
An allogeneic transfusion is when blood or blood components from a donor are given to a patient. This is a key treatment for those with severe blood loss, anemia, or other needs for blood replacement. Allogeneic blood transfusion involves donor blood. Explore this best vital guide to understand the risks and successful outcomes today.
At livhospital.com, we focus on giving top-notch care to international patients. We make sure they get the best medical treatment. Unlike autologous transfusions, where a patient’s own blood is used, allogeneic transfusions use donor blood. It’s important to match the donor’s blood type with the patient’s to avoid bad reactions.
Key Takeaways
- Allogeneic transfusion involves transferring blood or blood components from a compatible donor.
- This procedure is vital for treating severe anemia, surgical blood loss, and other conditions.
- Careful matching of the donor’s blood type is necessary to minimize risks.
- livhospital.com provides comprehensive care and support for international patients.
- Autologous transfusion uses a patient’s own blood, differing from allogeneic transfusion.
Understanding Allogeneic Blood Transfusion
Allogeneic blood transfusion is a lifesaving treatment that needs careful thought about who gives and who gets the blood. We will look at the key ideas behind this medical action.
Definition and Basic Concepts
Allogeneic blood transfusion means giving blood or blood parts from one person to another. It’s very important in surgeries and when someone is hurt badly. For more info, check out NHS guidelines on blood transfusion.
The success of this transfusion depends on the blood types matching between the giver and the receiver. It’s very important to make sure they match to avoid bad reactions. These reactions can be mild or very serious.
We will get into the details of blood matching and typing later. But for now, it’s key to know that allogeneic blood transfusion is a complex task. The careful screening of donors and the thorough testing of blood are crucial steps. They help make sure the transfusion is safe and works well.
By understanding the basics of allogeneic blood transfusion, doctors can handle the risks better. This leads to better care for patients.
Allogeneic vs. Autologous Transfusions: Key Differences

Allogeneic and autologous transfusions are two different ways to give blood. Each has its own good points and downsides. Knowing these differences helps make better choices for blood transfusions.
Understanding Autologous Transfusion
Autologous transfusion uses a patient’s own blood. This blood is collected and saved before surgery. It avoids blood type problems and lowers the chance of bad reactions.
This process starts weeks before surgery. It’s great for surgeries where a lot of blood loss is expected. This way, the patient’s blood is ready when needed.
Comparative Advantages and Limitations
Allogeneic and autologous transfusions have some key differences. Here’s a table that shows the main good and bad points of each:
|
Characteristics |
Allogeneic Transfusion |
Autologous Transfusion |
|---|---|---|
|
Source of Blood |
Donated blood from others |
Patient’s own blood |
|
Risk of Transfusion Reactions |
Higher risk due to potential incompatibility |
Lower risk as it uses the patient’s own blood |
|
Availability |
Generally available through blood banks |
Limited by the amount of blood that can be collected and stored |
|
Cost |
Variable, depending on blood bank costs |
May be more expensive due to collection and storage procedures |
|
Immunosuppression Risk |
Associated with a higher risk of immunosuppression |
Lower risk of immunosuppression |
Autologous transfusion has big advantages like less risk of bad reactions and less chance of weakening the immune system. But, it’s not always possible or available. It also has limits like how much blood can be saved.
In conclusion, choosing between allogeneic and autologous transfusions depends on many things. These include the patient’s health, the surgery type, and if autologous blood is available. Knowing the differences helps doctors make the best choices for their patients.
The Process of Allogeneic Blood Donation
At the heart of transfusion medicine is the allogeneic blood donation process. It involves careful donor selection, blood collection, and processing. We follow strict protocols to ensure the blood is safe and of high quality, from the start to the end.
Donor Eligibility Criteria
Donor eligibility is the first step in the allogeneic blood donation process. Potential donors are checked for their medical history, infectious disease status, and health. Eligible donors must be in good health, meet specific age and weight criteria, and pass a thorough medical examination.
The criteria are in place to protect both the donor and the recipient. For example, donors are tested for infectious diseases like HIV, hepatitis, and malaria. This rigorous screening process ensures the safety of the blood supply.
