Understand the science. Discover why the bone marrow is the key to curing leukemia and why a transplant is the ultimate medical goal.
Leukemia is a blood cancer that affects thousands globally. For many, a bone marrow transplant is a lifesaving option. Getting this diagnosis can be scary, and the thought of a transplant can be overwhelming.
But, this treatment can replace damaged cells with healthy ones. This can improve chances of remission and better life quality. Leukemia is a big reason for bone marrow transplants worldwide, showing its importance in treatment.
Key Takeaways
- Leukemia patients often need a bone marrow transplant to replace unhealthy cells.
- This procedure can be the best chance for a cure or long-term remission.
- It involves swapping damaged bone marrow with healthy cells.
- Leukemia is a major reason for bone marrow transplants globally.
- Modern medicine keeps improving treatments for leukemia and blood cancers.
Understanding Leukemia and Its Impact on the Body

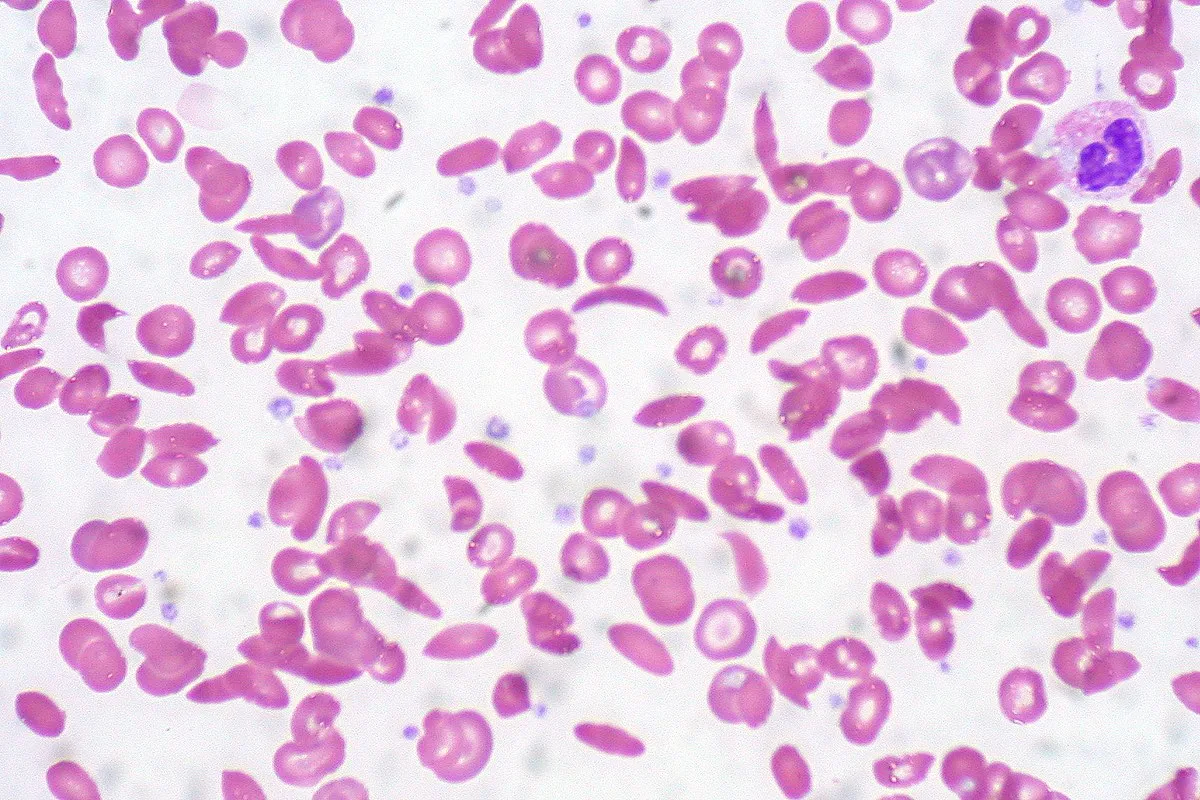
It’s important to understand leukemia to see how it affects the body. Leukemia is a cancer that messes with blood and bone marrow. It happens when white blood cells grow too much.
