What is an hsc in the context of fertility? Discover the secrets of how these cells impact reproductive health and modern medical research.
Fertility tests can be complex. They involve many diagnostic tests to find possible issues. One important test is the HSG (Hysterosalpingography), often called HSC in fertility talks.
The HSG test is a special X-ray. It checks the shape of the uterus and if the fallopian tubes are open. Both are key for women trying to get pregnant. Knowing about HSG helps people understand the fertility check process and what might block their way to having a child.
Key Takeaways
- HSG stands for Hysterosalpingography, a diagnostic test used in fertility assessments.
- The test evaluates the uterine cavity’s shape and fallopian tube patency.
- Understanding HSG is key to spotting fertility problems.
- HSG is a main tool for checking female infertility causes.
- The test gives important info on reproductive health.
Clarifying HSC vs. HSG in Fertility Testing

The difference between HSC and HSG is often confusing in reproductive medicine.
Common Terminology Confusion in Reproductive Medicine
Reproductive medicine uses a lot of complex terms. This can confuse both patients and doctors. The mix-up between HSC and HSG is a big part of this problem.
HSG stands for Hysterosalpingogram, a key test. It checks if the fallopian tubes are open and the uterus is shaped right. Both are important for fertility.
HSC Medical Abbreviation in Different Contexts
HSC can mean different things depending on where you see it. For example, in bone marrow transplants, HSC means Hematopoietic Stem Cells. Knowing the context is key to understanding HSC.
To make things clear, here’s what you need to know about HSG:
- HSG is a diagnostic procedure that uses contrast and X-rays.
- It checks if the fallopian tubes are open and the uterus is shaped right.
- HSG is a key tool for checking fertility, spotting blockages or issues.
Knowing the difference between HSC and HSG helps people understand their fertility tests better. This way, they can make better choices about their reproductive health.
What is an HSC? Addressing the Terminology Question

It’s important to know the difference between HSC and HSG in fertility talks. Both are used in medicine, but they mean different things.
HSC Definition and Meaning in Various Fields
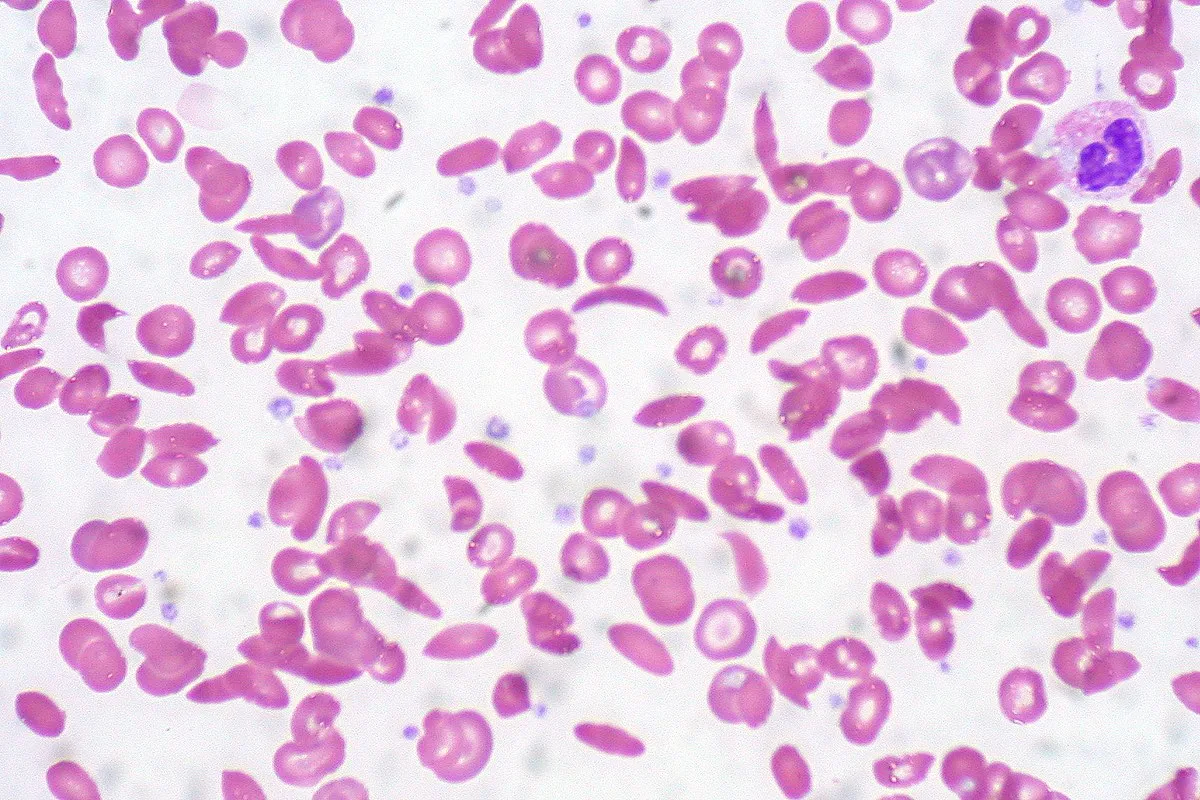
HSC stands for Hematopoietic Stem Cells. It’s mainly used in bone marrow transplants and regenerative medicine. Hematopoietic Stem Cells make blood cells and are key in treating blood disorders.
