
Cervical cancer is a big health problem worldwide. In 2022, it led to 660,000 new cases and 350,000 deaths, says the World Health Organization. The speed at which cervical cancer spreads depends on the type of tumor, its stage, and personal risk factors. It usually starts as a precancerous lesion and turns into invasive cancer over years.
Knowing these factors is key to understanding cervical cancer’s treatment and outlook. We’ll look at how tumor type, stage, and individual risk factors affect its spread. This helps us see why catching it early is so important.
Key Takeaways
- Cervical cancer progression varies based on tumor type, stage, and individual risk factors.
- The disease typically advances from precancerous lesions to invasive cancer over several years.
- Understanding the factors that influence cervical cancer spread is critical for determining prognosis and treatment.
- Early detection is vital for effective prevention and treatment of cervical cancer.
- Cervical cancer caused 660,000 new cases and about 350,000 deaths in 2022, according to the World Health Organization.
Understanding Cervical Cancer: The Basics
Knowing the basics of cervical cancer is key for early detection and treatment. Cervical cancer happens in the cervix, which is the lower part of the uterus in women.
What Is Cervical Cancer?
Cervical cancer starts when abnormal cells in the cervix grow too much. This can happen because of certain human papillomavirus (HPV) infections. The World Health Organization says it’s the fourth most common cancer in women worldwide.
Common Types of Cervical Cancer
Most cervical cancers are squamous cell carcinoma or adenocarcinoma. Squamous cell carcinoma makes up 70-80% of cases. It starts in the squamous cells on the cervix’s surface. Adenocarcinoma comes from glandular cells that make mucus.
There are also adenosquamous carcinoma and small cell carcinoma, though they’re less common. Knowing these types helps doctors choose the right treatment.
Global and U.S. Epidemiology
Cervical cancer is a big health problem worldwide. In the U.S., the SEER program says there are 7.7 new cases per 100,000 women each year. It’s a major cause of death for women, mostly in poor countries where screening is rare.
Studying cervical cancer’s spread and causes helps us understand its impact. By looking at global and U.S. data, we can find ways to prevent and treat it better.
The Natural History of Cervical Cancer Development
It’s important to know how cervical cancer develops. This disease starts with small changes in cells and can become serious. Cervical cancer happens when normal cells turn into cancer cells over time.
From Normal Cells to Precancerous Lesions
Cervical cancer often starts with an HPV infection. HPV is a common virus spread through sex. Most people clear this virus, but some types can cause cancer.
HPV can change cervical cells, leading to precancerous lesions. These can be treated if caught early. But, these changes often don’t show symptoms, making regular check-ups key.
The Role of HPV in Cervical Cancer
HPV is the main cause of cervical cancer. Types like HPV 16 and 18 cause most cases. The virus changes host DNA, causing cells to grow out of control.
HPV’s link to cervical cancer is clear: “HPV DNA is found in more than 99% of cervical cancer cases worldwide.” This shows how important HPV is in causing the disease.
Typical Timeline of Progression
It can take years, even a decade, for cervical cancer to develop after HPV infection. This long time allows for early detection and treatment. Knowing this timeline helps in creating better screening and prevention plans.
Things like HPV type, other infections, and immune response affect how fast cancer develops. “The natural history of cervical cancer is characterized by a long preclinical phase, during which lesions can be detected and treated.” This shows the chance for early action.
Precancerous Lesions: Understanding the Terminology
It’s important to know the terms used for precancerous lesions. These are abnormal cell changes in the cervix. They could turn into cancer if not treated.
CIN Classification System (CIN1, CIN2, CIN3)
The CIN system is a way to sort precancerous lesions. It groups them into three levels based on how bad the cell changes are:
- CIN1: This is mild dysplasia, where the bad cells are in the lower part of the epithelium.
- CIN2: This is moderate dysplasia, where the bad cells go up to the middle part of the epithelium.
- CIN3: This is severe dysplasia or carcinoma in situ, where the bad cells cover more than two-thirds of the epithelium.
This system helps doctors figure out how serious the lesion is and what to do next.
The Bethesda System: LSIL and HSIL
The Bethesda System is another way to report cervical cytology results. It divides precancerous lesions into two main groups:
- LSIL (Low-grade Squamous Intraepithelial Lesion): This includes mild dysplasia or CIN1, showing a low risk of turning into cancer.
