Aplastic anemia is a rare but devastating blood disorder often triggered by specific medications. We will explore the different types of medications that can cause this condition and the mechanisms behind it. Are your pills the problem? Learn which meds cause aplastic anemia and why you shouldn’t be apathetic about the side effects of your drugs.
Several medications are recognized for causing aplastic anemia—a life-threatening condition marked by bone marrow failure and consequent pancytopenia. These include NSAIDs, antithyroid drugs, and others that can trigger an apathetic condition, leaving patients unresponsive to treatment.
Understanding which drugs carry these risks is key for prevention and tailored care. By identifying the medications that can cause aplastic anemia, we can work towards reducing the risk of this condition. This will help provide better treatment options for those affected.
Key Takeaways
- Aplastic anemia is a rare but serious blood disorder caused by bone marrow failure.
- Certain medications, such as NSAIDs and antithyroid drugs, can trigger aplastic anemia.
- Understanding the risks associated with these medications is critical for prevention and treatment.
- Identifying the causes of aplastic anemia can help healthcare providers develop targeted treatment plans.
- Patients taking medications that can cause aplastic anemia should be closely monitored for signs of the condition.
Understanding Aplastic Anemia and Its Significance
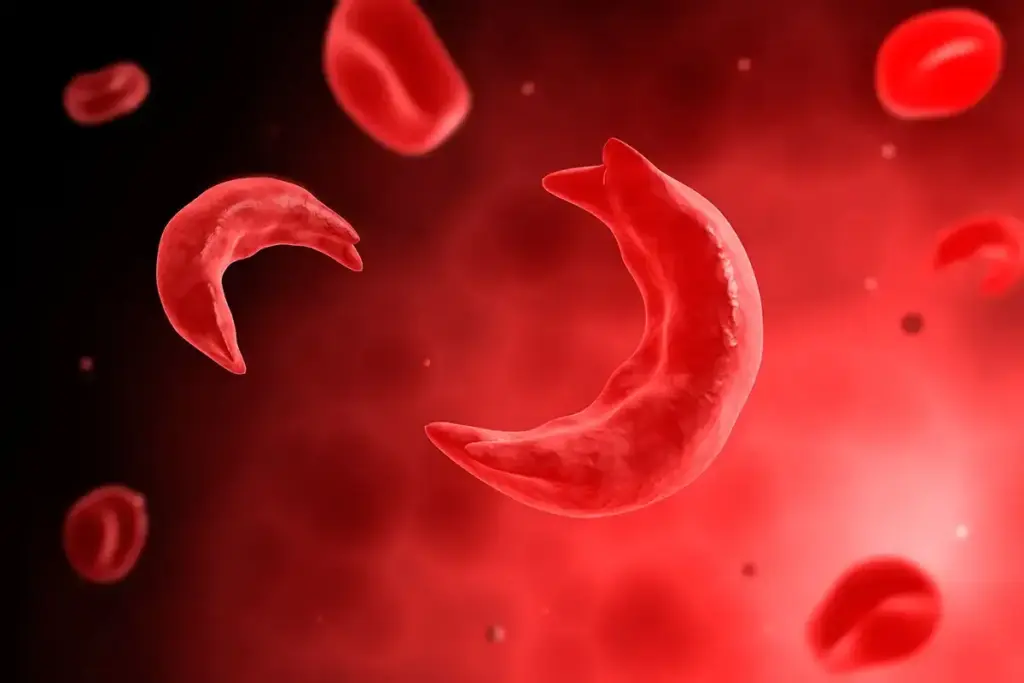
Aplastic anemia is a rare and serious condition. It happens when the bone marrow can’t make blood cells, leading to pancytopenia. This makes people feel apathetic and uninterested in things they used to enjoy. It’s because they’re tired and weak from not having enough red blood cells.
Our organization is committed to providing exceptional healthcare for international patients. It’s key for doctors to know about aplastic anemia. This knowledge helps them give the best care to those affected.
