythemia vera can be hard to spot. They are often vague and not specific. It’s important to catch these signs early to manage the disease well.
Subtle Initial Symptoms Often Overlooked
In the beginning, polycythemia vera shows up with mild symptoms. These can be mistaken for other health issues. Some common early signs include:
- Headaches
- Dizziness or lightheadedness
- Fatigue or weakness
- Itching, often after a warm bath or shower
- Numbness or tingling in the hands and feet
These symptoms are often mild and come and go. This makes it hard for people to see them as serious. But, knowing these signs is key to getting help early.
How Symptoms Progress Over Time
As polycythemia vera gets worse, symptoms get stronger. The disease can cause more red blood cells, leading to serious problems. Symptoms that may get worse include:
| Symptom | Description |
| Enlarged Spleen | The spleen may grow because of too many red blood cells. This can cause pain in the upper left abdomen. |
| Bleeding or Bruising | People might bleed more easily, like from their gums or nose, or bruise easily. |
| Painful Toes or Fingers | Some may feel pain or burning in their toes or fingers, known as erythromelalgia. |
Knowing how polycythemia vera symptoms change is important. Regular check-ups and care can help avoid serious problems. This can also make life better for those with the disease.
Cardiovascular Red Flags in Polycythemia Vera Patients
It’s key to know the heart risks linked to polycythemia vera. This blood disorder ups the chance of heart problems.
Hypertension and Heart-Related Symptoms
Hypertension is a big heart risk with polycythemia vera. High blood pressure can cause chest pain, shortness of breath, and palpitations. Keeping an eye on blood pressure is important to avoid these issues.
The thick blood from too many red blood cells can also harm the heart. This can lead to heart failure if not treated right away. Spotting these signs early is critical for quick action.
Blood Clot Risks and Warning Signs
Blood clots are another big heart risk for those with polycythemia vera. This can cause strokes, heart attacks, and deep vein thrombosis. Knowing the warning signs like swelling, pain, and redness is key.
People with polycythemia vera face a higher risk of blood clots because of the extra red blood cells. To manage this risk, regular checks and sometimes anticoagulant therapy are needed.
In summary, spotting heart risks in polycythemia vera is vital to avoid serious problems. By knowing the signs of hypertension, heart issues, and blood clots, we can handle the condition better and improve patient results.
Neurological Warning Signs of Polycythemia Vera
Polycythemia vera can cause subtle yet significant neurological symptoms. These symptoms can greatly affect a person’s quality of life. It’s important to recognize these signs early to get timely treatment.
Headaches and Visual Disturbances
Headaches are a common symptom of polycythemia vera. They can be mild or severe. Often, these headaches come with visual problems like blurred vision or double vision.
These symptoms suggest increased blood viscosity, a key feature of polycythemia vera. If you have persistent or severe headaches with visual issues, see a doctor right away.
Dizziness, Tinnitus, and Other Neurological Symptoms
People with polycythemia vera may also feel dizzy or have tinnitus. Dizziness can mean less blood flow to the brain, and tinnitus might be due to blood viscosity or pressure changes. Other symptoms include numbness, weakness, and trouble thinking.
It’s vital to watch for these symptoms and tell your doctor. By recognizing these signs early, we can help manage polycythemia vera better. This can lead to better health outcomes for patients.
Skin Manifestations: Visual Red Flags of Polycythemia
Skin signs are key in spotting polycythemia vera early. These signs help doctors diagnose the condition quickly.
Facial Plethora and Skin Redness
Facial plethora is a big sign of polycythemia vera. It makes the face look flushed or reddish. This happens because there’s more red blood cells, making the skin look different.
Facial plethora is often the first thing people notice. It makes them go see a doctor. The redness can be different, and it might itch or feel hot.
Itching (Pruritus) and Other Skin Symptoms
Itching, or pruritus, is another common sign. It can make you feel itchy all over or just in certain spots. It usually gets worse after taking a warm bath or shower.
- Itching can really affect your life, making you uncomfortable and upset.