- HSIL (High-grade Squamous Intraepithelial Lesion): This includes moderate to severe dysplasia (CIN2 and CIN3), showing a higher risk of turning into cancer.
This system is used for Pap smear results. It helps standardize how we diagnose and manage precancerous lesions.
Relationship Between Classification Systems
The CIN system and the Bethesda System both describe precancerous lesions. But they have different focuses. The CIN system looks at how severe the lesion is. The Bethesda System looks at the risk of the lesion turning into cancer.
Knowing how these systems relate is key for doctors to make the best decisions for their patients.
How Fast Does HSIL Turn to Cancer?
Knowing how quickly HSIL can turn into cancer is key for managing cervical issues. HSIL, or High-grade Squamous Intraepithelial Lesions, is a precancerous condition. If not treated, it can lead to cervical cancer.
Average Progression Rates from Clinical Studies
Studies show that HSIL turning into cancer varies among people. Without treatment, many HSIL cases can become cervical cancer.
A Journal of Clinical Oncology study found that about 30% of women with untreated HSIL will get cervical cancer in 10 years. Another study said the time to progress can be 2 to 5 years, based on risk factors.
“The natural history of cervical cancer development from HSIL involves complex interactions between the human papillomavirus (HPV) and the host immune system.”
An Oncologist
HSIL Cancer Transformation Timeline
The time it takes for HSIL to turn into cancer is not the same for everyone. It depends on many factors, like HPV type, immune status, and lifestyle.
|
Time Frame |
Progression Risk |
|---|---|
|
2-5 years |
Moderate risk |
|
5-10 years |
Higher risk |
|
More than 10 years |
Significantly higher risk |
Risk Factors That Accelerate Progression
Several factors can make HSIL turn into cancer faster. These include:
- HPV Type: High-risk HPV types (like HPV 16, 18) increase the risk a lot.
- Immune Status: People with weak immune systems, like those with HIV/AIDS, are at higher risk.
- Lifestyle Factors: Smoking and long-term use of hormonal contraceptives raise the risk of cervical cancer.
Regression Possibilities
Even though the risk of progression is a concern, some HSIL cases can get better. This is true with the right treatment and lifestyle changes. Studies show that up to 30% of cases can regress.
Understanding these dynamics is key for managing HSIL well and preventing cancer.
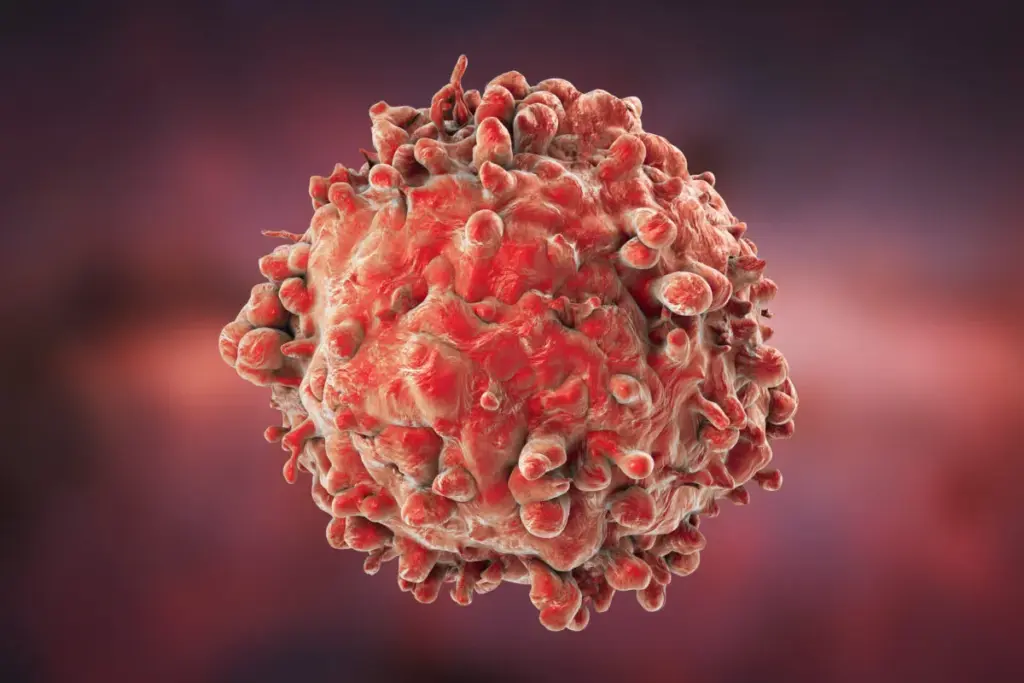
CIN1 to Cancer: Progression Timeline<SEP-1206_image_3>
Knowing how CIN1 turns into cancer is key to managing it well. CIN1, or cervical intraepithelial neoplasia grade 1, is a mild lesion. But, it’s important to know how it can grow worse.