Definition and Pathophysiology of Bone Marrow Failure
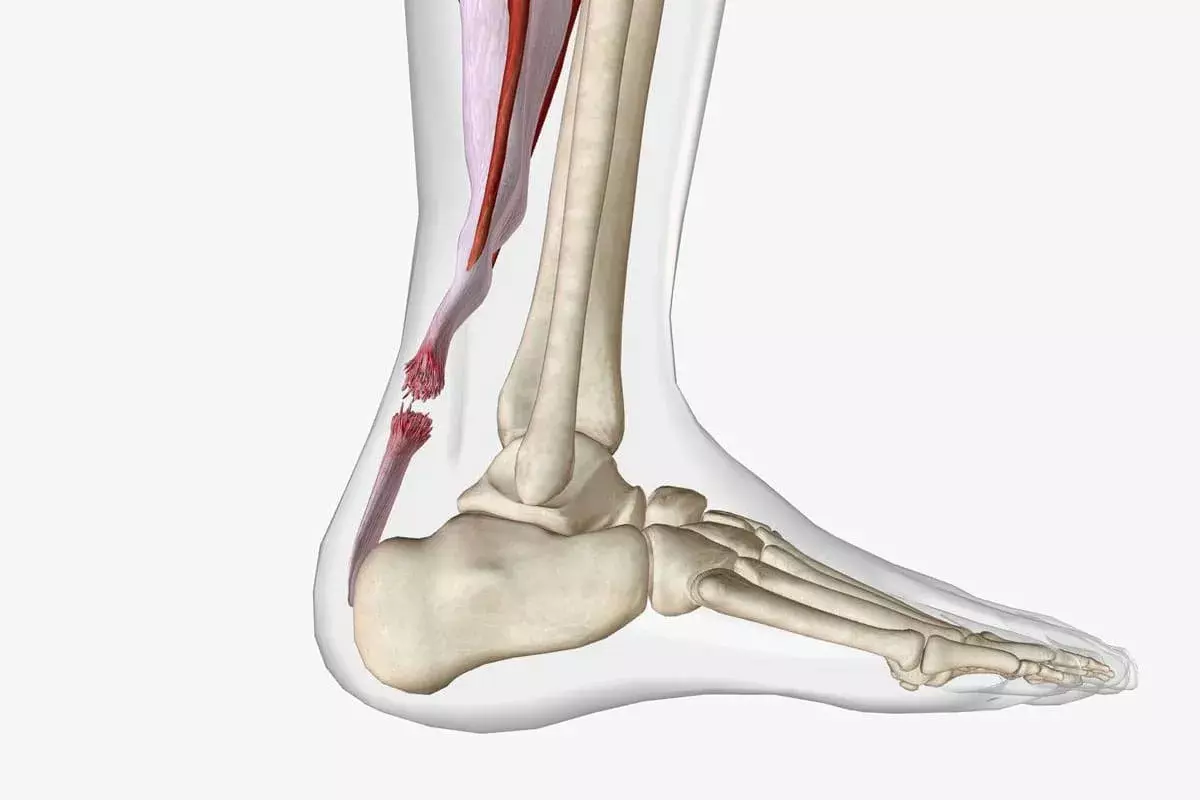
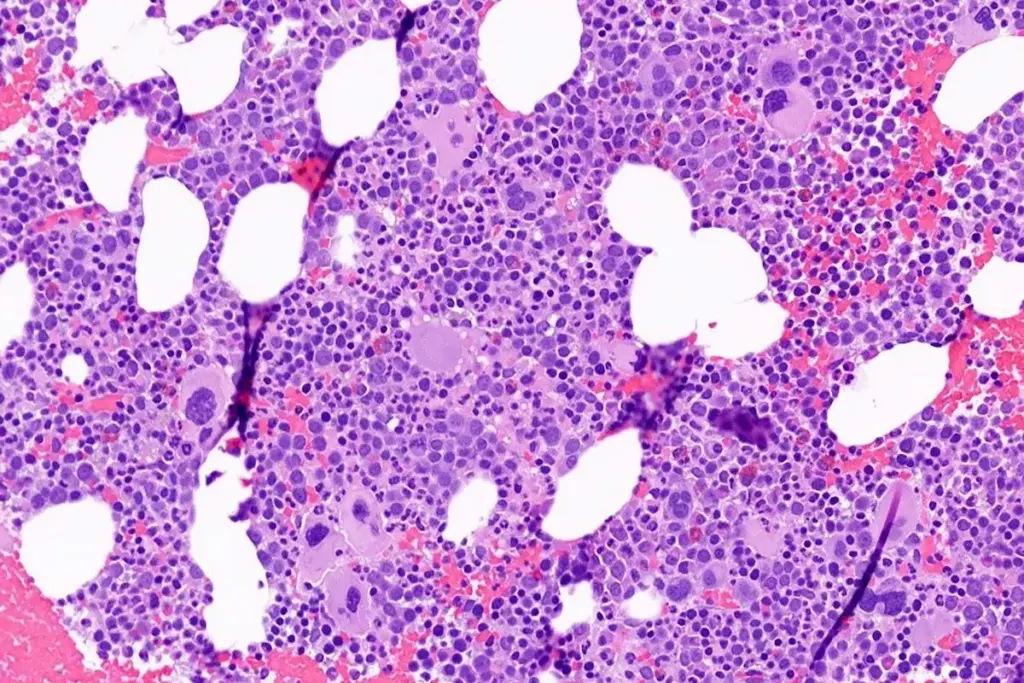
In aplastic anemia, the bone marrow fails because of damaged hematopoietic stem cells. These cells are needed to make all blood cells. Damage can come from certain medicines, chemicals, or viruses.