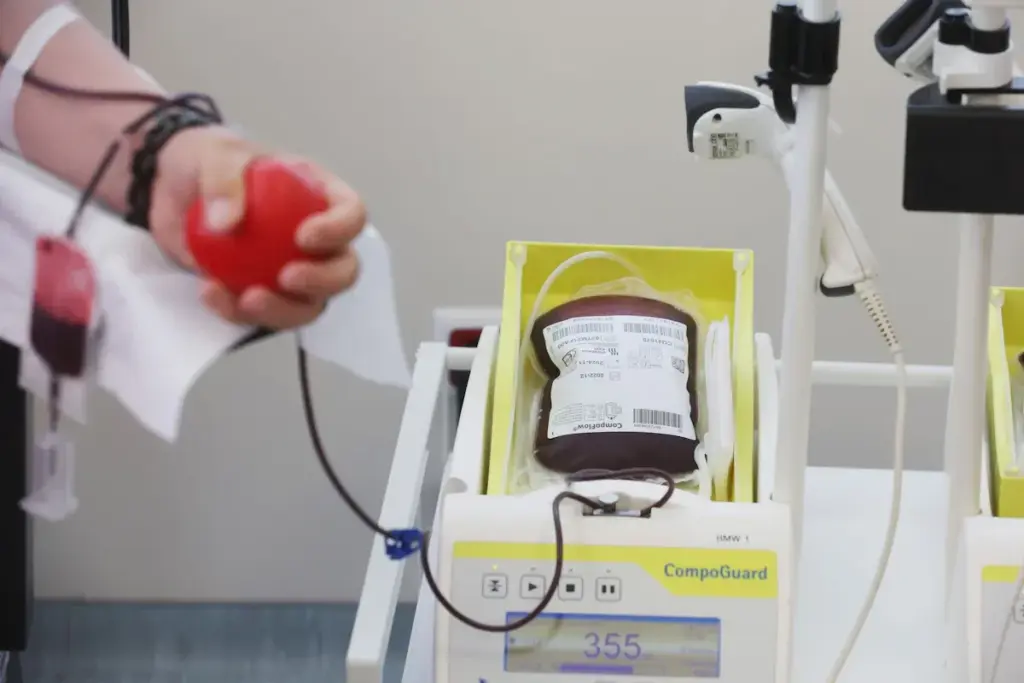
Collection and Processing Procedures
Once a donor is deemed eligible, the blood collection process starts. Blood is collected into sterile bags with anticoagulants to prevent clotting. We follow strict protocols to label and track donated blood, ensuring it is processed correctly and safely.
After collection, the blood is processed. This includes testing for infectious diseases and typing for compatibility. The blood is then separated into its components, such as red blood cells, plasma, and platelets. These components can treat different medical conditions.
|
Blood Component |
Primary Use |
|---|---|
|
Red Blood Cells |
Treatment of anemia, blood loss during surgery or trauma |
|
Plasma |
Management of clotting disorders, burn patients |
|
Platelets |
Prevention and treatment of bleeding in patients with low platelet count |
“The gift of blood donation is a lifesaving act that requires careful consideration and rigorous safety protocols. At our institution, we are committed to upholding the highest standards in transfusion medicine.”
— Medical Director
In conclusion, the allogeneic blood donation process is complex. It involves careful donor selection, meticulous blood collection, and thorough processing. We are dedicated to ensuring every step is carried out with care and attention to detail. This contributes to the safety and efficacy of blood transfusions.
Blood Compatibility and Typing
Allogeneic blood transfusion needs accurate blood typing and testing. It’s key to match the donor’s and recipient’s blood types to avoid bad reactions. Our team follows strict rules to keep patients safe during transfusions.
“The cornerstone of safe blood transfusion is compatibility,” say doctors everywhere. Making sure blood types match is not just a step; it’s a safety must that affects patient results.
ABO and Rh Blood Group Systems
The ABO and Rh systems are key in blood matching. The ABO system sorts blood into A, B, AB, and O types based on red blood cell antigens. The Rh system splits blood into Rh-positive or Rh-negative types, based on the RhD antigen.
Knowing these systems is crucial for blood transfusions. For example, someone with Type A blood has antibodies against Type B. Mixing incompatible blood can cause serious reactions. Our team makes sure ABO and Rh types match to lower reaction risks.
- ABO Blood Types: A, B, AB, O
- Rh Blood Types: Rh-positive, Rh-negative
Cross-Matching and Compatibility Testing
Cross-matching is a test to check if donor and recipient blood match. It mixes the recipient’s serum with the donor’s red blood cells to look for bad reactions.
Testing for compatibility involves several steps:
- Find the ABO and Rh types of both donor and recipient.