Natural History of Low-Grade Lesions
Low-grade lesions like CIN1 are early signs of cervical neoplasia. Many CIN1 cases can go away on their own. But, some may stay or get worse.
How likely CIN1 is to get worse depends on several things. These include the type of HPV and how well the immune system works.
Can CIN1 Progress to Cancer in 6 Months?
CIN1 usually turns into cancer over years, not months. While it’s possible for CIN1 to turn into cancer, it takes longer than 6 months. Studies show it can take from 3 to 10 years or more, based on several factors.
CIN1 is a sign of higher risk for cervical cancer. But, turning into cancer is a long process. It’s influenced by HPV type, immune status, and lifestyle.
Monitoring Recommendations for CIN1
Women with CIN1 should get regular check-ups. This is to catch any signs of worsening or cancer early. Guidelines suggest follow-up tests every 12 months.
It’s also vital for those with CIN1 to know their risk factors. Talk to your doctor about your situation. This includes the role of HPV vaccine, smoking, and other lifestyle factors.
CIN3 to Invasive Cancer: Critical Transition
The move from CIN3 to invasive cancer is a key step in cervical cancer’s growth. CIN3, or cervical intraepithelial neoplasia grade 3, is a serious lesion. It has a big chance of turning into invasive cancer if not treated.
Knowing how fast high-grade lesions like CIN3 can turn into invasive cancer is key. Doctors need this info to care for their patients well. Studies show that CIN3 has a higher risk of turning into invasive cancer than lower-grade lesions.
Progression Rates for High-Grade Lesions
Studies say that CIN3 can turn into invasive cancer in 30% to more cases if not treated fast. How fast it happens can vary a lot. This depends on things like the immune system, HPV type, and other factors.
Key factors influencing progression include:
- The presence of high-risk HPV types
- The patient’s immune status
- Other lifestyle and genetic factors
CIN3 to Cancer in 6 Months: Evidence and Possibilities
While CIN3 usually turns into invasive cancer over years, some cases can happen in just 6 months. These fast cases show why watching closely and acting fast is so important.
Evidence suggests that rapid progression is often associated with:
- High-risk HPV infection
- Immunosuppression
- Other underlying health conditions
Why CIN3 Requires Immediate Attention
CIN3 needs quick action because it can easily turn into invasive cancer. Early treatment can stop this, which is why regular check-ups are so important.
Immediate steps for managing CIN3 include:
- Colposcopy and biopsy to confirm the diagnosis
- Treatment options such as LEEP or cryotherapy
- Close follow-up to monitor for recurrence or progression
By knowing the risks of CIN3 and acting early, we can lower the chance of invasive cervical cancer. This helps improve health outcomes for patients.
How Long Does It Take for HPV to Cause Abnormal Cells?
Knowing how long it takes for HPV to cause abnormal cells is key to preventing cervical cancer. HPV, or Human Papillomavirus, is a common virus that can lead to cervical cancer. But, how fast it turns into abnormal cells varies a lot from person to person.
HPV Infection to LSIL Timeline
The time it takes for HPV to cause Low-grade Squamous Intraepithelial Lesions (LSIL) can differ. Research shows LSIL can appear in a few months to a couple of years after getting HPV. But, this time can change based on the HPV type and how well the body fights it off.
Key factors influencing this timeline include:
- The specific type of HPV (high-risk vs. low-risk)
- The individual’s immune response to the virus
- Lifestyle factors that may impact immune function
Factors Affecting HPV Persistence
Not all HPV infections stick around, and many things can affect this. High-risk HPV types are more likely to stay and cause problems. People with weaker immune systems are also more likely to have persistent HPV infection.