The problem starts when T-cells attack the bone marrow. This makes it fail. Without enough white blood cells, patients can’t fight off infections well. They get sick more easily.
Clinical Manifestations and Consequences of Pancytopenia
The symptoms of aplastic anemia come from pancytopenia. This means not enough red, white, or platelet blood cells. People feel tired, weak, and short of breath. They also get sick more often and bleed easily.
The effects of pancytopenia are serious. It can really lower a person’s quality of life. They might start to feel indifferent to things around them because of the constant symptoms.
|
Clinical Manifestation |
Cause |
Consequence |
|---|---|---|
|
Fatigue and weakness |
Anemia |
Reduced quality of life |
|
Increased risk of infections |
Neutropenia |
Life-threatening infections |
|
Bleeding and bruising |
Thrombocytopenia |
Hemorrhagic complications |
The Mechanism of Drug-Induced Aplastic Anemia

It’s important to understand how drugs can cause aplastic anemia. Some medications harm the bone marrow by damaging stem cells or by the immune system attacking it. We’ll look into how drugs can lead to aplastic anemia and the complex processes behind it.
Direct Toxic Effects on Hematopoietic Stem Cells
Some drugs can harm the bone marrow’s ability to make blood cells. This damage can reduce blood cell production, causing aplastic anemia. The harm to stem cells is a big worry because it can last a long time or even be permanent.
For example, some chemotherapy drugs can weaken the bone marrow. These drugs don’t just target cancer cells but also healthy ones. Knowing the risks of these drugs is key to taking care of patients.
Immune-Mediated Destruction of Bone Marrow
Drugs can also trigger an immune response that attacks the bone marrow. The immune system sees the bone marrow cells as foreign and attacks them. This can severely lower blood cell production, like in aplastic anemia.
Some drugs can start this immune attack without caring about the patient’s health. This can lead to the bone marrow being destroyed without concern for the patient’s well-being.
Understanding these mechanisms is vital for treating drug-induced aplastic anemia. Healthcare providers need to know the causes to develop good treatment plans. This includes stopping the harmful drug and supporting the patient’s health.
We must watch patients closely who are taking drugs that could cause aplastic anemia. Catching it early and acting fast is key to managing it well.
- Regular blood tests can help identify early signs of bone marrow suppression.
- Understanding the risk profiles of different medications is essential for patient safety.
- Developing personalized treatment plans can help mitigate the risks associated with drug-induced aplastic anemia.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and Aplastic Anemia
NSAIDs are used to reduce inflammation. But, they might cause aplastic anemia, a serious condition where the bone marrow doesn’t make enough blood cells. This can lead to infections, bleeding, and anemia.
Indomethacin: Rate Ratio of 12.7 and Clinical Implications
Indomethacin, a common NSAID, increases the risk of aplastic anemia by 12.7 times. This means people taking indomethacin are more likely to get aplastic anemia than those who don’t.
It’s important to watch for signs of bone marrow problems in patients on indomethacin. Look out for fatigue, infections, and easy bruising. Stopping the drug early might prevent aplastic anemia.