- You might also feel like your skin is burning or stinging.
- In some cases, you might get aquagenic pruritus, which means itching when you touch water.
Spotting these skin signs early is important. If you notice any, see a doctor right away. They can help figure out what’s going on and treat it.
Gastrointestinal and Abdominal Warning Signs
Polycythemia vera affects blood cells, but it can also cause stomach and abdominal problems. These signs are important and should not be ignored.
Enlarged Spleen (Splenomegaly)
Splenomegaly, or an enlarged spleen, is a common sign of polycythemia vera. The spleen gets bigger because it works harder to clean the blood. This can cause pain in the upper left abdomen that might spread to the back or shoulder.
An enlarged spleen can also make you feel full or uncomfortable after eating. This is because the spleen presses on the stomach. Sometimes, it can even lower the platelet count because it filters more blood cells.
Abdominal Discomfort and Digestive Issues
People with polycythemia vera often have stomach pain and digestive issues. These can be mild or very severe. Symptoms might include bloating, nausea, or changes in bowel movements.
Abdominal pain in polycythemia vera can come from several sources. This includes splenomegaly and other factors like blood clots. To manage these symptoms, a doctor might recommend monitoring, lifestyle changes, and medication.
If you’re experiencing ongoing or severe stomach problems, see your doctor. Early treatment for polycythemia vera can greatly improve your life and lower the risk of serious issues.
Laboratory Abnormalities: Blood Test Red Flags
Blood tests are key to spotting problems linked to polycythemia vera. They help doctors diagnose and keep an eye on the condition.
Elevated Red Blood Cell Count, Hemoglobin, and Hematocrit
Polycythemia vera often shows up in blood tests with too many red blood cells. This means more hemoglobin and hematocrit too. Hemoglobin carries oxygen, and hematocrit shows how many red blood cells you have.
Let’s look at what these numbers usually mean for people with polycythemia vera:
| Parameter | Normal Range | Typical Value in Polycythemia Vera |
| Red Blood Cell Count | 4.32-5.72 million cells/μL (men) | Often above 6 million cells/μL |
| Hemoglobin | 13.5-17.5 g/dL (men) | Often above 18 g/dL |
| Hematocrit | 40-50% (men) | Often above 55% |
Other Blood Test Abnormalities in Polycythemia Vera
Polycythemia vera can also show up in other ways in blood tests. These include:
- White Blood Cell Count: Often high, showing more white blood cells.
- Platelet Count: May be high, raising the risk of blood clots.
- Erythropoietin (EPO) Level: Usually low, as red blood cells are made without EPO.
These signs are important for diagnosing and tracking polycythemia vera. Regular blood tests help doctors adjust treatment plans to control the disease.
Risk Factors: Who Should Be Vigilant About Polycythemia Vera Signs
Polycythemia vera can be influenced by genetics and the environment. Knowing these risk factors helps spot who should watch for signs of this condition.
Age, Gender, and Genetic Predisposition
Age is a big risk factor, with most cases happening between 50 and 70. Men are more at risk than women. Genetic factors, like the JAK2 mutation, also play a big part.
Key Demographic Risk Factors:
| Risk Factor | Description |
| Age | Most diagnoses occur between 50 and 70 years |
| Gender | Men are more likely to develop polycythemia vera |
| Genetic Predisposition | Presence of mutations like JAK2 |
Environmental Factors and Lifestyle Considerations
Some environmental toxins and lifestyle choices might raise the risk of polycythemia vera. The exact ways these factors work are being studied. Knowing them can help prevent the condition.
By knowing these risk factors, people can watch for polycythemia vera signs. They should see a doctor if they notice any symptoms.
Diagnostic Journey: From Suspicion to Confirmation
The journey to diagnose polycythemia vera is complex. It involves several key steps to confirm the blood disorder. We will guide you through the process, from initial suspicion to confirmation. We will highlight the important tests and evaluations involved.
