
Is it possible to go into remission with aplastic anemia? Discover the breakthrough treatments helping patients recover their health today.
Receiving a diagnosis of aplastic anemia can be overwhelming and frightening. But, it’s important to know that remission is possible with today’s treatments. Studies show that immunosuppressive therapy (IST) works well, with about 65-66% of patients responding positively. In some cases, 11-20% of patients even achieve complete remission, as found in a study on .
At livhospital.com, we’re dedicated to top-notch healthcare for international patients. We aim to offer advanced medical treatments and support. Our goal is to help patients on their path to remission.
Key Takeaways
- Immunosuppressive therapy (IST) is effective in achieving remission in aplastic anemia patients.
- Overall response rates to IST are around 65-66%.
- Complete remissions are reported in 11-20% of patients.
- Modern therapies have significantly improved patient outcomes.
- Comprehensive support services are crucial for patient care.
Understanding Aplastic Anemia: A Comprehensive Overview
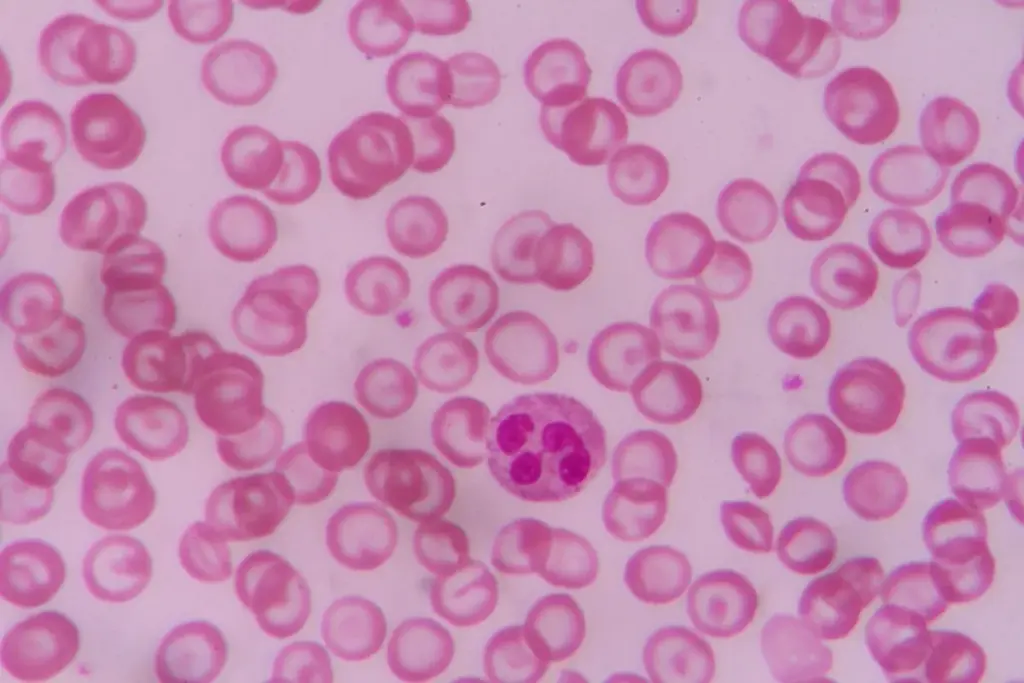
Aplastic anemia is when the bone marrow can’t make enough blood cells. This leads to health problems. It’s a complex condition with many causes.
Definition and Pathophysiology
Aplastic anemia means the bone marrow can’t make blood cells. This causes a lack of red and white blood cells and platelets. The pathophysiology is linked to the immune system attacking the bone marrow.
Many things can cause aplastic anemia. These include idiopathic causes, drug side effects, and infections. A study in says knowing the causes is key to finding treatments.
Causes and Risk Factors
Many things can lead to aplastic anemia. These include toxins, certain drugs, viruses, and autoimmune diseases. Risk factors include genetics, chemical exposure, and past treatments like chemotherapy.
- Exposure to toxins or chemicals
- Certain medications
- Viral infections
- Autoimmune disorders
- Genetic predisposition
Signs and Symptoms
The symptoms of aplastic anemia vary. They include tiredness, weakness, infections, and easy bruising. As it gets worse, symptoms like shortness of breath and dizziness can happen.