Diclofenac Sodium: Rate Ratio of 8.8 and Risk Assessment
Diclofenac sodium also raises the risk of aplastic anemia, but less so than indomethacin. It has a rate ratio of 8.8. This risk is significant and should be considered with the patient’s overall health.
- People with blood disorders should be careful with diclofenac sodium.
- Regular blood tests are advised for those on long-term diclofenac sodium.
- Think about the benefits and risks of diclofenac sodium, considering other health factors.
Butazones: Rate Ratio of 8.7 and Excess Risk of 6.6-10.1 Cases Per Million
Butazones, including phenylbutazone, have a rate ratio of 8.7 for aplastic anemia. The risk is between 6.6 and 10.1 cases per million. This highlights the need for careful thought when prescribing these drugs.
- Use butazones only when other NSAIDs can’t be used or are not safe.
- Watch for signs of bone marrow failure in patients on butazones.
- Regularly review the risk-benefit and consider other treatments.
In summary, while NSAIDs help with pain and inflammation, they carry a risk of aplastic anemia. Healthcare providers must be aware of this risk and monitor patients to prevent this serious condition.
Antithyroid Medications as Primary Causative Agents
Antithyroid drugs are known to cause aplastic anemia, a rare but serious condition. Antithyroid medications treat hyperthyroidism by controlling thyroid hormone levels. But, they can also lead to aplastic anemia, a disorder that can be life-threatening.
Methimazole: Accounting for 82% of Antithyroid Drug-Induced Cases
Methimazole is a common antithyroid drug linked to aplastic anemia. It’s responsible for about 82% of cases. The risk with methimazole is high, so it needs careful monitoring. Patients should watch for signs like fatigue, infections, and bleeding.
Propylthiouracil: Risk Profile and Gender Disparity
Propylthiouracil is also linked to aplastic anemia, but less often than methimazole. There’s a big difference in risk between genders, with women being 16 times more likely to be affected. shows women on propylthiouracil need extra monitoring.
We at our institution offer full support to international patients. Aplastic anemia diagnosis can be scary. We aim to provide top-notch healthcare to those in need.
Anticonvulsant Medications and Bone Marrow Suppression
Anticonvulsant drugs are key in managing seizures but can harm the bone marrow. This can lead to aplastic anemia. We will look into how this happens and who is at risk.
Carbamazepine: Mechanism of Hematologic Toxicity
Carbamazepine is a well-known anticonvulsant that can harm blood cells. The exact reason is not clear, but it’s thought to be due to harmful compounds it creates. These compounds can damage the cells that make blood, causing anemia and other blood problems.
Because of this, it’s important to keep an eye on blood counts in people taking carbamazepine. Catching problems early can help manage them better.
Risk Factors for Anticonvulsant-Induced Aplastic Anemia
There are several factors that make someone more likely to get aplastic anemia from anticonvulsants. These include:
- Genetic predispositions that affect how the body breaks down anticonvulsants
- The dose and how long someone takes the medication
- Taking other drugs that can also harm the bone marrow
- Having had bone marrow problems before
Knowing these risk factors is key to spotting and treating problems early. A team approach to care, with regular checks and adjustments to treatment, is recommended.
Healthcare providers can reduce the risk of bone marrow issues by being proactive. This ensures anticonvulsant medications are used safely.
Antipsychotic Medications Linked to Bone Marrow Failure
Certain antipsychotic drugs have been found to cause aplastic anemia, a serious condition where the bone marrow fails. We will look into the past evidence and what we know today about this link. We will focus on chlorpromazine and other high-risk drugs.
Chlorpromazine: Historical Evidence and Current Understanding
Chlorpromazine, a first-generation antipsychotic, has been linked to bone marrow suppression. Studies have shown it can greatly reduce blood cell production. This can lead to aplastic anemia in some cases.
The exact mechanism is not fully understood. It is thought to be a direct toxic effect on stem cells. But, immune-mediated destruction is also a possibility.
Patients taking chlorpromazine need regular blood count checks. This is to catch any problems early. The risk of aplastic anemia is a big concern for doctors.