High-Risk vs. Low-Risk HPV Types
HPV types are split into high-risk and low-risk based on their link to cervical cancer. High-risk types, like HPV 16 and 18, cause most cervical cancer cases. Low-risk types are more often linked to genital warts. Knowing the HPV type is important for understanding the risk of abnormal cells and cervical cancer.
We suggest regular check-ups and care to watch how HPV infection progresses. This helps catch any abnormal cell changes early.
How Fast Does Cervical Dysplasia Progress?
Understanding how cervical dysplasia progresses is key to managing it well. Cervical dysplasia, or CIN, means abnormal cells on the cervix that could turn into cancer if not treated.
It’s divided into mild (CIN1), moderate (CIN2), and severe (CIN3) based on cell changes. How fast these cells turn into cancer varies a lot from person to person.
Mild Dysplasia Progression Rates
Mild dysplasia, or CIN1, is often a short-term HPV infection. Many CIN1 lesions go away on their own. But, some can get worse.
Going from CIN1 to CIN2 or CIN3 takes years. It’s important to keep an eye on it to catch any changes early.
Moderate Dysplasia Progression Rates
Moderate dysplasia, or CIN2, has a higher chance of turning into severe dysplasia or cancer. This risk is higher if it’s not treated.
Women with CIN2 need to be watched closely. The risk of it turning into CIN3 or cancer is high. Treatment choices depend on many factors.
Severe Dysplasia Progression Rates
Severe dysplasia, or CIN3, is a serious condition with a high risk of turning into cancer. It can happen faster than in CIN1 or CIN2.
Quick treatment is usually needed for CIN3 to stop cancer from developing. The treatment choice depends on several factors.
Individual Variation in Progression Speed
The speed at which cervical dysplasia progresses can differ a lot between people. This depends on the type of HPV, the immune system, and lifestyle factors like smoking.
Regular check-ups are vital to catch any changes early. This allows for timely action if needed.
Cervical Cancer Growth Rate After Invasion
Knowing how fast cervical cancer grows after it invades nearby tissues is key. This helps doctors choose the best treatment. If not treated, cervical cancer can spread quickly, making early action vital.
Early-Stage Growth Patterns
In the early stages, cervical cancer grows slowly and often without symptoms. Regular screening is essential to catch it early when it’s easier to treat.
Research shows that cervical cancer grows at different rates in different people. Things like the type of HPV, the immune system, and lifestyle habits like smoking can affect how fast it grows.
Advanced-Stage Spread Dynamics
When cervical cancer gets to advanced stages, it grows faster and can spread to other areas. Knowing how it spreads is important for treatment planning.
The cancer can move to lymph nodes, bones, and other places, making treatment harder. Early detection and treatment are critical to stop this spread.
|
Stage |
Growth Characteristics |
Typical Symptoms |
|---|---|---|
|
Early-Stage |
Local growth, minimal symptoms |
Abnormal bleeding, pelvic pain |
|
Advanced-Stage |
Rapid growth, metastasis |
Severe pain, weight loss, urinary/bowel obstruction |
Cellular and Molecular Factors Affecting Growth Rate
Many factors affect how fast cervical cancer grows. High-risk HPV types, genetic changes, and changes in cell pathways can make it more aggressive.
Scientists are studying these factors to find new treatments. Understanding these mechanisms is essential for better treatment results.
Stages of Cervical Cancer and Spread Patterns
Knowing how cervical cancer grows is key to treating it well. It goes through different stages, each showing how far the disease has spread. We’ll look at these stages and what they mean for patient care.
Stage 1 Cervical Cancer: Local Disease
In Stage 1, the cancer is only in the cervix. It hasn’t spread to other tissues or organs yet. This stage is split into parts based on the tumor’s size and how deep it is. Catching it early can greatly improve treatment results.
Stage 2 Cervical Cancer: Regional Spread
At Stage 2, the cancer has moved beyond the cervix. It’s in the upper vagina or the area around the cervix. But it hasn’t reached the pelvic wall or other distant organs. Treatment at this stage might include surgery, radiation, or chemotherapy.
Stages 3 and 4: Advanced Disease
Stages 3 and 4 show the cancer has spread more. Stage 3 is in the lower vagina or the pelvic wall. Stage 4 means it’s in distant organs or the bladder/rectum. At these stages, treatment focuses on easing symptoms and improving life quality.