Knowing about aplastic anemia helps patients understand their condition. Recognizing causes, risk factors, and symptoms helps them make better health choices.
Defining Remission in Aplastic Anemia
Remission in aplastic anemia is a key goal of treatment. It shows how well the treatment is working. Achieving remission is complex, depending on the disease’s severity, the patient’s health, and the treatment used.
We will look at the different types of remission in aplastic anemia. This includes complete and partial remission, how to measure them, and what success in treatment means.
Complete vs. Partial Remission
In aplastic anemia, remission is divided into complete and partial remission. Complete remission means blood counts are normal and no transfusions are needed. Partial remission shows big improvements in blood counts but not to normal levels, and less need for transfusions.
Complete remission shows a strong treatment response, with normal blood cell counts. Partial remission means a big improvement, but some blood cell counts may still be low.
Clinical Markers of Remission
Several clinical markers help check if a patient is in remission. These include:
- Blood counts: Regular checks of neutrophil, platelet, and hemoglobin levels.
- Bone marrow biopsy: Looking at bone marrow cellularity and shape.
- Transfusion dependency: Seeing if the need for blood transfusions goes down or stops.
These markers help doctors see if treatment is working and if a patient is in remission.
Measuring Treatment Success
Measuring treatment success in aplastic anemia looks at how well remission is achieved. It checks blood counts, bone marrow function, and the patient’s overall health. Success is seen in achieving and keeping remission, either complete or partial, and improving the patient’s life quality.
We use remission rates and how long remission lasts to measure success. Knowing these helps doctors manage patient hopes and tailor treatments for the best results.
The Journey Into Remission: What Patients Can Expect
Getting into remission with aplastic anemia is tough but full of hope. It involves different treatments and care to help patients. Knowing what affects this journey can really help improve results.
Timeline for Treatment Response
How long it takes to see results varies a lot. Some see improvements in a few months, while others take longer. Remember, remission isn’t quick, and patience is key. Research shows it can take 3 to 6 months, but it can be longer for some.
Doctors watch how patients react to remission therapy closely. They use blood counts and bone marrow tests to check progress. This helps them adjust treatments to get the best results.
|
Timeframe |
Expected Response |
|---|---|
|
0-3 months |
Initial treatment phase; stabilization of blood counts |
|
3-6 months |
Noticeable improvement in blood counts; possible reduction in transfusion needs |
|
6+ months |
Potential achievement of partial or complete remission; continued monitoring |
Monitoring Blood Counts and Bone Marrow
Checking blood counts and bone marrow often is key to seeing if remission therapy is working. Doctors do blood tests to see how blood cells are doing. They also do bone marrow biopsies to check the marrow’s health.
“The regular assessment of blood counts and bone marrow function is vital in guiding treatment decisions and ensuring the best possible outcomes for patients with aplastic anemia.”
Psychological Aspects of the Treatment Journey
The mental side of treatment for aplastic anemia is very important. Patients feel many emotions, from fear to hope. Supportive care, like counseling and support groups, helps a lot.
Things that affect remission factors are not just medical treatments. A patient’s overall health and support system also play a big role. By focusing on these areas, doctors can give more complete care.
As we learn more about treating aplastic anemia, the path to remission gets easier and more hopeful. By using the right remission therapy and supportive care, we can make life better for those affected.
Immunosuppressive Therapy (IST): Primary Treatment Approach
Immunosuppressive Therapy is a main way to treat aplastic anemia. It helps the bone marrow make blood cells again. We’ll look into IST, its parts, and how it helps patients with aplastic anemia.
Anti-Thymocyte Globulin (ATG) Therapy
ATG therapy is key in IST for aplastic anemia. It removes T-cells, which harm the bone marrow. By stopping the immune system’s attack, ATG therapy boosts blood cell making. ATG is given in the hospital because of the risk of reactions.
Cyclosporine Treatment
Cyclosporine is another important drug in treating aplastic anemia. It stops T-cells from attacking the bone marrow. Studies show that cyclosporine works better with ATG therapy. It’s important to watch cyclosporine levels to avoid harm.