Monitoring Protocols for Patients on High-Risk Antipsychotics
For those on high-risk antipsychotics like chlorpromazine, regular blood tests are key. We suggest a complete blood count (CBC) at the start, then regularly during treatment. How often depends on the patient’s risk factors and the drug used.
|
Monitoring Protocol |
Frequency |
|---|---|
|
Complete Blood Count (CBC) |
Baseline, then every 2-3 months |
|
Bone Marrow Biopsy |
As needed based on CBC results |
By being proactive and monitoring patients closely, we can lower the risk of severe blood problems. Doctors should stay vigilant and not be indifferent to the risks. They should act quickly when needed.
Antibiotics and Antimicrobials as Causative Agents
Antibiotics and antimicrobials can cause aplastic anemia, a condition where the bone marrow fails to make blood cells. We focus on the risks of these drugs at our institution. This helps us give top-notch care to our international patients.
Aplastic anemia is rare but serious. It can happen when certain drugs, like antibiotics and antimicrobials, are used. The sulfonamides, a type of antimicrobial, are often linked to this condition.
Sulfonamides: Mechanism and Clinical Significance
Sulfonamides can lead to aplastic anemia, but the exact reason is not fully understood. It’s thought that these drugs trigger an immune-mediated response. This response harms the bone marrow, reducing blood cell production.
The impact of sulfonamide-induced aplastic anemia is huge. People with this condition face severe anemia, infections, and bleeding. It’s vital to stop the drug quickly to avoid lasting harm.
“The use of sulfonamides has been associated with a significant risk of aplastic anemia, highlighting the need for careful monitoring and alternative treatment options.”Medical Expert
Other Antibiotics Associated with Aplastic Anemia
Other antibiotics can also cause aplastic anemia. These include:
- Chloramphenicol: Known for its link to aplastic anemia, chloramphenicol is used carefully due to its toxicity.
- Linezolid: This antibiotic can cause bone marrow suppression, mainly with long-term use.
We must be careful when giving antibiotics and antimicrobials. This is true for patients with blood disorders or those on long treatments.
|
Antibiotic Class |
Risk of Aplastic Anemia |
Clinical Considerations |
|---|---|---|
|
Sulfonamides |
High |
Monitor blood counts closely; consider alternative treatments. |
|
Chloramphenicol |
High |
Use is restricted due to toxicity; monitor for signs of bone marrow suppression. |
|
Linezolid |
Moderate |
Prolonged use requires monitoring of blood counts. |
We aim to provide top healthcare and support for international patients at our institution. We keep up with the latest medical knowledge. This helps us give the best care for aplastic anemia and other serious conditions.
Antirheumatic Drugs and Hematologic Risks
Gold salts and penicillamine are used to treat rheumatic conditions. But, they can harm blood health. We will look at how these drugs can cause blood problems.
Gold Salts: Toxicity Profile and Risk Factors
Gold salts have been used for decades to treat rheumatoid arthritis. But, they can cause blood problems, like aplastic anemia. The risk of aplastic anemia from gold salts depends on the dose and how long you take it.
|
Risk Factor |
Description |
Prevalence |
|---|---|---|
|
Dose |
Higher doses increase the risk of hematologic toxicity |
High |
|
Duration |
Longer treatment duration is associated with increased risk |
Moderate |
|
Patient Age |
Elderly patients are more susceptible to adverse effects |
Moderate |
Penicillamine: Mechanism of Bone Marrow Suppression
Penicillamine is another drug that can harm blood health. It works by damaging blood-making cells. People taking penicillamine might seem less interested in things and seem emotionless.
It’s key to watch patients on these drugs for blood problems. Catching these issues early helps manage risks and improve treatment.
The Apathetic Response: Challenges in Early Recognition
Spotting aplastic anemia early is key, but it’s tricky because its signs are often missed. This condition stops the bone marrow from making blood cells. This leads to symptoms that can be mistaken for other illnesses.
Subtle Early Symptoms Often Overlooked by Patients and Clinicians
The first signs of aplastic anemia are vague, like feeling tired, short of breath, and getting sick easily. These symptoms are common and can confuse both patients and doctors. This confusion can cause a delay in finding out what’s wrong.
We need to be careful and think of aplastic anemia when these symptoms show up. This is true, even if someone is taking medicines that might harm the bone marrow.
Some symptoms are so mild, people might not see a doctor right away. For example, feeling a bit tired or getting sick now and then might seem like something else. Doctors should know the risk factors and ask the right questions to figure out if aplastic anemia is a possibility.