HSC can also mean other medical terms, but these are not as common in fertility talks. This shows how vital clear talk is in medical care.
Why HSG is the Correct Term in Fertility Assessment
In fertility tests, HSG is the right term. It stands for Hysterosalpingogram. This test checks the uterus and fallopian tubes for problems. It uses X-rays and a contrast agent.
HSG is key in finding out why someone might not be able to get pregnant. It shows if the tubes are blocked or if the uterus is shaped wrong. This helps doctors plan the best treatment.
Unlike HSC, Hysterosalpingogram (HSG) is all about checking the reproductive system. So, when we talk about fertility tests, HSG is the term we should use.
Hysterosalpingogram (HSG): The Essential Fertility Diagnostic Tool
HSG is a special X-ray test that looks at the uterus and fallopian tubes. It’s key in checking if a woman can get pregnant by showing how her reproductive system works.
Definition and Purpose of HSG Procedure
The HSG procedure uses a contrast agent and X-rays to see the uterus and fallopian tubes. Its main goal is to check if the fallopian tubes are open and find any problems in the uterus.
This test is done in a radiology department or fertility clinic. First, a speculum is put in the vagina to see the cervix. Then, a cannula goes through the cervix into the uterus. The contrast material is injected through it. X-ray pictures are taken as the contrast moves through, showing if the tubes are open.
|
Procedure Step |
Description |
|---|---|
|
1. Preparation |
The patient is positioned on an X-ray table, and a speculum is inserted into the vagina. |
|
2. Contrast Injection |
A cannula is inserted through the cervix, and contrast material is injected into the uterine cavity. |
|
3. Imaging |
X-ray images are taken as the contrast material flows through the uterus and fallopian tubes. |
Historical Development of Fallopian Tube Imaging
Imaging the fallopian tubes started in the early 20th century. Over time, methods have changed a lot. From using radium to today’s contrast agents and digital X-rays.
Historical milestones include the use of safer, water-soluble contrast agents and digital fluoroscopy. This has made imaging safer and clearer, with less radiation.
The growth of fallopian tube imaging has been key in improving fertility tests. Today, HSG is a main tool for checking if tubes are open and finding uterine issues. It helps doctors decide on the next steps for fertility care.
The Critical Role of Fallopian Tubes in Fertility
The fallopian tubes are key in the female reproductive system. They help the egg move from the ovary to the uterus. Their health is vital for successful fertilization.
Understanding Tubal Function in Conception
Tubal function is key for conception. It allows the egg to travel from the ovary to the uterus. The fallopian tubes have cilia that move the egg. Their muscular layer also helps move it.
The success of conception depends on the patency and functionality of the fallopian tubes. Any damage or blockage can greatly reduce fertility.
How Tubal Factors Affect Fertility Rates
Tubal factors are a big reason for female infertility. About 25-35% of cases are linked to fallopian tube issues. Damage or blockage can come from pelvic inflammatory disease, endometriosis, or surgeries.
Tubal problems have a big impact on fertility rates. Damaged or blocked tubes stop the egg from being fertilized or reaching the uterus. It’s important to understand and treat tubal issues to help with infertility.
Prevalence of Tubal Factors in Female Infertility
It’s key to know how common tubal factors are in female infertility. Tubal factors are any issues with the fallopian tubes. These tubes are vital for getting pregnant.
Research Statistics on Tubal-Related Infertility
Many studies show tubal factors play a big role in female infertility. About 25-35% of cases involve damage or blockage in the tubes.