What is Leukemia?
Leukemia is a serious disease that messes with blood cell making in the bone marrow. This can cause anemia, infections, and bleeding problems. If not treated, it can get worse fast.
How Leukemia Affects Blood Cell Production
Leukemia stops the bone marrow from making healthy blood cells. The bad white blood cells take over, leaving less room for good cells. This can cause tiredness, more infections, and bleeding issues.
Types of Leukemia and Their Severity
There are different kinds of leukemia, each with its own severity. The main types are:
- Acute Lymphoblastic Leukemia (ALL): This type gets worse fast and needs quick treatment.
- Chronic Lymphocytic Leukemia (CLL): This type gets worse slowly and might not need immediate treatment.
- Acute Myeloid Leukemia (AML): This type gets worse fast and affects myeloid cells.
- Chronic Myeloid Leukemia (CML): This type gets worse slowly and affects myeloid cells.
|
Type of Leukemia |
Speed of Progression |
Common Age Group Affected |
|---|---|---|
|
Acute Lymphoblastic Leukemia (ALL) |
Fast |
Children and young adults |
|
Chronic Lymphocytic Leukemia (CLL) |
Slow |
Adults over 60 |
|
Acute Myeloid Leukemia (AML) |
Fast |
Adults, increasing with age |
|
Chronic Myeloid Leukemia (CML) |
Slow |
Adults, peak in 50s and 60s |
Knowing about leukemia helps us see why treatments like bone marrow transplants are needed. The type and how severe it is decide the best treatment.
The Critical Functions of Bone Marrow in Human Health
Bone marrow is a spongy tissue inside bones. It’s key for making blood cells and boosting the immune system. It’s a vital part of our body’s system for making blood cells.
What is Bone Marrow and Where is it Located?
Bone marrow is inside the bones, mainly in the hips, thighbones, and spine. It’s a complex tissue filled with hematopoietic stem cells. These cells turn into different blood cell types. The bone marrow’s rich blood vessel environment helps blood cells grow.
- Bone marrow is found in the bones of the pelvis, vertebrae, and the ends of long bones.
- It produces about 500 billion blood cells every day.
- The bone marrow environment is key for blood cell development and maturation.
How Bone Marrow Produces Blood Cells
The process of making blood cells, called hematopoiesis, happens in the bone marrow. Hematopoietic stem cells turn into different blood cell types. This process is controlled by growth factors and cytokines.
- Hematopoietic stem cells become myeloid and lymphoid progenitor cells.
- Myeloid progenitors make red blood cells, platelets, and some white blood cells.
- Lymphoid progenitors turn into lymphocytes, a type of white blood cell important for fighting infections.
The Immune System’s Relationship with Bone Marrow
The bone marrow is vital for the immune system. It produces immune cells like lymphocytes and other white blood cells. These cells help fight infections and diseases. The bone marrow also stores immune cells, releasing them when needed.
In summary, bone marrow is essential for human health. It supports blood cell production and immune function. Knowing its importance helps us understand the role of bone marrow transplants in treating blood disorders.
How Leukemia Damages Bone Marrow Function
It’s important to know how leukemia harms bone marrow. This is why treatments like bone marrow transplants are needed. Leukemia cells get into the bone marrow and stop it from making healthy blood cells.
“The bone marrow is the spongy tissue inside some of your bones, such as your hips and thighbones, which produces blood cells,” explains the importance of bone marrow in our body. When leukemia cells invade this area, they compromise its function, leading to various health complications.
The Mechanism of Bone Marrow Infiltration
Leukemia cells get into the bone marrow through a complex process. They avoid normal cell rules and take over. This crowds out healthy cells needed for blood production.
This process is like an invasion. The leukemia cells use up the bone marrow’s space and resources. This affects the production of red blood cells, white blood cells, and platelets, and weakens the immune system.