Combination Therapies and Protocols
Using ATG and cyclosporine together is now common in IST for aplastic anemia. This mix has a 65-66% success rate, giving patients a good chance of remission. Treatment plans can change based on how a patient responds. Researchers are looking for the best way to use IST to get better results.
Every patient with aplastic anemia is different, and treatments are made just for them. IST has changed how we manage this disease, giving patients hope for a better life.
Success Rates of Immunosuppressive Therapy
Knowing how well IST works is key for treating aplastic anemia. Immunosuppressive therapy is a mainstay in managing this condition. It’s a good option for many patients instead of bone marrow transplants.
Research shows IST works well for most patients. It gets good results in 65-66% of cases. And, 11-20% of patients see a complete recovery. These numbers show how effective IST can be.
Overall Response Rates
The success rate of IST is important. It shows how many patients see some improvement. With a success rate of 65-66%, IST proves to be a valuable treatment.
Complete Remission Statistics
Seeing a complete recovery is a big win in treating aplastic anemia. While only 11-20% of patients reach complete remission with IST, it’s a big step forward for them.
Factors Affecting Treatment Success
Several things can affect how well IST works. These include the patient’s age, how severe the disease is, and the type of immunosuppressive treatment. Knowing these can help improve treatment results.
|
Factor |
Influence on IST Success |
|---|---|
|
Patient Age |
Younger patients tend to have better outcomes |
|
Disease Severity |
Less severe disease at diagnosis correlates with higher success rates |
|
Immunosuppressive Regimen |
Combination therapies often yield better results than single-agent treatments |
By looking at these factors and knowing the success rates, doctors can make IST better fit each patient. This can lead to better treatment results.
Age-Related Differences in Remission Outcomes
Age is key in how well patients with aplastic anemia do. It affects how well they respond to treatment.
Pediatric Response Rates
Young patients do well with treatment, with a 65.7% response rate. About 11.42% even get complete remission. This shows kids can often get better from aplastic anemia.
A study found that kids do great with early treatment. This is because they start treatment sooner.
“Early intervention with immunosuppressive therapy can significantly improve outcomes in children with aplastic anemia.”
|
Age Group |
Overall Response Rate |
Complete Remission Rate |
|---|---|---|
|
Pediatric |
65.7% |
11.42% |
|
Adult |
Varies |
Varies |
|
Over 60 |
47% |
Lower than younger adults |
Adult Response Patterns
Adults react differently to treatment. Their health and how bad the disease is matter. Some get complete remission, while others don’t respond at all.
Special Considerations for Patients Over 60
People over 60 face special challenges. They have a 47% response rate. They often have other health issues and may face more risks from treatment. So, their treatment plans need to be very careful and specific.
Understanding how age affects treatment is crucial for managing aplastic anemia. This knowledge helps doctors create better treatment plans for each patient group.
Hematopoietic Stem Cell Transplantation (HSCT): The Curative Option
Hematopoietic Stem Cell Transplantation (HSCT) is a treatment that can cure aplastic anemia. It replaces damaged bone marrow with healthy stem cells. These stem cells can come from the patient or a donor. We’ll look at how HSCT works, including choosing the right candidate, matching donors, and the transplant process.
Candidate Selection Process
Choosing the right candidate for HSCT is complex. It looks at the patient’s health, how severe their aplastic anemia is, and if they’ve tried other treatments. Those with severe aplastic anemia or who didn’t do well with other treatments are often considered for HSCT.
|
Selection Criteria |
Description |
|---|---|
|
Age and Health Status |
Younger patients with fewer health problems are usually better candidates. |
|
Disease Severity |
Those with severe aplastic anemia are often chosen for HSCT. |
|
Previous Treatment Response |
Those who didn’t do well with other treatments might get HSCT. |
Donor Matching Considerations
Matching donors is key for allogenic transplants. The human leukocyte antigen (HLA) system is used to match donors and recipients. How well the HLA matches can affect the risk of graft-versus-host disease (GVHD), a serious complication.
“The success of HSCT depends a lot on how well the HLA matches between donor and recipient. Finding a good donor is very important.”
Transplantation Procedure
The HSCT process starts with conditioning, getting the bone marrow ready for new stem cells. Then, the stem cells are infused. They go to the bone marrow and start making new blood cells.