Looking at research, we find:
|
Study |
Prevalence of Tubal Factors |
Sample Size |
|---|---|---|
|
Study A |
28% |
500 |
|
Study B |
32% |
750 |
|
Study C |
25% |
1000 |
Why 25-35% of Infertility Cases Involve Tubal Issues
Several reasons explain why tubal factors are so common in infertility. These include pelvic inflammatory disease (PID), endometriosis, and past surgeries. These can cause scarring and blockages in the tubes.
Pelvic inflammatory disease is a big risk for tubal damage. It’s common in women of childbearing age and often leads to scarring and infertility.
Knowing about tubal factors in female infertility is vital. It helps doctors find better ways to diagnose and treat. By understanding the causes, they can help women get pregnant.
The HSG Procedure: A Step-by-Step Guide
HSG, or Hysterosalpingogram, is a special X-ray test. It checks the uterus and fallopian tubes. It’s key for finding fertility problems, like issues with the uterus or fallopian tubes.
Pre-Procedure Preparation
Before the HSG test, there are steps to take:
- Book the test in the first half of your menstrual cycle, between days 7-14. This avoids pregnancy and lessens discomfort.
- Tell your doctor about any allergies, like to contrast media or iodine.
- Share any medicines you’re taking.
- Some doctors might suggest an anti-anxiety pill or ibuprofen beforehand to ease discomfort.
During the HSG Test: What Happens
The HSG procedure includes several steps:
- The patient lies on an examination table, slightly tilted.
- A speculum is put in the vagina to see the cervix.
- A catheter is gently put through the cervix into the uterus.
- A contrast medium is slowly injected through the catheter to fill the uterus and fallopian tubes.
- X-ray images are taken as the contrast medium moves through the reproductive structures.
- The flow of the contrast medium is watched on a fluoroscope. This lets the doctor see any blockages or problems.
|
Procedure Step |
Description |
|---|---|
|
1. Positioning |
Patient is positioned on an examination table. |
|
2. Speculum Insertion |
A speculum is inserted to visualize the cervix. |
|
3. Catheter Insertion |
A catheter is inserted through the cervix into the uterus. |
|
4. Contrast Injection |
Contrast medium is injected to fill the uterine cavity and fallopian tubes. |
|
5. X-ray Imaging |
X-ray images are taken as the contrast medium flows through the reproductive structures. |
Post-Procedure Care and Recovery
After the HSG test, you can usually go back to normal activities right away. But, you might feel:
- Mild cramping, which can be eased with over-the-counter pain relievers.
- Spotting or light bleeding, which usually goes away on its own.
- Dizziness or nausea, which is usually short-lived.
It’s wise to:
- Avoid using tampons or having sex for a day or two after the procedure.
- Call your healthcare provider if you have severe pain, heavy bleeding, or signs of infection.
Knowing about the HSG procedure can help ease worries and prepare you for your fertility check-up.
Diagnostic Accuracy of HSG in Detecting Tubal Blockages
Understanding HSG’s accuracy is key to knowing its role in finding tubal blockages. HSG, or Hysterosalpingogram, is a vital tool in fertility tests. It gives insights into the fallopian tubes’ health.
The accuracy of HSG is measured by its sensitivity and specificity rates. Sensitivity shows how well it spots tubal blockages. Specificity shows how well it misses them.
Sensitivity and Specificity Rates
Research shows HSG’s sensitivity is about 80% for finding tubal blockages. This means it correctly spots blockages in 80% of cases. But, specificity rates vary, usually between 70% to 90%.
Understanding the 80% Diagnostic Sensitivity for Tubal Occlusion
The 80% sensitivity of HSG for tubal occlusion means it’s reliable but not perfect. It misses blockages in about 20% of cases. This highlights the need to look at HSG results with the patient’s overall health in mind.
Many factors can affect HSG’s accuracy. These include the practitioner’s skill, the equipment quality, and the patient’s tubal condition.
Interpreting HSG Results: What Your Doctor Sees
The HSG test gives insights into your uterine cavity and fallopian tubes’ health. Your doctor looks for certain signs of your reproductive health when reviewing your HSG results.
Normal Uterine Cavity and Patent Tubes
A normal HSG result shows a symmetrical and smooth uterine cavity. The contrast material should fill it evenly without defects. Also, patent fallopian tubes are shown by free contrast material spillage into the pelvic cavity.
When both tubes are patent, it means there are no big blockages. This is good for egg fertilization and embryo travel to the uterus.