- Check the recipient’s serum for antibodies against blood group antigens.
- Do a cross-match test to confirm it’s safe.
By doing these steps, we lower the chance of bad reactions and make sure patients get the right blood. As doctors, we promise to give the right blood to the right patient at the right time. It’s not just a saying; it’s our promise to keep patients safe.
In summary, blood typing and compatibility are key for safe blood transfusions. By understanding ABO and Rh systems and doing detailed tests, we can reduce risks and give top-notch care to our patients.
Clinical Indications for Allogeneic Transfusions
In today’s healthcare, allogeneic blood transfusions are key for treating patients. They are needed for those undergoing major surgery, experiencing trauma, or dealing with chronic medical conditions. These transfusions help replace blood lost during surgery or injury, aiding in recovery and survival.
Allogeneic blood transfusions play a vital role in managing different health issues. They help restore blood volume, improve oxygen delivery, and support patient recovery.
Surgical Interventions
During surgeries, allogeneic transfusions manage significant blood loss. Common surgeries needing these transfusions include:
- Cardiovascular surgery
- Orthopedic surgery
- Neurosurgery
- Organ transplantation
These surgeries often lead to a lot of blood loss. Transfusion therapy is crucial for patient care.
Trauma and Emergency Medicine
In trauma cases, allogeneic transfusions are essential. They quickly restore blood volume and ensure vital organs get enough oxygen. Trauma patients often need massive transfusion protocols, involving large amounts of blood products.
Chronic Medical Conditions
Certain chronic conditions, like anemia from chronic disease or bone marrow failure, may require allogeneic transfusions. Patients with these conditions often need regular transfusions to manage symptoms and improve their life quality.
Global Statistics and Prevalence
The need for allogeneic blood transfusions is growing worldwide. This creates challenges in meeting supply and demand. It’s important to understand the global statistics and prevalence of these transfusions.
Transfusion Rates Across Different Countries
Allogeneic blood transfusion rates differ greatly from country to country. This is due to various factors like healthcare infrastructure and the prevalence of certain diseases. For example, countries with older populations often see higher transfusion rates due to more surgeries and age-related diseases.
The World Health Organization (WHO) notes that blood transfusion availability and use vary widely. Developed countries have more established blood banking systems, leading to higher transfusion rates. In contrast, some developing countries struggle to maintain a stable blood supply, resulting in lower rates.
|
Country |
Transfusion Rate (per 1,000 population) |
|---|---|
|
United States |
75.4 |
|
Canada |
67.2 |
|
Australia |
58.1 |
|
United Kingdom |
54.9 |
Supply and Demand Challenges
One major challenge in transfusion medicine is balancing blood supply and demand. Demand is driven by surgeries, trauma cases, and managing certain medical conditions. Ensuring a safe and sufficient blood supply requires effective blood bank management and donor recruitment.
“The key to meeting the demand for blood transfusions lies in maintaining a robust blood banking system that can ensure a steady supply of safe blood.”
— Transfusion Medicine Specialist
To tackle these challenges, healthcare organizations are using various strategies. These include improving donor recruitment, enhancing blood collection, and optimizing inventory management. By implementing these measures, we can ensure the global demand for allogeneic blood transfusions is met effectively.
Safety Measures in Modern Transfusion Medicine
Transfusion medicine has become much safer. It uses strict screening for diseases and quality control. These steps help lower the risk of infections and ensure blood quality.
Screening Protocols for Infectious Diseases
Checking blood donations for diseases is crucial. We use the latest technology to find viruses like HIV and hepatitis. We also look for bacteria in the blood.
Key screening measures include:
- Nucleic acid testing (NAT) for viral detection
- Serological testing for antibodies against specific pathogens
- Bacterial contamination testing for platelet components
Quality Control Standards
Quality control is key to safe blood products. We follow strict rules from donation to transfusion.
Key aspects of quality control include:
- Donor selection and screening
- Blood component preparation and storage
- Labeling and tracking of blood products
|
Quality Control Measure |
Description |
Benefit |
|---|---|---|
|
Donor Screening |
Rigorous assessment of donor eligibility |
Reduces risk of transfusion-transmitted infections |
|
Blood Component Testing |
Advanced testing for pathogens and compatibility |
Ensures safety and compatibility of blood products |
|
Storage and Handling |
Controlled environment for blood product storage |
Maintains integrity and viability of blood components |
These safety steps make blood transfusions safer. They protect patients from infections and improve care quality.