- Pre-transplant conditioning to prepare the bone marrow.
- Infusion of hematopoietic stem cells.
- Post-transplant care to manage complications and support recovery.
Understanding HSCT helps patients and doctors make informed decisions. It’s a complex but potentially life-saving treatment for aplastic anemia.
Long-Term Survival and Remission Rates with HSCT
Hematopoietic Stem Cell Transplantation (HSCT) has changed how we treat aplastic anemia. It offers hope for long-term survival and remission. It’s important to know how HSCT affects different patients.
Pediatric Outcomes
Pediatric patients do well with HSCT, with survival rates of 70% to 78%. Younger patients adapt better to treatment and have fewer health issues. HSCT improves their survival and quality of life, helping them grow up normally.
Adult Outcomes
Adults’ results with HSCT depend on their age, health, and other conditions. While many do well, choosing the right patient and donor is key. Adults need a detailed check-up before transplant to reduce risks and improve chances of survival and remission.
Advances in Transplantation Protocols
New HSCT methods have boosted patient results. Better donor matching, more effective treatments, and improved care after transplant are some of these advances. Personalized treatment plans, based on each patient’s genetics and history, are also becoming more common. These changes aim to improve survival and remission rates even more.
We keep working to make HSCT better for our patients. By understanding how HSCT works, we can support patients and their families better. This complex journey is easier with our help.
Life-Threatening Complications and Management
Managing aplastic anemia is more than just treating the condition. It also means dealing with serious complications that can be life-threatening. These complications can greatly affect a patient’s quality of life and chances of survival.
Infection Risks and Prevention
Patients with aplastic anemia face a high risk of infections. Their weakened immune systems make them more likely to get sick from bacteria, viruses, and fungi. To prevent infections, we use antibiotics, avoid exposure to germs, and sometimes isolate patients.
We also stress the importance of getting vaccinated against common diseases. However, we avoid live vaccines because they can cause problems.
Bleeding Complications
Bleeding is another big worry for those with aplastic anemia. The condition can cause a low platelet count, which increases bleeding risks. To manage this, we advise avoiding injuries, use platelet transfusions when needed, and give medicines to help platelets grow.
For severe bleeding, quick medical help is needed to keep the patient safe and prevent further issues.
Organ Damage and Supportive Care
Aplastic anemia can also harm organs, either directly or as a side effect of treatment. Supportive care is key in handling these problems. It includes watching for organ damage signs and finding ways to reduce harm.
Supportive care includes blood transfusions to manage anemia and low platelets. It also includes medicines to help organs work better. Sometimes, patients need to stay in the hospital to manage severe issues.
|
Complication |
Management Strategies |
Preventive Measures |
|---|---|---|
|
Infections |
Prophylactic antibiotics, antifungal medications |
Vaccinations, isolation, hygiene practices |
|
Bleeding |
Platelet transfusions, medications to promote platelet production |
Avoiding trauma, monitoring platelet count |
|
Organ Damage |
Supportive care, monitoring for organ dysfunction |
Regular check-ups, adjusting treatment plans as necessary |
By knowing the risks of aplastic anemia and using effective management strategies, we can improve patient outcomes. This helps reduce the risk of serious complications.
Risk of Relapse After Achieving Remission
Getting to remission is a big win for those with aplastic anemia. But, the fight doesn’t stop there. The chance of relapse is still there, and knowing how to handle it is key for staying healthy long-term.
Monitoring for Early Signs of Recurrence
Keeping an eye on things is crucial to spot relapse early. This means regular blood tests and bone marrow biopsies. Early detection lets doctors act fast to stop a full relapse.
Key Monitoring Parameters:
- Blood cell counts
- Bone marrow cellularity
- Presence of abnormal cells
We suggest patients team up with their doctors to set up a monitoring plan that fits their needs.