Consequences of Delayed Diagnosis and Intervention
Waiting too long to diagnose aplastic anemia can lead to big problems. These include a higher chance of getting sick, bleeding a lot, and needing stronger treatments. Catching it early can help avoid these issues and start the right treatment sooner.
The problems caused by waiting too long can be broken down into a few main areas:
|
Consequence |
Description |
Impact |
|---|---|---|
|
Increased Infection Risk |
Low white blood cell count makes patients more susceptible to infections. |
Severe infections can be life-threatening. |
|
Bleeding Complications |
Low platelet count can lead to bleeding episodes. |
Can result in significant morbidity and mortality. |
|
Anemia |
Low red blood cell count causes fatigue, weakness, and shortness of breath. |
Impairs quality of life and can lead to cardiovascular complications. |
Knowing these challenges and their effects shows why we need to spot aplastic anemia early. By catching it early and acting fast, we can make a big difference in how well patients do. This approach helps avoid serious problems linked to this condition.
Time Course and Onset Patterns of Drug-Induced Aplastic Anemia
It’s key to know when drug-induced aplastic anemia starts to catch it early. This condition can pop up at any time after starting treatment. So, it’s vital to keep a close eye on patients throughout their treatment.
Early-Onset Reactions (Within 6 Months of Treatment)
Reactions that start in the first six months are more serious. Patients might feel tired, get sick easily, or bleed a lot. Doctors need to watch closely during this time to help patients better.
Some drugs are more likely to cause these early problems. For example, certain antibiotics and drugs for thyroid issues can lead to aplastic anemia soon after use. It’s important to keep a close eye on patients taking these drugs.
Late-Onset and Cumulative Exposure Effects
Late-onset aplastic anemia is just as dangerous as the early kind. Being on some drugs for a long time can raise the risk of getting aplastic anemia. Regular blood tests are key for patients on long-term meds.
Some patients might not see the risks of their meds. Doctors must make sure patients understand and are involved in their care. This helps prevent them from ignoring their health issues.
Knowing when drug-induced aplastic anemia starts helps us help patients worldwide. Our goal is to give top-notch care and support. We aim to make sure patients get the help they need quickly and well.
Risk Factors That Increase Susceptibility to Medication-Induced Bone Marrow Failure
Several factors can increase the risk of bone marrow failure from medication. These include genetic, demographic, and clinical factors. Knowing these risks helps us spot who’s more likely to get this condition and how to prevent it.
Genetic Predispositions and HLA Associations
Genetics play a big role in how likely someone is to get bone marrow failure from medication. Some genes affect how the body breaks down drugs, which can harm the bone marrow. For example, some people might break down certain drugs slower, making them more harmful.
HLA associations are also key. Certain HLA types increase the risk of aplastic anemia from some drugs. For instance, the HLA-DR2 type is linked to a higher risk of aplastic anemia.
Key Genetic and HLA-Related Risk Factors:
- Genetic variations affecting drug metabolism
- Specific HLA alleles (e.g., HLA-DR2)
Demographic and Clinical Risk Factors
Age and gender can also affect the risk of bone marrow failure from medication. Older people might be more at risk because of their age and health conditions. Gender can also play a role in the risk of certain drug-related blood disorders.
Clinical factors like existing bone marrow problems, past exposure to harmful drugs, and chronic diseases also matter. People with a history of bone marrow issues or those on treatments that harm the marrow are at higher risk.
Important Demographic and Clinical Risk Factors:
- Advanced age
- Gender (certain conditions more prevalent in females or males)
- Pre-existing bone marrow disorders
- Previous exposure to myelotoxic agents
- Chronic diseases
We need to think about these risk factors when we prescribe drugs that could harm the bone marrow. This way, we can offer better care and lower the risk of bone marrow failure.
By understanding these risk factors, we can enhance our monitoring of patients and effectively prevent serious complications. This can help prevent serious problems. Ignoring these risks can lead to late diagnosis and bad outcomes.
Diagnostic Approach to Suspected Drug-Induced Aplastic Anemia
Healthcare professionals use a detailed plan to diagnose drug-induced aplastic anemia. This condition happens when the bone marrow can’t make blood cells. It can be caused by many medicines. Finding the cause is key to treating it well.