The spread patterns of cervical cancer are very important. They help doctors figure out the stage and the best treatment. This way, care plans can be made just for each patient.
By understanding the stages of cervical cancer, patients and doctors can work together. This can lead to better outcomes and a better quality of life.
Recent Trends in Cervical Cancer Progression
Recent studies have shown a worrying trend in cervical cancer. The way it develops and spreads is changing. This is important for both healthcare providers and patients to know.
Increasing Rates of Advanced-Stage Disease
There’s been a rise in advanced-stage cervical cancer cases. This is a big concern because it’s harder to treat and has a worse outlook. We must find out why this is happening to improve early detection and treatment.
The increase in advanced-stage disease might be due to several reasons. These include changes in screening, HPV vaccination rates, and lifestyle. We need to look into these areas to find ways to improve.
Distant-Stage Squamous Cell Carcinoma Trends
Squamous cell carcinoma is the most common cervical cancer type. Recent data show a worrying trend in distant-stage squamous cell carcinoma. This aggressive cancer needs quick treatment.
Understanding distant-stage squamous cell carcinoma trends helps us target high-risk groups. We should work on better screening and diagnosis to catch it early.
Factors Contributing to Changing Patterns
Many factors are behind the changing cervical cancer patterns. These include demographic changes, shifts in HPV prevalence, and differences in healthcare access and quality. We need to study these closely to grasp their impact.
- Demographic changes, like an aging population, can affect cancer rates.
- Changes in HPV prevalence due to vaccines may shape cervical cancer trends.
- Differences in healthcare access and quality can influence early detection and treatment success.
By understanding these factors, we can create targeted strategies. This will help address the changing cervical cancer trends and improve patient outcomes.
Factors That Accelerate Cervical Cancer Spread
It’s important to know what makes cervical cancer spread faster. This knowledge helps doctors find better ways to treat it. Cervical cancer grows in a complex way, influenced by many things.
Host Factors: Age, Immune Status, Genetics
Host factors greatly affect how fast cervical cancer spreads. Age is key, as older people often have weaker immune systems. This can make cancer grow faster. Immune status is also important; people with weak immune systems, like those with HIV/AIDS, are more at risk. Genetics can also play a role in how fast cancer grows.
Viral Factors: HPV Type and Viral Load
The type of Human Papillomavirus (HPV) and its load are big factors. Certain high-risk HPV types can lead to aggressive cancer. A high viral load can overwhelm the immune system, speeding up the disease.
Lifestyle Factors: Smoking, Contraceptive Use
Lifestyle choices can also affect cervical cancer spread. Smoking is a big risk factor that can make cancer worse. Some contraceptives may also increase cancer risk, speeding up its spread.
Impact of Delayed Diagnosis
Delayed diagnosis can make cervical cancer spread faster. Early detection is key to stopping cancer from getting worse. If cancer is not caught early, it can become harder to treat and may have a worse outcome.
Cervical Cancer Survival Rates by Stage and Spread
Knowing about cervical cancer survival rates is key for patients and doctors. It helps in choosing the right treatment. Survival rates change based on the disease’s stage and spread.
Early-Stage Survival Statistics
Early detection of cervical cancer leads to better survival chances. The American Cancer Society reports a 5-year survival rate of about 92% for early-stage cervical cancer.
- The 5-year survival rate for stage I cervical cancer is around 92%.
- For stage IA, the survival rate is even higher, typically above 95%.
Advanced-Stage Survival Statistics
Advanced cervical cancer has lower survival rates. Stage III has a 5-year survival rate of about 57%. Stage IV’s rate drops to around 17%.
Factors Affecting Prognosis
Several factors can change a cervical cancer patient’s prognosis. These include:
- Age: Older patients tend to have a poorer prognosis.
- Overall health: Patients with underlying health conditions may have a poorer prognosis.
- Tumor characteristics: The size, grade, and histological type of the tumor can impact prognosis.
Recent Improvements in Survival Outcomes
Recent years have seen better survival rates for cervical cancer. This is thanks to new treatments and early detection methods. Regular screening and early action are key.
We are committed to top-notch healthcare for international patients. Our team works hard to give the best care for cervical cancer patients.
Preventing Rapid Progression: Screening Guidelines
Regular cervical cancer screening is key to stopping the disease from getting worse. It helps find precancerous lesions or early cancer. This can greatly improve treatment success and survival chances.