Consequences of Compromised Bone Marrow
When bone marrow is damaged by leukemia, the effects are serious. Patients might get anemia, infections, and bleeding disorders. These problems can make life hard.
The impact on a patient’s quality of life can be significant, with increased fatigue, heightened risk of infections, and other complications that require careful management. Often, the only way to fix this is with a bone marrow transplant, or BMT.
In conclusion, leukemia’s harm to bone marrow is a key part of the disease. It needs treatments like bone marrow transplantation to fix blood cell production and help patients.
When Bone Marrow Transplantation Becomes Necessary
Bone marrow transplantation is needed when leukemia is severe or doesn’t respond to treatment. This is a more aggressive option. It’s considered when other treatments fail or the leukemia is very aggressive.
Medical Indicators for Transplantation
Several signs show the need for a bone marrow transplant. These include:
- Aggressive or high-risk leukemia
- Failure to achieve remission after initial treatment
- Relapse after previous treatments
- Specific genetic markers indicating a high risk of treatment failure
Healthcare providers may suggest a bone marrow transplant when these signs are present.
When Other Treatments Fail
If leukemia doesn’t respond to usual treatments like chemotherapy, a bone marrow transplant is an option. This is true for those with aggressive leukemia needing stronger treatment.
Replacing Unhealthy Bone Marrow After Intensive Treatments
Intensive chemotherapy or radiation can severely damage bone marrow. In these cases, a transplant is needed. It replaces the damaged marrow with healthy cells, either from the patient (autologous transplant) or a donor (allogeneic transplant).
|
Transplant Type |
Source of Cells |
Typical Use Case |
|---|---|---|
|
Autologous |
Patient’s own cells |
When patient’s bone marrow is healthy enough to be harvested, treated, and reinfused. |
|
Allogeneic |
Donor cells |
When patient’s bone marrow is diseased or damaged beyond recovery. |
Knowing when a bone marrow transplant is needed helps patients and families make better treatment choices.
Types of Bone Marrow Transplants for Leukemia Patients
Leukemia treatment has evolved to include several types of bone marrow transplants. Each type is tailored to the individual needs of patients. The choice of transplant type depends on the patient’s health, donor availability, and leukemia characteristics.
Autologous Transplants: Using the Patient’s Own Cells
Autologous bone marrow transplants use the patient’s own stem cells. This option is often chosen for patients in remission or not ideal for an allogeneic transplant.
- Advantages: Reduced risk of graft-versus-host disease (GVHD), as the patient’s own cells are used.
- Considerations: The risk of reintroducing cancerous cells if the patient’s marrow is not completely cleared of leukemia cells.
Allogeneic Transplants: Donor-Derived Cells
Allogeneic transplants use stem cells from a donor. This donor can be a related or unrelated individual, provided there is a suitable Human Leukocyte Antigen (HLA) match.
Experts note, “Allogeneic transplantation offers a graft-versus-leukemia effect. The donor’s immune cells help fight the patient’s leukemia.”
This effect is a significant advantage, potentially reducing the risk of leukemia relapse.
- Benefits: The graft-versus-leukemia effect can help reduce the risk of leukemia relapse.
- Challenges: The risk of GVHD, where the donor’s immune cells attack the patient’s tissues.
Haploidentical and Cord Blood Transplants
Haploidentical transplants involve using a partially HLA-matched donor, often a family member. Cord blood transplants utilize stem cells from umbilical cord blood. This offers an alternative when a traditional HLA-matched donor is not available.
- Haploidentical Transplants: Allow for a broader donor pool, including family members who are not fully HLA-matched.
- Cord Blood Transplants: Provide a readily available source of stem cells, with a lower risk of GVHD.
Each type of bone marrow transplant has its advantages and considerations. The choice of transplant depends on a thorough evaluation of the patient’s condition and available donor options.