Identifying Abnormalities and Blockages
Abnormal HSG results can show fertility issues. Common problems include:
- Filling defects in the uterine cavity, which could be polyps, fibroids, or adhesions.
- Tubal blockages, where contrast material doesn’t spill into the pelvic cavity, showing an obstruction.
- Tubal damage or abnormalities, like dilation or irregular tube shapes.
These findings help your doctor find the cause of infertility. They can then suggest the right treatment.
The Significance of Contrast Spillage
Contrast spillage during an HSG test is a critical indicator of tubal patency. Free spillage into the pelvic cavity means at least one tube is open. The presence or absence of spillage helps your doctor plan your fertility journey.
Understanding your HSG results is key for your fertility journey. Your doctor will talk about the findings with you. They will then create a treatment plan tailored to your needs.
Potential Therapeutic Effects of HSG Beyond Diagnosis
HSG is not just for diagnosing issues. It also has therapeutic effects on fertility. This has caught the attention of many in the medical field, mainly fertility experts.
The “Flushing” Phenomenon and Fertility Enhancement
The “flushing” phenomenon is a key part of HSG’s benefits. The contrast material used in the procedure might clear out debris and blockages in the fallopian tubes. This could improve tubal patency and boost fertility.
Some patients see better fertility after HSG, even without blockages found. This suggests that flushing the tubes can help. It might remove small blockages or enhance tubal function.
Research on Pregnancy Rates Following HSG
Many studies have looked into HSG’s impact on pregnancy rates. While findings vary, most show HSG can improve fertility. Some studies found higher pregnancy rates after HSG, even without other treatments.
A meta-analysis showed a higher pregnancy rate after HSG. But, the quality of evidence differs, and more research is needed. This will help us understand HSG’s full benefits.
HSG’s therapeutic effects show how diagnosis and treatment are linked in fertility care. As research continues, HSG remains a key tool in managing infertility.
Risks, Side Effects, and Complications of HSG
HSG is a key tool for checking fertility. But, it’s important to know the possible risks and side effects.
Common Discomfort and Expected Side Effects
Most women feel some pain during HSG, like mild menstrual cramps. Some might also see:
- Mild spotting or vaginal bleeding
- Dizziness or lightheadedness
- Nausea
- A feeling of pressure in the pelvic area
These effects usually go away quickly after the test.
Rare but Serious Complications to Be Aware Of
Even though rare, serious issues can happen with HSG. These include:
- Infection: Pelvic inflammatory disease (PID) is a risk, mainly if there’s an existing infection or if the procedure isn’t done properly.
- Allergic reactions: Some might be allergic to the dye used in HSG.
- Vasovagal reaction: This can cause a sudden drop in heart rate and blood pressure, leading to fainting.
- Damage to the reproductive organs: Though very rare, there’s a chance of perforating the uterus or harming the fallopian tubes.
Contraindications for HSG Testing
HSG isn’t right for everyone. It’s not for:
- Known or suspected pregnancy
- Active pelvic infection
- Known severe iodine allergy (for contrast dye)
- Recent pelvic surgery or uterine bleeding
Talking to your doctor about your health history and worries is key before getting an HSG.
Modern Guidelines for HSG in Fertility Evaluation
Today, HSG is key in checking fertility. It helps see if the tubes are open and if the uterus is normal.
When HSG is Recommended in the Fertility Workup
Women with unexplained infertility or suspected tubal disease should get an HSG. It shows if the tubes are open, helping doctors plan the next steps.
The American Society for Reproductive Medicine (ASRM) and others say HSG is a top choice for some. It’s good for checking the tubes and the uterus.
Integration with Other Diagnostic Procedures
HSG often goes hand-in-hand with other tests. This gives a full picture of fertility. Tests might include:
- Transvaginal ultrasound
- Hysteroscopy
- Laparoscopy
Together, these tests help doctors understand infertility better. They can then make treatment plans that fit each person’s needs.
|
Diagnostic Procedure |
Purpose |
Integration with HSG |
|---|---|---|
|
HSG |
Assess tubal patency and uterine cavity |
Primary diagnostic tool |
|
Transvaginal Ultrasound |
Evaluate ovarian reserve and uterine anatomy |
Complementary to HSG |
|
Hysteroscopy |
Direct visualization of uterine cavity |
Confirmatory after HSG |
|
Laparoscopy |
Examine pelvic anatomy and tubal function |
Used when HSG indicates tubal disease |
Knowing about HSG’s role in fertility is important. It helps doctors and patients get a clear diagnosis. This leads to better treatment plans.