Pap Smear Recommendations
The Pap smear, or Pap test, has been a mainstay in cervical cancer screening for years. The American Cancer Society advises starting Pap smear tests at age 21. Women aged 21 to 29 should get a Pap smear every 3 years.
Women aged 30 to 65 should get co-testing with Pap smear and HPV testing every 5 years. Or, they can get a Pap smear alone every 3 years.
Following these guidelines is vital for catching precancerous lesions and early cancer on time.
HPV Testing Guidelines
HPV testing is now a big part of cervical cancer screening, mainly for women over 30. The American Cancer Society suggests HPV testing with Pap smear every 5 years for women 30 to 65. HPV testing spots high-risk HPV types that can lead to cervical cancer.
Women with abnormal Pap smear results or HPV infection might need more frequent screening.
Colposcopy and Biopsy Timing
A colposcopy examines the cervix, vagina, and vulva for disease signs. If a Pap smear or HPV test shows something abnormal, a colposcopy might be done. During this, a biopsy is taken if any suspicious lesions are found.
The timing of colposcopy and biopsy varies based on the abnormality’s severity. Women with high-grade lesions or persistent low-grade lesions might need a colposcopy and biopsy.
New Technologies in Early Detection
New technologies are coming to make cervical cancer screening better. These include:
- HPV DNA testing with genotyping
- Liquid-based Pap cytology
- Automated Pap smear analysis
- Artificial intelligence-assisted colposcopy
These new tools could make cervical cancer screening more accurate and efficient.
|
Screening Method |
Recommended Frequency |
Age Group |
|---|---|---|
|
Pap Smear |
Every 3 years |
21-29 years |
|
Pap Smear + HPV Testing |
Every 5 years |
30-65 years |
|
Pap Smear |
Every 3 years |
30-65 years (alternative) |
By sticking to these screening guidelines and using the latest technologies, we can lower cervical cancer’s rapid progression risk. This improves treatment success and survival rates.
HPV Vaccination: Preventing the Initial Trigger
HPV vaccination is key in cutting down cervical cancer cases. It stops HPV infection, which is a major cause of cervical cancer. This makes it a vital tool in preventing cervical cancer.
Vaccination Timing and Effectiveness
When you get the HPV vaccine matters a lot. It works best if you get it before you start having sex. The Centers for Disease Control and Prevention (CDC) suggests getting it at ages 11 to 12. But, it can start as early as 9.
For those who missed out, the CDC says get vaccinated up to age 26. This is called catch-up vaccination.
Effectiveness of HPV Vaccination: Research shows HPV vaccines are very effective. A study in the Journal of the National Cancer Institute found a 90% drop in high-grade cervical lesions. This shows how well the vaccine works.
Population-Level Impact on Progression Rates
HPV vaccination can greatly lower cervical cancer rates. By stopping HPV infections, we can stop more people from getting cervical cancer.
“The introduction of HPV vaccination has the power to almost wipe out cervical cancer in the future. This is if we get enough people vaccinated.” –
A study in the U.S. found a big drop in high-grade cervical lesions among the vaccinated. This shows the vaccine’s impact on cervical cancer.
|
Vaccination Coverage |
Reduction in High-Grade Cervical Lesions |
|---|---|
|
Low Coverage ( |
Minimal Reduction |
|
Moderate Coverage (30-60%) |
Significant Reduction |
|
High Coverage (>80%) |
Substantial Reduction |
Current Recommendations
Experts say pre-teens should get the HPV vaccine. Those who missed it should catch up by age 26. The CDC backs this up.
As we get more people vaccinated, cervical cancer will likely go down a lot. This is a big step towards a healthier future.
Treatment Options Based on Progression Stage
The treatment for cervical cancer depends on its stage. Knowing the stage is key to picking the right treatment. We’ll look at the different treatments for each stage of the disease.
Management of Precancerous Lesions
Precancerous lesions are abnormal cell growths on the cervix. They can turn into cancer if not treated. Cryotherapy and LEEP (Loop Electrosurgical Excision Procedure) are common treatments for these lesions.
Treatment for Early-Stage Cancer
Early cervical cancer can be treated with surgery or radiation. Surgical options include hysterectomy or conization, depending on fertility wishes. Radiation therapy may be used alone or with chemotherapy.