The Bone Marrow Transplant Procedure Explained
For many leukemia patients, a bone marrow transplant is a key treatment option. It involves several stages. Knowing about the bone marrow transplant procedure can ease worries and prepare patients for what’s ahead. The process includes getting ready for the transplant, collecting stem cells, and the transplant itself. Each step is important for the treatment’s success.
Pre-Transplant Preparation and Conditioning
Pre-transplant preparation is a critical step. It gets the patient’s body ready for the transplant. This includes chemotherapy and sometimes radiation therapy. The goal is to remove the old, often sick, bone marrow for new stem cells. Conditioning regimens can be tough and have big side effects, but they’re key for the transplant’s success.
During this time, patients are watched closely for any problems. Supportive care helps manage side effects. This care may include medicines to prevent infections, blood transfusions, and nutritional support.
The Harvesting Process
The harvesting process collects stem cells. This can be from the patient themselves (autologous transplant) or a donor (allogeneic transplant). For autologous transplants, stem cells are collected after giving medications to release them into the bloodstream. For allogeneic transplants, stem cells come from a compatible donor, usually through a blood donation-like process.
The harvesting method aims to be safe and comfortable for both the donor and the recipient. The collected stem cells are then prepared for transplantation.
Transplantation and Initial Recovery
The transplant process is simple. The prepared stem cells are infused into the patient’s bloodstream through an intravenous line, like a blood transfusion. The stem cells then go to the bone marrow to make new blood cells.
Initial recovery is a key time. The patient is watched closely for signs of engraftment, infection, or graft-versus-host disease (GVHD) in allogeneic transplants. Supportive care continues, focusing on managing side effects and preventing complications.
As the new bone marrow starts working, patients see improvements in their blood counts and health. But, full recovery takes time. Ongoing care is needed to watch for any late transplant effects.
“The success of a bone marrow transplant depends not only on the procedure itself but also on the complete care given before, during, and after the transplant.”
Hematologist
Understanding the bone marrow transplant procedure helps patients better navigate their treatment. Knowing what to expect at each stage is important.
Finding a Compatible Bone Marrow Donor
Finding a bone marrow donor is key for a successful transplant. This includes HLA typing, checking family members, and searching donor registries.
HLA Typing and Matching Process
HLA typing is a genetic test that finds specific genes in an individual. These genes help the immune system fight off invaders. In bone marrow transplants, matching donors and recipients is vital to avoid complications.
The test looks at several genes, like HLA-A and HLA-DRB1. A close match between donor and recipient is important for a successful transplant.
Family Members as Possible Donors
Family members are often the first choice for donors. Siblings have a 25% chance of being a match. Parents and children are also likely to be partial matches.
When a family member is considered, they go through HLA typing. This includes medical and psychological checks to make sure they’re willing to donate.
Unrelated Donor Registries and Their Importance
When family donors aren’t available, donor registries are essential. These registries have volunteers who are willing to donate.
Donor registries are very important. They offer a wide range of donors, helping patients from different backgrounds find a match. The bigger and more diverse the registry, the better the chances of finding a donor.
|
Donor Type |
Match Probability |
Donation Process |
|---|---|---|
|
Sibling |
25% chance of being a full match |
Medical and psychological evaluation |
|
Unrelated Donor |
Varies based on registry diversity |
Registry search and HLA typing confirmation |
|
Parent/Child |
Typically a half-match |
Medical evaluation and HLA typing |
Understanding HLA typing, family donors, and donor registries shows how complex finding a donor is. This process is vital for successful transplants, giving hope to patients with blood disorders.
The Challenge of Donor Diversity and Ethnic Disparities
Finding a bone marrow donor is hard, even more so for people from different ethnic backgrounds. The chance of finding a match varies a lot between ethnic groups. Some groups have a much lower chance of finding a compatible donor.
Donor diversity is key for patients from all ethnic backgrounds to have a fair chance of finding a match. The state of unrelated donor registries is very important. It directly affects how many compatible donors are available for patients.
Varying Match Rates Across Ethnic Groups
Studies show that finding a suitable donor depends a lot on the patient’s ethnic background. People from well-represented ethnic groups have a better chance of finding a match. But those from underrepresented groups face bigger challenges.