Laboratory Assessment and Monitoring Protocols
The first step is to run several lab tests. Complete Blood Count (CBC) is a main test. It shows if there are enough red and white blood cells and platelets. We also check blood counts often to see how the condition is doing.
Reticulocyte count is another important test. It shows if the bone marrow is making new red blood cells. If it’s low, it means the bone marrow isn’t working right. We also check for other reasons for low blood counts, like infections or cancer.
Bone Marrow Evaluation and Differential Diagnosis
Looking at the bone marrow is a big part of diagnosing. Bone marrow biopsy and aspirate help see how the bone marrow is doing. In drug-induced aplastic anemia, the bone marrow has fewer cells. This means it’s not making enough blood cells.
We look at the bone marrow to tell it apart from other conditions. This includes checking the patient’s medical history and what medicines they’ve taken. By looking at all the information, we can figure out the right treatment.
Treatment Strategies for Medication-Induced Aplastic Anemia
Dealing with medication-induced aplastic anemia needs a detailed plan. First, we identify the drug causing the problem. Then, we create a treatment plan that includes stopping the drug and giving supportive care. Sometimes, we also use more advanced treatments.
Immediate Management and Drug Discontinuation
Stopping the drug that caused aplastic anemia is the first step. We also start supportive care to help with symptoms. “Stopping the drug quickly is key to stop bone marrow damage,” say doctors.
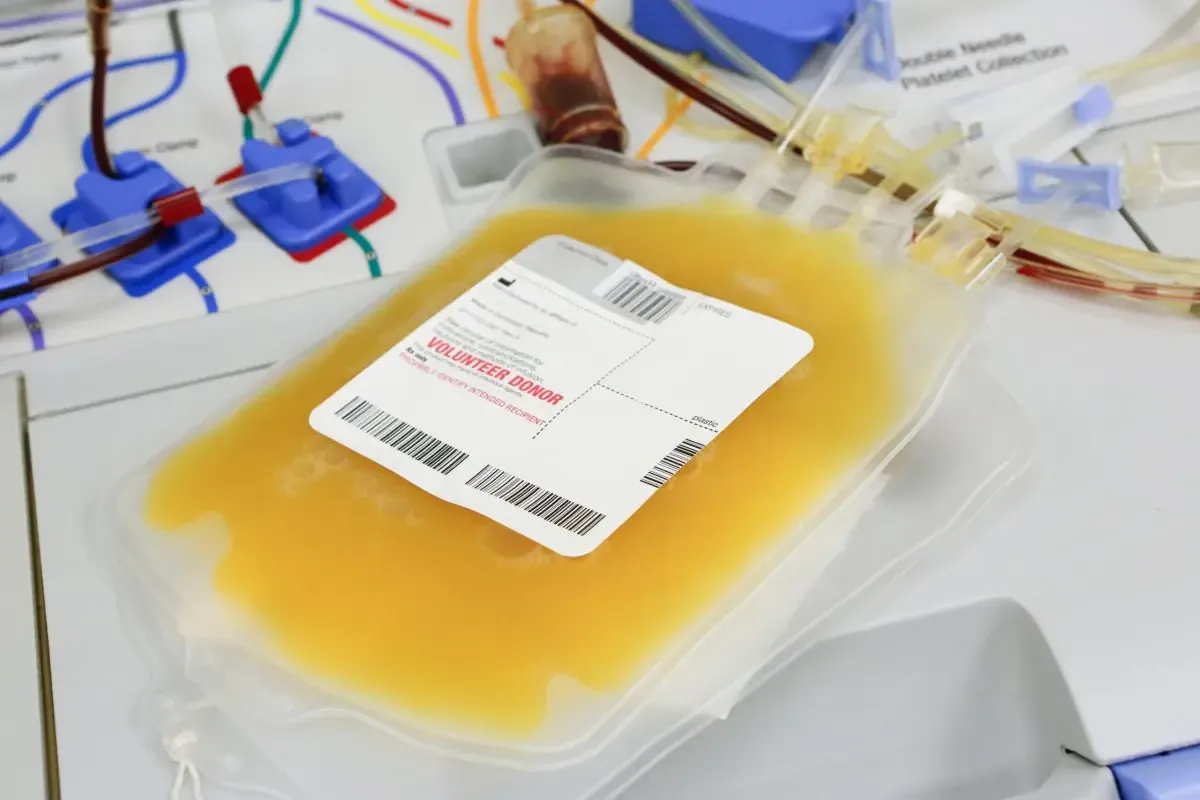
Supportive care is vital while the bone marrow heals. This might include giving growth factors to help make blood cells. In severe cases, patients might need to stay in the hospital to avoid infections.