Initial Screening and Blood Tests
The first step in diagnosing polycythemia vera is initial screening and blood tests. These tests are critical for assessing the patient’s condition and identifying red flags.
Blood tests measure red blood cell count, hemoglobin, and hematocrit levels. Elevated levels can indicate polycythemia vera.
| Blood Test Parameter | Normal Range | Polycythemia Vera Indication |
| Red Blood Cell Count | 4.32-5.72 million cells/μL (male) | Elevated above normal range |
| Hemoglobin | 13.5-17.5 g/dL (male) | Higher than normal range |
| Hematocrit | 40-54% (male) | Increased above normal range |
Bone Marrow Biopsy and Genetic Testing
After initial blood tests, further diagnostic procedures may be necessary. A bone marrow biopsy is performed to examine the bone marrow’s cellularity and morphology. This helps confirm the diagnosis.
Genetic testing is also critical. It can identify the JAK2 mutation, a common genetic abnormality associated with polycythemia vera. This test helps differentiate polycythemia vera from other myeloproliferative neoplasms.
Ruling Out Secondary Causes and Other Conditions
An essential part of the diagnostic process is ruling out secondary causes of polycythemia. This includes chronic hypoxia or other underlying conditions that could lead to elevated red blood cell counts. A thorough medical history, physical examination, and additional diagnostic tests are needed.
By systematically evaluating the results of these tests and assessments, healthcare providers can accurately diagnose polycythemia vera. They can differentiate it from other conditions, ensuring appropriate management and treatment.
Complications: When Polycythemia Vera Goes Untreated
If polycythemia vera is not treated, it can cause serious problems. The condition leads to more red blood cells and thicker blood. This can result in severe health issues. We will look at the complications that can happen if this condition is not managed.
Thrombotic Events and Cardiovascular Complications
Untreated polycythemia vera can lead to blood clots. These clots can cause strokes, heart attacks, and other heart problems. These events are very dangerous and need quick medical help. The thick blood also strains the heart, leading to high blood pressure and other heart issues.
People with untreated polycythemia vera are at high risk for blood clots. This includes deep vein thrombosis and pulmonary embolism. These problems can greatly reduce a person’s quality of life. They may need to take blood thinners for a long time to prevent more clots.
Disease Progression to Myelofibrosis or Leukemia
Untreated polycythemia vera can also lead to more serious conditions. This includes myelofibrosis, which scars the bone marrow. It can cause anemia, fatigue, and other issues. Regular monitoring and proper management are key to prevent this.
Some people with polycythemia vera may develop acute myeloid leukemia (AML). AML is a more aggressive disease. It has a worse prognosis, showing the need for careful monitoring and early treatment.
When to Seek Medical Attention: Critical Warning Signs
Certain symptoms need quick action, and knowing them can greatly help polycythemia vera patients. We must watch for critical warning signs that mean we need to see a doctor fast. This can prevent problems and help manage the condition well.
Emergency Symptoms Requiring Immediate Care
Some symptoms are so bad they need quick medical help. These include:
- Severe chest pain or discomfort
- Difficulty breathing or shortness of breath
- Severe headaches or migraines
- Confusion, dizziness, or fainting spells
- Weakness or numbness in the face, arm, or leg
If you or someone you know has any of these emergency symptoms, get medical help right away. Waiting can cause serious problems, like heart issues or brain damage.
| Symptom | Description | Action |
| Severe Chest Pain | Pressure or discomfort in the chest | Seek immediate medical care |
| Difficulty Breathing | Shortness of breath or feeling winded | Seek immediate medical care |
| Severe Headache | Headache that is unusually severe | Seek immediate medical care |
Symptoms Warranting Prompt Medical Consultation
Some symptoms need quick doctor visits, not emergencies. These include:
- Persistent itching or pruritus
- Enlarged spleen or abdominal discomfort
- Unexplained weight loss or fatigue
- Bleeding or bruising easily
If you have any of these symptoms, talk to your doctor. They can check you out and tell you what to do next.