Patients from ethnic minorities often struggle to find a compatible donor. A leading expert, says: “
The lack of diversity in donor registries is a pressing issue that affects the outcomes of bone marrow transplants for patients from diverse ethnic backgrounds.
“
Initiatives to Increase Donor Diversity
Several initiatives aim to increase diversity in donor registries. These include targeted recruitment campaigns and partnerships with community groups. The goal is to raise awareness about the importance of bone marrow donation.
There’s a positive trend in growing diverse donor registrations. This is key for improving match rates for patients from all ethnic backgrounds. We must keep these efforts going to ensure everyone has an equal chance to find a compatible donor.
By boosting donor diversity and improving representation in unrelated donor registries, we can make bone marrow transplantation fairer for all patients.
Global Statistics on Bone Marrow Transplants for Leukemia
Looking at global bone marrow transplant stats gives us insight into their success. We’ll dive into current trends, recent data, and how well these transplants work for leukemia patients.
Current Transplant Rates and Trends
The number of bone marrow transplants worldwide has gone up each year. This rise is mainly because more people have leukemia and because transplant tech has improved.
2023 Transplant Data: 47,000+ Procedures in Europe
In 2023, over 47,000 bone marrow transplants happened in Europe, studies show. This highlights the need for this treatment in fighting leukemia.
Success Rates and Survival Statistics
How well bone marrow transplants work depends on several things. These include the leukemia type, the patient’s age, and how well the donor’s marrow matches. Thanks to better tech and care, survival rates have gotten better over time.
|
Region |
Number of Transplants (2023) |
Success Rate (%) |
|---|---|---|
|
Europe |
47,000+ |
60-80 |
|
North America |
30,000+ |
55-75 |
|
Asia |
20,000+ |
50-70 |
There’s been a big jump in bone marrow transplants worldwide, with Europe leading the way in 2023. Success rates differ by region but are getting better. As tech keeps improving, we might see even better results for leukemia patients getting these transplants.
Potential Complications and Risks of Bone Marrow Transplantation
Bone marrow transplantation offers hope for leukemia patients. But, it’s important to know the risks and complications. This procedure replaces a patient’s diseased bone marrow with healthy marrow, from themselves or a donor.
Graft-Versus-Host Disease (GVHD)
Graft-versus-host disease is a big risk in allogeneic transplants. It happens when the donor’s immune cells attack the recipient’s body. GVHD can be acute or chronic, affecting the skin, liver, and gut.
Managing GVHD means using immunosuppressive drugs. These drugs help reduce the attack on the body. Proper HLA matching between donor and recipient also helps prevent GVHD.
Infection Risks During Recovery
Patients after bone marrow transplant are at high risk of infections. This is because the conditioning regimen weakens the immune system. Infections can be bacterial, viral, or fungal, happening early or months later.
Preventing and managing infections is key. This includes using antimicrobial drugs, watching for signs of infection, and treating them quickly. Patients are also taught how to avoid infections.
Other Possible Complications
Other issues with bone marrow transplant include organ damage and graft failure. The conditioning regimen can harm organs like the liver and lungs. Graft failure means the new marrow doesn’t work.
|
Complication |
Description |
Management |
|---|---|---|
|
Graft-Versus-Host Disease (GVHD) |
Donor immune cells attack recipient tissues |
Immunosuppressive medications |
|
Infections |
Bacterial, viral, or fungal infections due to immunosuppression |
Prophylactic antimicrobial therapy, monitoring, and prompt treatment |
|
Organ Damage |
Damage to organs like liver, lungs, and heart from conditioning regimen |
Supportive care, monitoring, and management of organ-specific complications |
Knowing about these complications helps manage risks in bone marrow transplant. Healthcare providers can then give the best care to patients facing this complex treatment.
The Recovery Journey After a Bone Marrow Transplant
After a bone marrow transplant, patients start a long recovery journey. This journey is not just about healing from the transplant. It’s also about rebuilding health and managing possible complications.