Alternative and Complementary Procedures to HSG
HSG is key in checking fertility, but other methods can help too. These methods give extra info or work better in certain cases.
Sonohysterography (SHG): Ultrasound Alternative
Sonohysterography, or saline infusion sonography, uses ultrasound with saline in the uterus. It’s a good choice instead of HSG for looking at the uterus without X-rays.
Advantages of SHG:
- Shows the uterus in detail
- No X-rays needed
- Can be done in a doctor’s office
- Looks at other pelvic areas too
Hysteroscopy: Direct Visualization Method
Hysteroscopy lets you see inside the uterus with a thin, lighted scope. It can find and fix problems inside the uterus.
Benefits of hysteroscopy include:
- Sees the uterus up close
- Can take biopsies or remove growths
- Finds problems accurately
Laparoscopy: Surgical Diagnostic Approach
Laparoscopy is a surgery that looks at the pelvic organs. It’s more invasive than HSG or SHG but can fix problems at the same time.
Key aspects of laparoscopy:
- Looks at the outside of the tubes and ovaries
- Can treat issues like endometriosis or adhesions
- Needs general anesthesia and is more invasive
In summary, while HSG is important, other methods like sonohysterography, hysteroscopy, and laparoscopy help too. The right choice depends on the patient’s needs and what they need to know about their fertility.
Impact of Untreated Tubal Issues on Fertility Outcomes
Untreated tubal blockages can greatly lower a woman’s chance of getting pregnant naturally. Tubal issues are a big factor in fertility. They can stop the egg from being fertilized or the embryo from attaching to the uterus.
Natural Conception Rates with Tubal Blockage
Women with untreated tubal blockages have much lower chances of getting pregnant naturally. Studies show that tubal blockage can cut conception rates by up to 50%.
|
Tubal Condition |
Conception Rate |
|---|---|
|
Normal Tubal Function |
20% |
|
Unilateral Tubal Blockage |
10% |
|
Bilateral Tubal Blockage |
Less than 2% |
The Less Than 2% Monthly Conception Rate Explained
The monthly conception rate for women with both fallopian tubes blocked is less than 2%. This low rate is because both tubes are blocked, stopping the egg from being fertilized. In such cases, IVF is often needed for conception.
Key factors influencing conception rates with tubal blockage include:
- The extent of tubal damage
- The presence of other fertility issues
- The woman’s age
In conclusion, untreated tubal issues can greatly affect fertility outcomes. Knowing the natural conception rates with tubal blockage helps people make better choices about their fertility treatments.
Advanced HSG Techniques and Technological Innovations
New technologies have changed HSG procedures for the better. They offer better diagnosis and care for patients. The field of fertility testing keeps getting better, thanks to new imaging tech.
Digital Fluoroscopy and Reduced Radiation Exposure
Digital fluoroscopy is a big step forward in HSG. It gives clear images in real-time with less radiation than old methods. Digital fluoroscopy makes images better, helping doctors see if tubes are open or not.
This means patients get less radiation, making them safer. Plus, doctors can save and share images easily.
3D Reconstruction and Enhanced Diagnostic Capability
3D reconstruction is another cool thing in HSG. It uses many images to show the uterus and tubes in 3D. This clear view helps find tricky problems and makes diagnoses more accurate.
|
Technological Innovation |
Benefits |
Impact on HSG |
|---|---|---|
|
Digital Fluoroscopy |
Lower radiation exposure, real-time imaging |
Improved patient safety, enhanced image quality |
|
3D Reconstruction |
Comprehensive visualization, detailed anatomy |
Improved diagnostic accuracy, better detection of abnormalities |
HSG Costs, Insurance Coverage, and Accessibility in the US
The cost of HSG and other fertility tests is a big worry for many in the US. It affects how people decide on their fertility treatments. Knowing the costs, insurance, and where to get these tests is key.
Average Procedure Costs and Regional Variations
HSG costs can change a lot based on where you are, who you see, and where you go. On average, it costs between $300 and $1,000 in the US. But, prices can go up in big cities or if you get extra services.
|
Region |
Average Cost |
|---|---|
|
Northeast |
$450 – $900 |
|
South |
$350 – $800 |
|
West Coast |
$500 – $1,000 |
Navigating Insurance Coverage for Fertility Testing
Insurance for HSG can differ a lot. Some plans cover it for fertility tests, but others don’t. Always check your insurance before you get the test.