Approaches for Advanced Disease
Advanced cervical cancer needs aggressive treatment. This often includes chemotherapy, radiation, and targeted therapy. The aim is to control the disease and improve life quality.
Impact of Treatment Timing on Outcomes
When treatment starts is very important for cervical cancer patients. Early treatment can stop the disease from getting worse. Regular screening and quick treatment are key to better outcomes.
In conclusion, cervical cancer treatment varies by stage. Understanding these treatments helps patients make informed choices about their care.
Conclusion: Key Takeaways About Cervical Cancer Progression
Cervical cancer can be stopped or slowed down with early detection and treatment. We’ve looked at the different stages of cervical cancer. This includes precancerous lesions and invasive cancer. We also talked about how fast HSIL turns to cancer.
The time it takes for HSIL to turn into cancer varies. But studies show that high-grade lesions can turn into cancer in a few years if not treated. This shows why we need to act quickly.
Prevention and treatment are key to lowering cervical cancer risk. We stress the importance of regular screenings, HPV vaccines, and treating precancerous lesions early. This helps prevent invasive cancer.
By knowing these key points about cervical cancer progression, we can all help fight this disease. Together, we can lower its incidence and improve treatment results for those affected.
FAQ
What is cervical cancer and how does it develop?
Cervical cancer is a type of cancer that happens in the cervix. It usually starts from abnormal cells caused by the human papillomavirus (HPV). It takes years for these cells to turn into cancer, going through different stages of abnormal growth.
How quickly can cervical cancer spread?
How fast cervical cancer spreads depends on several things. These include the cancer’s stage, the type of tumor, and personal risk factors. Early cancer grows slowly, but advanced cancer can spread quickly.
Can CIN1 progress to cancer in 6 months?
It’s very rare for CIN1 (mild dysplasia) to turn into cancer in 6 months. Most of the time, CIN1 either goes away or stays the same. It usually takes years for it to turn into cancer.
How long does it take for HPV to cause abnormal cells?
How long it takes for HPV to cause abnormal cells varies a lot. Sometimes, it can cause mild lesions in a few months or years. Other times, it might not cause any problems at all.
What is the difference between LSIL and HSIL?
LSIL (Low-grade Squamous Intraepithelial Lesion) and HSIL (High-grade Squamous Intraepithelial Lesion) are levels of abnormal cell changes in the cervix. LSIL is mild, while HSIL is more serious and has a higher risk of turning into cancer.
How fast does HSIL turn to cancer?
How fast HSIL turns into cancer varies. Studies show that many HSIL cases can turn into cancer if not treated. It can take anywhere from a few years to over a decade for this to happen.
What are the risk factors that accelerate cervical cancer progression?
Several things can make cervical cancer progress faster. These include persistent HPV infection, smoking, being immunosuppressed, and certain lifestyle choices. Early detection and treatment can greatly improve outcomes.
What are the stages of cervical cancer, and how do they affect spread patterns?
Cervical cancer is staged from I to IV. Stage I is when it’s just in the cervix, and stage IV is when it’s spread to other parts of the body. The stage at diagnosis affects treatment and how well you might do.
How effective is HPV vaccination in preventing cervical cancer?
HPV vaccination is very effective in preventing cervical cancer. It protects against the most common types of HPV that cause cancer. It’s recommended before becoming sexually active and has been shown to lower cervical cancer and precancerous lesion rates.
What are the treatment options for cervical cancer based on progression stage?
Treatment for cervical cancer depends on its stage. Early cancer might be treated with surgery or localized therapies. Advanced cancer often needs a mix of chemotherapy, radiation, and other treatments.
How can cervical cancer survival rates be improved?
Survival rates for cervical cancer can be bettered by early detection and treatment. Prevention through HPV vaccination is also key. Understanding and addressing factors that affect prognosis is important too.
References:
Frontiers in Medicine. Cervical cancer research article. https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1579446/full
World Health Organization (WHO). Cervical cancer fact sheet. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
National Cancer Institute, Surveillance, Epidemiology, and End Results Program (SEER). Cervical cancer statistics. https://seer.cancer.gov/statfacts/html/cervix.html
American Cancer Society. Key statistics for cervical cancer. https://www.cancer.org/cancer/cervical-cancer/about/key-statistics.html
PubMed Central (PMC). Cervical cancer research article. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10492095/
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/cervical-cancer