Risks Associated with Allogeneic Transfusions
It’s important to know the risks of allogeneic transfusions for better patient care. These blood transfusions are key in medical treatment but come with risks.
Immediate Transfusion Reactions
Immediate reactions happen within minutes to hours after transfusion. They can be mild or severe, causing fever, chills, and in bad cases, anaphylaxis or hemolysis. We watch patients closely to spot and handle any bad reactions fast.
Common immediate transfusion reactions include:
- Febrile non-hemolytic transfusion reactions (FNHTR)
- Allergic reactions
- Acute hemolytic transfusion reactions (AHTR)
Delayed Complications
Delayed problems can show up days to years later. These include infections from transfusions, iron overload, and graft-versus-host disease (GVHD). Though rare, these issues can really affect a patient’s health.
|
Complication |
Description |
Prevention/ Management |
|---|---|---|
|
Transfusion-transmitted infections |
Infections passed through transfused blood, like HIV or hepatitis. |
Strict donor screening and blood testing. |
|
Iron overload |
Too much iron from frequent transfusions, which can harm organs. |
Checking iron levels and using chelation therapy. |
|
Graft-versus-host disease (GVHD) |
Donor immune cells attacking the recipient’s tissues. |
Using irradiated blood products to stop donor lymphocytes. |
Transfusion-Related Acute Lung Injury (TRALI)
TRALI is a serious issue causing non-cardiogenic pulmonary edema. It’s linked to plasma-containing blood products. We follow strict protocols to lower TRALI risk, like using male-dominant plasma to avoid HLA antibodies.
“TRALI is a leading cause of transfusion-related mortality, emphasizing the need for vigilant monitoring and preventive strategies.”
— Source: Clinical Transfusion Medicine
By knowing these risks and taking safety steps, we aim to give safe and effective transfusions to our patients.
Immunological Considerations
It’s key to understand how allogeneic transfusions affect the immune system. These transfusions can change a patient’s immune response, impacting their health in the short and long term. We work hard to manage these effects to help our patients get the best care.
Transfusion-Related Immunomodulation
Transfusion-related immunomodulation (TRIM) happens when blood from another person changes how the immune system works. This can make patients more likely to get infections. It might also affect how well surgeries or cancer treatments work. TRIM involves many complex processes and can be influenced by how much blood is given and the patient’s immune health.
Impact on Recipient’s Immune System
Allogeneic transfusions really affect a patient’s immune system. They can either boost or weaken the immune response, making it harder to fight off infections or deal with other immune challenges. We keep a close eye on patients who have had these transfusions to handle any immune problems that might arise.
Infection Risk Comparison: Allogeneic vs. Autologous
It’s important to know the differences in infection risk between allogeneic and autologous transfusions. We look at the stats on postoperative infections and how to prevent them. This gives us a full picture.
Statistical Analysis of Postoperative Infections
Research shows that allogeneic and autologous blood transfusions have different infection risks. Allogeneic transfusions, which come from another person, carry a higher risk of infections. This is because they can introduce foreign antigens and affect the immune system.
Autologous transfusions, where patients get their own blood, might lower the risk of infections. This is because the body is less likely to react against its own blood. We’ve gathered data from various studies to show this difference.
|
Transfusion Type |
Infection Rate (%) |
Relative Risk |
|---|---|---|
|
Allogeneic |
12.5 |
1.8 |
|
Autologous |
6.2 |
0.7 |
Preventive Strategies
To lower the risk of infections after surgery, we use several strategies. These include:
- Strict donor screening for allogeneic blood
- Use of autologous blood transfusions when feasible
- Implementation of robust infection control protocols
- Monitoring patients for early signs of infection
By using these strategies, we can greatly reduce the risk of infections in patients who need blood transfusions. Our focus on evidence-based care means our patients get the best treatment.
Healthcare Network Protocols and Standards
Healthcare networks play a key role in setting rules for transfusion medicine. A strong framework is essential for safe and efficient blood product delivery. We work together, combining the skills of hematologists, transfusion specialists, and other healthcare experts. This teamwork helps us create and follow detailed protocols.
Multidisciplinary Approach to Transfusion Medicine
Working together is vital in transfusion medicine. It helps us share knowledge and ideas across different healthcare fields. This teamwork allows us to:
- Make protocols based on the latest research in transfusion medicine.