Key factors influencing insurance coverage:
- Type of insurance plan
- Policy specifics regarding fertility testing
- Deductibles and copays
Financial Assistance Options for Fertility Diagnostics
If money is tight, there are ways to help with HSG and fertility tests. Look into financial help programs, grants, and clinics with sliding scale fees.
Knowing about costs, insurance, and help options can help you make better choices for your fertility care.
Multidisciplinary Approaches to Fertility Care
Fertility issues are complex and need a team effort to solve. Today, fertility care involves many medical fields working together. This teamwork helps create detailed treatment plans for each patient.
Top fertility centers use integrated treatment protocols. They bring together reproductive endocrinologists, urologists, geneticists, and mental health experts. This team approach ensures patients get a full check-up and a treatment plan that fits them.
Integrated Treatment Protocols at Leading Fertility Centers
Leading fertility centers use a mix of tests and treatments. They tailor their care to meet each patient’s needs. This approach boosts the chances of getting pregnant.
|
Discipline |
Role in Fertility Care |
Key Contributions |
|---|---|---|
|
Reproductive Endocrinology |
Diagnosis and treatment of hormonal imbalances |
Hormone regulation, ovulation induction |
|
Urology |
Evaluation and treatment of male factor infertility |
Semen analysis, vasectomy reversal |
|
Genetics |
Genetic screening and counseling |
PGD, genetic risk assessment |
|
Mental Health |
Support and counseling for patients |
Stress management, emotional support |
Case Study: Liv Hospital’s Innovative Fertility Approaches
Liv Hospital is a great example of a center using innovative fertility approaches. Their team combines different medical fields to offer the latest treatments and care.
Liv Hospital’s methods include advanced tests like genetic screening and 3D ultrasound. They also offer IVF and egg freezing. Their focus on new research and technology makes them a top choice in fertility care.
The success of team-based fertility care is clear at places like Liv Hospital. By working together and using the latest technology, these centers help more people have babies.
Conclusion: Making Informed Decisions About HSG in Your Fertility Journey
Understanding HSG’s role in fertility is key for those on their fertility journey. HSG is a valuable tool that checks the health of the fallopian tubes. This is important for getting pregnant.
We’ve cleared up the confusion between HSC and HSG. HSG is the right term for checking fertility. It helps find blockages in the tubes and can even help treat them.
Thinking about HSG means looking at its benefits and risks. Today’s guidelines say HSG is a top choice for checking fertility. It’s often used with other tests like sonohysterography or hysteroscopy.
Deciding on HSG is about knowing its place in your fertility care. Using HSG in a full fertility check can help you understand your reproductive health. This way, you can make smart choices about your treatment.
FAQ
What does HSC stand for in fertility testing?
HSC is often confused with HSG, which is short for Hysterosalpingogram. It’s a tool used to check fertility.
What is the difference between HSC and HSG?
HSG is the real term for fertility testing. It checks the fallopian tubes and uterus. HSC is not a recognized term here.
What is the purpose of an HSG test?
The HSG test checks if the fallopian tubes are open and the uterus is shaped right. It helps find why someone might not be able to get pregnant.
How is HSG performed?
For HSG, a special dye is put through the cervix. Then, X-rays show the inside of the uterus and tubes.
What are the therapeutic effects of HSG?
Some studies say HSG might help with fertility. It could clean out the fallopian tubes.
What are the risks and side effects associated with HSG?
Side effects like pain and cramps are common. But, serious problems like infection or allergic reactions are rare.
Are there alternative diagnostic procedures to HSG?
Yes, there are other tests like sonohysterography (SHG), hysteroscopy, and laparoscopy. Each has its own benefits and uses.
How do untreated tubal issues affect fertility outcomes?
If tubal problems aren’t treated, getting pregnant is very hard. The chances are often less than 2% each month.
What are the costs associated with HSG, and is it covered by insurance?
HSG costs vary. Insurance coverage depends on the policy. There might be ways to get help with the cost.
What are the benefits of advanced HSG techniques?
Newer HSG methods like digital fluoroscopy and 3D images are better. They help find problems more accurately and use less radiation.
Why is a multidisciplinary approach important in fertility care?
Using many different tests and treatments together helps a lot. It gives better care and can improve chances of getting pregnant.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK572146/