Immunosuppressive Therapy and Hematopoietic Stem Cell Transplantation
For severe cases, we might use immunosuppressive therapy (IST) or hematopoietic stem cell transplantation (HSCT). IST uses drugs to calm the immune system, helping the bone marrow recover. A study found IST can improve outcomes for severe aplastic anemia patients.
HSCT is an option for those with severe disease and a donor. It replaces the patient’s bone marrow with healthy donor cells. While it can cure, it carries risks like graft-versus-host disease and infections.
We offer full support to international patients with medication-induced aplastic anemia. Our team aims to provide top-notch healthcare and help access treatments like IST and HSCT.
In summary, treating medication-induced aplastic anemia needs a careful look at the patient’s situation. We then tailor a treatment plan. By avoiding the drug and using advanced treatments, we can help patients get better and receive full care.
Conclusion
Patients who don’t worry about the risks of certain medicines might face serious side effects. Aplastic anemia is one of them. It’s key for doctors to teach patients about the signs and symptoms of this condition.
An uninterested or unresponsive attitude can delay diagnosis and treatment. This makes the condition worse. We aim to give top-notch healthcare to international patients, ensuring they get the care they need quickly and well.
Aplastic anemia is a serious issue that needs fast action. Knowing the causes, how it works, and how to treat it helps doctors make better choices. This approach helps avoid a lack of interest that can harm patient outcomes.
We’re dedicated to supporting patients emotionally and guiding them. Our aim is to give patients the knowledge and tools they need to manage their health well.
FAQ
What is aplastic anemia, and how does it occur?
Aplastic anemia is a serious condition where the bone marrow fails to make blood cells. This leads to a lack of all blood cell types. It can happen due to many medications, like NSAIDs and antibiotics.
What are the symptoms of aplastic anemia, and why is early diagnosis challenging?
Symptoms of aplastic anemia are often mild and easy to miss. This makes it hard to catch early. People might feel tired, get sick easily, or bleed a lot.
How do NSAIDs cause aplastic anemia?
Some NSAIDs, like indomethacin, can increase the risk of aplastic anemia. It’s not clear how, but it might harm the cells that make blood.
What is the role of antithyroid medications in causing aplastic anemia?
Medications for thyroid issues, like methimazole, can lead to aplastic anemia. Methimazole is the main culprit, and propylthiouracil is also risky, more for women.
Can anticonvulsant medications cause aplastic anemia?
Yes, some anticonvulsants, like carbamazepine, can harm the bone marrow. This can lead to aplastic anemia. Certain factors can make this risk higher.
How do antipsychotic medications contribute to bone marrow failure?
Some antipsychotics, like chlorpromazine, can cause bone marrow failure. This is a serious side effect. It’s important to watch patients closely on these drugs.
What is the significance of sulfonamides in causing aplastic anemia?
Sulfonamides, a type of antibiotic, can cause aplastic anemia. They do this by attacking the bone marrow in an immune response.
Can antirheumatic drugs cause hematologic risks, including aplastic anemia?
Yes, drugs for rheumatism, like gold salts, can harm the blood-making cells. This includes the risk of aplastic anemia. It’s important to know the risks of these drugs.
What are the risk factors that increase susceptibility to medication-induced bone marrow failure?
Some people are more at risk due to their genes, HLA type, or other factors. These can make them more likely to have problems with medication.
How is drug-induced aplastic anemia diagnosed?
Finding drug-induced aplastic anemia takes a careful approach. This includes lab tests, watching patients closely, and looking at the bone marrow. It’s also important to rule out other conditions.
What are the treatment strategies for medication-induced aplastic anemia?
Treatment starts with stopping the drug and managing symptoms. In severe cases, stronger treatments like stem cell transplants may be needed.
How can patients with a history of aplastic anemia be managed to prevent recurrence?
Patients who have had aplastic anemia need close monitoring. Their medications should be carefully chosen to avoid problems. It’s key to avoid drugs known to cause aplastic anemia.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9911543/