Treatment Options for Relapsed Disease
If relapse happens, there are ways to manage it again. Options include starting immunosuppressive therapy again or looking into other treatments like stem cell transplants.
|
Treatment Option |
Description |
Considerations |
|---|---|---|
|
Immunosuppressive Therapy |
Using medications to suppress the immune system and support bone marrow function. |
Response rates vary; may require combination therapy. |
|
Hematopoietic Stem Cell Transplantation |
A potentially curative option involving replacing the patient’s bone marrow with healthy stem cells. |
Requires a suitable donor; carries risks of graft-versus-host disease. |
Long-term Follow-up Protocols
For those in remission, ongoing care is vital. This means regular check-ups, constant monitoring, and adjusting treatments as needed. It’s all about keeping the best outcomes in sight.
Long-term follow-up care includes:
- Regular blood tests
- Periodic bone marrow assessments
- Disease management planning
By staying alert and teaming up with healthcare, patients can lower the risk of relapse. This way, they can live a better life.
Emerging Therapies and Research Directions
New treatments are changing how we manage aplastic anemia, leading to better results for patients. Research is moving towards more precise and effective treatments.
Novel Immunosuppressive Approaches
New ways to suppress the immune system are being studied. Eltrombopag, a drug that helps blood cells, is showing great promise. It’s used with other treatments to improve outcomes.
Researchers are also looking into checkpoint inhibitors. These could help the immune system stop attacking bone marrow cells. This could lead to better recovery.
Gene Therapy Prospects
Gene therapy is a new, exciting field. It aims to fix the genetic problems that cause aplastic anemia. By fixing or replacing bad genes, it could offer a cure.
Early tests have shown gene therapy is safe and works. Now, scientists are working to make it even better. They’re looking at new ways to deliver the therapy.
Clinical Trials and Experimental Treatments
Clinical trials are key in finding new treatments for aplastic anemia. They’re testing new drugs, gene editing, and cell therapies.
Joining a clinical trial can give patients access to new treatments. It also helps doctors learn more about the disease. This knowledge will help improve care for aplastic anemia in the future.
Lifestyle Factors That Support Remission
Medical treatment is key, but lifestyle also plays a big role in helping aplastic anemia patients get better. The right habits can make treatment work better and make you feel better overall.
Nutrition and Diet
Eating well is very important for those fighting aplastic anemia. Nutritional support helps deal with side effects and helps the bone marrow heal. Foods high in iron, vitamin B12, and folate are especially good because they help make blood cells.
It’s best to eat a variety of foods like lean proteins, whole grains, and lots of fruits and veggies. Drinking lots of water is also key. Try to avoid raw or undercooked foods to lower the chance of getting sick.
Physical Activity Guidelines
Doing gentle physical activity can boost your health and cut down on tiredness. Walking, yoga, or swimming are good choices because they’re easy on the body and can be adjusted to fit your energy level.
Always talk to your doctor before starting any new exercise. They can make sure it’s safe for you.
Infection Prevention Strategies
Infection prevention is very important for aplastic anemia patients, especially when they’re getting treatment. Simple steps like washing your hands a lot, staying away from sick people, and getting all your shots can really help prevent infections.
Also, know the signs of infection like fever, chills, or a long cough. If you notice these, get help right away.
Specialized Care Centers and Treatment Access
Specialized care centers are key in treating aplastic anemia. They have the latest tech and teams with lots of experience. This makes them perfect for complex cases.
Expert Medical Teams
Finding the right medical team is crucial. Hematologists and oncologists work together to create treatment plans for each patient. Access to a multidisciplinary team is a hallmark of specialized care centers.
When looking for a specialized care center, consider these factors:
- Experience of the medical team in treating aplastic anemia
- Availability of advanced treatment options, including immunosuppressive therapy and hematopoietic stem cell transplantation
- Comprehensive support services, including counseling and nutritional guidance
Insurance and Financial Considerations
Dealing with insurance and money can be tough. Many care centers have staff to help with these issues. It’s essential to discuss these aspects with your healthcare provider to avoid unexpected costs.
|
Insurance Factor |
Description |
Consideration |
|---|---|---|
|
Coverage |
Check if your insurance covers treatments for aplastic anemia |
Review policy details carefully |
|
Pre-authorization |
Understand pre-authorization requirements for treatments |
Work with your healthcare provider to facilitate pre-authorization |
|
Out-of-pocket costs |
Calculate potential out-of-pocket expenses |
Explore financial assistance programs |
International Treatment Options
For those looking for other treatment options, international centers offer cutting-edge therapies and clinical trials. It’s crucial to research the credentials of these centers and understand any extra logistical needs.