- Make sure everyone follows the best practices, keeping patients safe and well cared for.
- Keep healthcare professionals updated with the newest information.
By combining different skills, we tackle the tough challenges in transfusion medicine. This leads to better care for our patients.
Quality Assurance and Ethical Considerations
Quality is at the core of our transfusion medicine work. We follow strict quality control steps, including:
- Regular checks to make sure we follow the rules.
- Watching how transfusions go to find ways to get better.
- Putting ethical rules first, like getting consent and keeping patient info private.
We are fully committed to quality and ethics. This shows our dedication to top-notch healthcare. We think a team effort and strict quality checks help us keep transfusion medicine at its best.
Key parts of our quality work include:
- Screening protocols to cut down on risks from infectious diseases.
- Quality control standards for blood collection, processing, and storage.
- Ethical guidelines that always put patient safety and well-being first.
By sticking to these standards, we make sure our transfusion medicine is safe, effective, and respects patient rights.
Future Developments in Transfusion Medicine
Looking ahead, transfusion medicine will evolve with new technologies and research. The field is always changing, thanks to tech advances and innovation. At livhospital.com, we’re committed to leading these changes, ensuring our patients get the best in transfusion medicine.
Emerging Technologies and Techniques
New technologies are set to change transfusion medicine. Artificial intelligence (AI) and machine learning (ML) could improve blood selection and transfusion results. They can analyze lots of data to tailor transfusions to each patient.
Synthetic blood substitutes are also being developed. These could replace some blood transfusions, making them safer and more available. Though still experimental, they show great promise.
- New blood typing and cross-matching methods aim to lower transfusion reaction risks.
- Pathogen reduction technologies are being used to make blood safer.
- Researchers are exploring new ways to store blood longer.
Research Directions and Innovations
Transfusion medicine research covers many areas. One key focus is transfusion-related immunomodulation and its effects on patients. Studying how transfusions affect the immune system can lead to better care.
Another important area is personalized transfusion medicine. Tailoring transfusions to each patient can improve outcomes and reduce risks. This involves considering genetic factors, medical history, and current health.
Studies are also looking at transfusion medicine in different situations. This includes surgeries, trauma care, and managing chronic conditions. The goal is to refine guidelines and enhance patient care.
Conclusion
Allogeneic blood transfusions are key in today’s healthcare. They need careful thought about matching, safety, and patient care. At livhospital.com, we aim to offer top-notch healthcare. We focus especially on transfusion medicine.
Looking after patients who get allogeneic blood transfusions is a team effort. We follow strict quality and ethics standards. We make sure our international patients get the best treatment for their health issues.
Our main goal is quality, safety, and care that puts patients first. We use the newest in allogeneic blood transfusion and keep safety rules tight. This way, we aim to give our patients care that meets their unique needs.
FAQ
What does allogeneic mean in the context of blood transfusion?
Allogeneic blood comes from one person and is given to another. This is different from using a patient’s own blood, known as autologous transfusions.
What is the difference between allogeneic and autologous blood transfusions?
Allogeneic blood comes from someone else, while autologous blood is from the patient. Allogeneic blood can cause reactions and weaken the immune system. Autologous blood avoids blood type problems.
How is blood compatibility determined for allogeneic transfusions?
Blood types are checked to match the donor and recipient. This includes the ABO and Rh systems. Tests ensure the blood is safe for the recipient.
What are the risks associated with allogeneic blood transfusions?
Risks include immediate reactions and long-term problems. There’s also a chance of lung injury. The blood can affect the recipient’s immune system.
How is the safety of allogeneic blood transfusions ensured?
Safety comes from strict screening and quality control. Our team follows international standards. This reduces risks for patients.
What are the clinical indications for allogeneic blood transfusions?
They’re used in surgeries, trauma, and chronic conditions. They replace lost blood and help patients recover.
How does allogeneic blood donation work?
Donors are first screened. Then, blood is collected and tested. It’s typed for compatibility to ensure safety.
What is the impact of allogeneic transfusions on the recipient’s immune system?
These transfusions can change how the immune system works. It’s important to understand this for patient care.
Are there any alternatives to allogeneic blood transfusions?
Autologous transfusions use the patient’s own blood. But, they’re not always possible. Research is exploring new options.
What is being done to improve the safety and efficacy of allogeneic blood transfusions?
New technologies and research are making transfusions safer and more effective. Our team keeps up with these advancements.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10270726/