Short-term Recovery Expectations
In the short term, patients face many challenges. These challenges include the conditioning regimen and the risk of infections. The conditioning regimen can cause side effects like fatigue, nausea, and hair loss.
The period right after the transplant is critical. It’s when the risk of infections and graft-versus-host disease (GVHD) is highest. To manage these risks, patients stay in the hospital for weeks after the transplant.
While in the hospital, they receive supportive care. This includes blood transfusions, antibiotics, and medications to prevent or treat infections and GVHD. The healthcare team closely watches the patient’s condition. They adjust treatment as needed to help the patient recover smoothly.
|
Aspect of Care |
Description |
Importance |
|---|---|---|
|
Infection Prevention |
Use of antibiotics and other medications to prevent infections. |
High |
|
Blood Transfusions |
Transfusion of blood components to support blood cell counts. |
High |
|
GVHD Prophylaxis |
Medications to prevent graft-versus-host disease. |
High |
|
Nutritional Support |
Dietary advice and supplements to maintain nutrition. |
Medium |
Long-term Follow-up and Monitoring
Long-term follow-up is key to monitoring the new bone marrow’s health. It also helps address any late effects of the treatment. This includes regular check-ups with the healthcare team and monitoring for signs of GVHD.
Patients are also watched for signs of disease relapse and secondary malignancies. The frequency of follow-up visits decreases over time. But long-term monitoring is a critical part of post-transplant care.
Quality of Life Considerations
Maintaining and improving quality of life is important in the recovery journey. This involves managing physical health and addressing emotional and psychological impacts of the transplant.
Patients are encouraged to gradually return to normal activities, like work and social engagements. Support from family, friends, and support groups is vital in helping patients cope with recovery challenges.
Understanding the recovery journey after a bone marrow transplant helps patients and their caregivers navigate this complex process. This improves outcomes and quality of life.
Advancements in Bone Marrow Transplant Procedures
Recent years have seen big changes in bone marrow transplant procedures. These changes have made transplants safer and more effective for patients with leukemia.
Reduced-Intensity Conditioning Regimens
One big change is the use of reduced-intensity conditioning (RIC) regimens. RIC regimens help more patients get transplants. This includes older patients and those with health issues.
RIC uses lower doses of chemotherapy and/or radiation. This makes the transplant process safer and more comfortable for more people.
Improved GVHD Prevention and Treatment
Graft-versus-host disease (GVHD) is a big problem with bone marrow transplants. But, new ways to prevent and treat GVHD are helping patients. New immunosuppressive strategies and better matching of donors and recipients have cut down on GVHD.
New therapies are also being tested. They target specific parts of GVHD. These efforts are making transplants safer and more effective.
Emerging Technologies and Approaches
New technologies and approaches are coming into bone marrow transplantation. For example, haploidentical transplantation is becoming more common. It allows for more donors, including family members who aren’t a perfect match.
Another area seeing progress is the use of cord blood for transplants. Cord blood is a rich source of stem cells. It may also lower the risk of GVHD.
|
Advancement |
Description |
Benefit |
|---|---|---|
|
Reduced-Intensity Conditioning |
Lower doses of chemotherapy and/or radiation |
Increased eligibility for older patients and those with comorbidities |
|
Improved GVHD Prevention |
New immunosuppressive strategies and better donor-recipient matching |
Reduced incidence and severity of GVHD |
|
Haploidentical Transplantation |
Transplantation using partially HLA-matched donors |
Broader pool of possible donors |
|
Cord Blood Transplants |
Use of cord blood as a source of hematopoietic stem cells |
Potential reduction in GVHD risk |
These changes in bone marrow transplant procedures are changing how we treat leukemia. They offer better results and hope for patients. As research keeps moving forward, we can look forward to even more improvements in care for transplant patients.
Medical Centers of Excellence and International Standards
For patients needing bone marrow transplants, top medical centers offer hope. These places are key for complex treatments. They need skilled teams and the right setup.