“Early detection and treatment of polycythemia vera can significantly improve patient outcomes and quality of life.” -Medical Expert
Knowing the warning signs and when to see a doctor is key for managing polycythemia vera. Stay alert and talk to your healthcare team if you have any worries.
Living with Polycythemia Vera: Management Strategies
To manage polycythemia vera, a holistic plan is needed. This includes lifestyle modifications and regular health check-ups. It’s key to reduce the condition’s impact and prevent complications.
Lifestyle Modifications and Self-Care
Changing your lifestyle is important for managing polycythemia vera. Eating well and exercising regularly can help. Drinking plenty of water is also vital to avoid dehydration.
Self-care is just as important. Stress management, like meditation or yoga, can help. Avoiding extreme temperatures and keeping a comfortable environment can also ease symptoms.
Long-term Monitoring and Follow-up Care
Regular long-term monitoring is key for managing polycythemia vera. This means frequent blood tests to check red blood cell count and hemoglobin levels. Working with your healthcare provider to adjust your treatment plan is important.
Follow-up care is also vital. It helps catch new or changing symptoms early. Regular visits with your healthcare provider can prevent serious issues like blood clots.
With a complete management plan, people with polycythemia vera can live well. It’s important to stay informed and work with your healthcare team for the best care.
Conclusion:
Living with polycythemia vera means knowing a lot about it and how to manage it. We’ve looked at the signs, causes, symptoms, and how it’s diagnosed. To manage it well, you need to see a doctor quickly, make lifestyle changes, and keep an eye on your health over time. With the right care, people with polycythemia vera can live full and happy lives. It’s key to know about the condition and act fast if you notice symptoms. This way, you can handle your diagnosis and treatment better. We talked about how important it is to have a team approach to managing polycythemia vera. This includes medical treatment, taking care of yourself, and getting support. In the end, dealing with polycythemia vera is a journey that needs commitment, strength, and the right help.
FAQ
What is polycythemia vera?
Polycythemia vera is a rare blood disorder. It causes the bone marrow to make too many red and white blood cells and platelets.
What are the symptoms of polycythemia vera?
Symptoms include headaches, dizziness, and itching. Fatigue, shortness of breath, and visual problems are also common. Skin redness can occur too.
What causes polycythemia vera?
A mutation in the JAK2 gene is the main cause. Genetic and environmental factors can also play a part.
How is polycythemia vera diagnosed?
Blood tests check for high red blood cell counts. A bone marrow biopsy and genetic testing confirm the JAK2 mutation.
What are the risks associated with untreated polycythemia vera?
Without treatment, it can lead to serious problems. These include blood clots, heart disease, and cancer.
How is polycythemia vera treated?
Treatment includes regular blood draws and medications. Lifestyle changes help manage symptoms and prevent complications.
Can polycythemia vera be cured?
There’s no cure, but effective treatment can control symptoms. It also reduces the risk of serious complications.
What lifestyle changes can help manage polycythemia vera?
Stay hydrated and avoid extreme temperatures. Manage stress and make healthy diet choices. Regular exercise is also beneficial.
How often should I have follow-up care for polycythemia vera?
Regular check-ups are key to monitoring the condition. The frequency depends on individual needs.
Are there any emergency symptoms that require immediate medical attention?
Yes, seek help for severe chest pain, trouble breathing, or sudden numbness or weakness.
Can polycythemia vera increase the risk of other health problems?
Yes, it can lead to heart disease and blood clots if not managed well.
Is polycythemia vera considered a cancer?
It’s a type of blood cancer called a myeloproliferative neoplasm. But it’s different from other cancers.
References
- Snow, C. F. (1999). Laboratory diagnosis of vitamin B12 and folate deficiency: A guide for the primary care physician. Archives of Internal Medicine, 159(12), 1289“1298.https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/485067
- NHS. (2024). Vitamin B12 or folate deficiency anaemia. NHS. https://www.nhs.uk/conditions/vitamin-b12-or-folate-deficiency-anaemia/