When thinking about international treatment, consider these factors:
- Accreditation and reputation of the treatment center
- Language and cultural considerations
- Travel and accommodation arrangements
Conclusion: The Future of Aplastic Anemia Treatment and Remission
Recent advances in treatments have greatly helped patients with aplastic anemia. We’ve looked at how to diagnose and treat this condition. We also talked about the need for full care.
The SOAR trial showed that a combination of treatments can work well. It found that 46% of patients had a good response after 6 months. This shows promise for new treatments.
New research brings hope for the future. Scientists are looking into new treatments like HPAG. It might be safer and less likely to cause blood clots. For more on this, check out .
The outlook for treating aplastic anemia is bright. With ongoing research, we can expect even better results. Healthcare providers can give the best care by staying up-to-date on treatments.
FAQ
What is aplastic anemia, and how is it defined?
Aplastic anemia is when the bone marrow can’t make enough blood cells. It’s a rare disease that can be very serious if not treated.
What are the causes and risk factors of aplastic anemia?
The exact causes of aplastic anemia are not always known. It can be caused by chemicals, radiation, or viruses. Some cases are linked to genetic disorders or autoimmune diseases.
What is remission in aplastic anemia, and how is it achieved?
Remission means the disease is controlled, and the bone marrow is making enough blood cells. It can be achieved through treatments like immunosuppressive therapy and stem cell transplantation.
What is the difference between complete and partial remission in aplastic anemia?
Complete remission means blood counts and bone marrow function are normal. Partial remission means there’s a big improvement in blood counts, but not to normal levels.
How is treatment success measured in aplastic anemia?
Success is measured by checking blood counts, bone marrow function, and overall health. Regular check-ups with a healthcare provider are key to see how treatment is working.
What is immunosuppressive therapy, and how does it work in treating aplastic anemia?
Immunosuppressive therapy aims to stop the immune system from attacking the bone marrow. It uses medicines like anti-thymocyte globulin and cyclosporine.
What are the success rates of immunosuppressive therapy in treating aplastic anemia?
About 65-66% of patients respond to immunosuppressive therapy. Complete remission rates are 11-20%. Success can depend on age, disease severity, and treatment.
How does age impact remission outcomes in aplastic anemia?
Age is a big factor in remission outcomes. Kids tend to do better than adults. Older adults may have lower success rates due to other health issues and bone marrow function.
What is hematopoietic stem cell transplantation, and how does it work in treating aplastic anemia?
Hematopoietic stem cell transplantation is a treatment that replaces the bone marrow with healthy stem cells from a donor. It’s a complex process that needs careful planning and matching.
What are the long-term survival and remission rates with hematopoietic stem cell transplantation?
Survival rates after stem cell transplantation vary. They depend on age and disease severity. Kids tend to have better survival rates, ranging from 70-78%.
How can patients prevent and manage life-threatening complications associated with aplastic anemia?
Patients can prevent and manage complications by following infection prevention strategies, getting regular blood transfusions, and monitoring blood counts and bone marrow function.
What lifestyle factors can support remission in aplastic anemia?
Eating a healthy diet, staying active, and following infection prevention strategies can help support remission in aplastic anemia.
How can patients access specialized care centers and treatment options for aplastic anemia?
Patients can find specialized care centers through referrals from their primary care physician or hematologist. It’s important to consider insurance and financial options to find the best treatment.
What are the emerging therapies and research directions for aplastic anemia?
New therapies include novel immunosuppressive approaches, gene therapy, and clinical trials. Research is ongoing to improve treatment outcomes and find new strategies.
What is the definition of remission therapy in the context of aplastic anemia?
Remission therapy refers to treatments used to achieve and maintain remission in aplastic anemia. This includes immunosuppressive therapy and stem cell transplantation.
How do remission rates vary among different patient populations?
Remission rates vary among different patient groups. This depends on factors like age, disease severity, and treatment protocol.
What are the criteria used to determine treatment success and remission in aplastic anemia?
Treatment success and remission are determined by monitoring blood counts, bone marrow function, and overall health. Established clinical criteria and guidelines are used.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26524459/