Academic Care Paths
Academic care paths are vital for the best treatments. Medical centers of excellence follow these paths. They use the newest research and guidelines.
This way, healthcare teams can tailor treatments for each patient. It helps improve results and life quality.
These centers use a team effort. Specialists from different fields work together. They create treatment plans that fit each patient’s needs.
Ethical Considerations
Ethics are very important in transplant medicine. Respecting patient choices is a big part of it. Patients must be informed and involved in their care.
Top medical centers focus on ethics. They are open and honest with patients and families. They give full details about treatment options and risks.
Case Study: LIV Hospital’s Approach to Transplant Care
LIV Hospital is a top center for bone marrow transplants. They focus on academic care and ethics.
“At LIV Hospital, we believe that the key to successful bone marrow transplantation lies in a multidisciplinary approach, combining the latest medical research with a patient-centered care model,” said a representative from LIV Hospital.
LIV Hospital’s care includes a detailed check before transplant, a skilled team, and close follow-up. Their results meet or beat international standards.
Medical centers like LIV Hospital lead in bone marrow transplants. They focus on patient care, ethics, and research. These centers save lives and push medical science forward.
Conclusion: The Life-Saving Bone Marrow Transplants Offer a Life-Saving Option
Bone marrow transplants can save lives for those with leukemia. They offer a chance for a cure or long-term remission. The process involves making tough choices about the transplant type, finding the right donor, and dealing with possible complications.
The need for bone marrow transplants is growing. This is because more people are getting blood cancers and new transplant methods are being developed. In 2023, over 47,000 procedures were done in Europe, showing how much this treatment is needed.
Improvements in bone marrow transplants are making them more effective and available. Learning about leukemia treatment and bone marrow transplants helps us see the need for ongoing research. This research is key to making this treatment even better.
FAQ
What is a bone marrow transplant?
A bone marrow transplant replaces damaged bone marrow with healthy cells. These cells come from the patient or a donor.
Why is a bone marrow transplant necessary for leukemia patients?
Leukemia harms the bone marrow, stopping it from making blood cells. A transplant can replace the bad marrow with good cells. This helps the patient get better and live a better life.
What are the different types of bone marrow transplants?
There are many types of bone marrow transplants. These include using the patient’s own cells, cells from a donor, or stem cells from umbilical cord blood.
How is a compatible bone marrow donor found?
Donors are found by matching Human Leukocyte Antigen (HLA) types. Family members are often first choices because they are genetically similar. But, unrelated donors can also be found through registries.
What are the possible complications of a bone marrow transplant?
Complications can include graft-versus-host disease (GVHD) and infections. These issues can arise during the recovery phase.
What is graft-versus-host disease (GVHD)?
GVHD happens when the donor’s immune cells attack the recipient’s body. It can be acute or chronic and needs careful management.
How long does it take to recover from a bone marrow transplant?
Recovery has short-term and long-term phases. Patients need close monitoring and follow-up care. This helps manage complications and ensures the new bone marrow is healthy.
What advancements have been made in bone marrow transplantation?
New advancements include less intense conditioning regimens and better GVHD prevention. New technologies also make transplants safer and more effective.
What is the role of medical centers of excellence in bone marrow transplantation?
Medical centers of excellence provide top-notch care for bone marrow transplant patients. They follow international standards and use the latest research and guidelines.
How does leukemia affect bone marrow function?
Leukemia damages the bone marrow by filling it with cancer cells. This disrupts blood cell production, leading to anemia, infections, and bleeding disorders.
What are the benefits of autologous bone marrow transplants?
Autologous transplants use the patient’s own cells. This reduces the risk of GVHD and allows for quicker recovery.
What is the significance of donor diversity in bone marrow transplantation?
Donor diversity is key for patients from different ethnic backgrounds. It ensures they have a fair chance of finding a compatible donor.
What is hematopoietic stem cell transplantation?
Hematopoietic stem cell transplantation is another name for bone marrow transplantation. It involves transferring stem cells that produce blood cells.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6112322/