Multiple myeloma is a type of bone marrow cancer. It’s often hard to diagnose because its symptoms are not clear-cut. These symptoms can be mistaken for other, more common conditions.
Fatigue, persistent pain, or unexplained anemia might not make you think of myeloma right away. Such symptoms can result in delays in obtaining accurate diagnosis and timely treatment. Research shows that more than half of myeloma patients face delays of over three months.
We look into how myeloma is often misdiagnosed. We also see why catching it early is key to better health outcomes.
Key Takeaways
- Multiple myeloma symptoms can be mistaken for other diseases.
- Diagnostic delays are common, affecting over 50% of patients.
- Early detection is critical for better patient outcomes.
- Common misdiagnoses include osteoporosis and rheumatoid arthritis.
- Understanding myeloma diagnosis better can improve healthcare.
The Nature of Multiple Myeloma
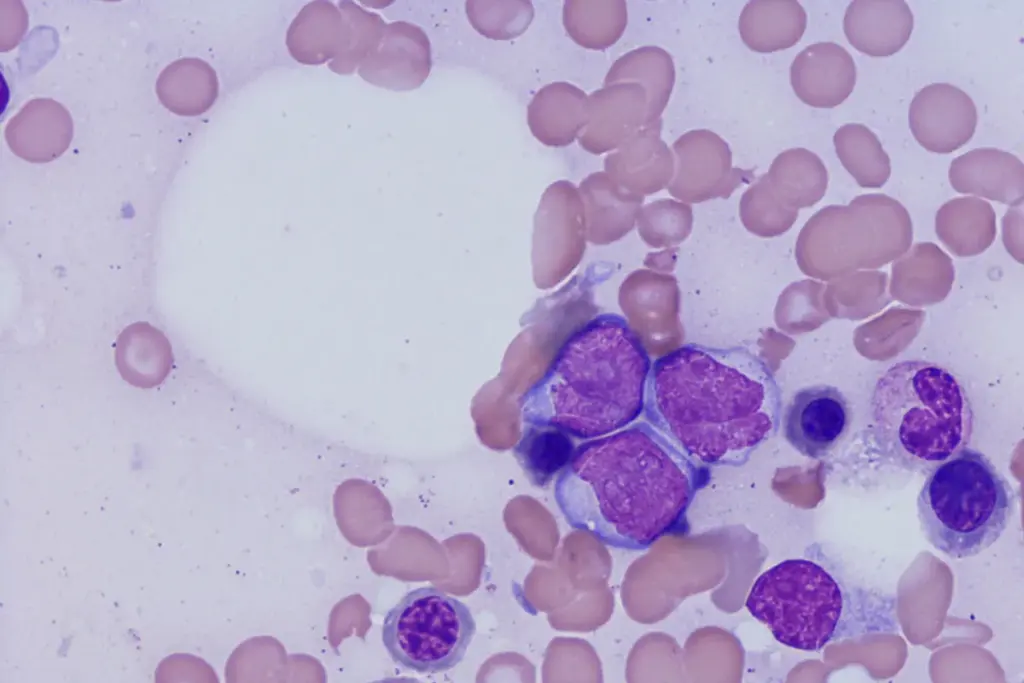
Understanding multiple myeloma involves recognizing that it is a plasma cell disorder. It’s a cancer where bad plasma cells grow in the bone marrow. This can really hurt a person’s quality of life.
Defining Multiple Myeloma as a Plasma Cell Disorder
Multiple myeloma is a cancer that attacks plasma cells, key to our immune system. Plasma cells make antibodies to fight off infections. But in multiple myeloma, these cells turn bad and pile up in the bone marrow.
This buildup can cause anemia, bone pain, and make infections more likely. Early diagnosis is critical to manage the disease well and help patients.
Prevalence and Demographics
Multiple myeloma makes up about 1% of all cancers and over 10% of blood cancers. It mostly hits people over 65. Understanding the demographics helps find who’s at risk and catch it early.
Impact on Bone Marrow Function
The bad plasma cells in multiple myeloma mess up the bone marrow. This leads to fewer healthy blood cells, causing anemia, infections, and bleeding problems. It also causes bone damage and high calcium levels.
Seeing how multiple myeloma affects the bone marrow is key. It helps us understand how the disease grows and why we need to act fast.
Common Symptoms That Lead to Misdiagnosis
Many cases of multiple myeloma are misdiagnosed because of its early symptoms. These symptoms are often vague and can be mistaken for other illnesses. This makes it hard to diagnose correctly.
Non-Specific Nature of Early Symptoms
The early signs of multiple myeloma are non-specific. People might feel tired, lose weight, and feel generally unwell. These symptoms can be confused with other common illnesses, causing delays in diagnosis.
Bone Pain Patterns and Characteristics
Bone pain is a common symptom of multiple myeloma. It often feels like a persistent ache in the back, ribs, or hips. This pain can be misattributed to osteoporosis or other bone-related conditions. It’s important to understand the patterns and characteristics of bone pain for accurate diagnosis.
Fatigue and Weakness Manifestations
Fatigue and weakness are common in patients with multiple myeloma. These symptoms can be mistaken for anemia or other chronic conditions. This makes the diagnostic process even more complicated.
Renal Dysfunction Indicators
Renal dysfunction is another common symptom of multiple myeloma. It often shows as kidney damage or failure. It’s important to recognize the indicators of renal dysfunction for timely intervention.
|
Symptom |
Common Misdiagnosis |
Key Diagnostic Features |
|---|---|---|
|
Bone Pain |
Osteoporosis, Degenerative Disc Disease |
Persistent ache, often in back, ribs, or hips |
|
Fatigue and Weakness |
Anemia, Chronic Fatigue Syndrome |
Unexplained and persistent tiredness |
|
Renal Dysfunction |
Chronic Kidney Disease, Nephrotic Syndrome |
Kidney damage or failure, proteinuria |
Bone Marrow Cancer: Multiple Myeloma vs. Other Malignancies
It’s important to tell multiple myeloma apart from other bone marrow cancers. This is key for the right diagnosis and treatment. Multiple myeloma is a specific bone marrow cancer different from leukemia and lymphoma.
Distinguishing Features of Multiple Myeloma
Multiple myeloma has unique features that make it stand out. It’s marked by the growth of bad plasma cells in the bone marrow. These cells make abnormal proteins that can harm the kidneys and bones.
These abnormal proteins, or M proteins, are a key sign of multiple myeloma. Tests like serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) find and measure these proteins.
Comparison with Leukemia
Leukemia is a blood cancer that starts in the bone marrow. It’s different from multiple myeloma because it involves too many immature white blood cells. Myeloma, on the other hand, involves plasma cells.
Both can cause joint pain due to bone damage. But, the reasons behind this pain are different for each condition.
Comparison with Lymphoma
Lymphoma affects the lymphatic system, like lymph nodes and spleen. It can also be in the bone marrow, but it starts elsewhere than myeloma.
Diagnosing lymphoma often means looking at lymph nodes. But, myeloma is diagnosed through bone marrow biopsies and finding M proteins.
Metastatic Bone Cancers That Mimic Myeloma
Metastatic bone cancers, from places like the breast or lung, can look like myeloma’s bone damage. Advanced scans like PET and MRI help tell them apart.
Knowing where the cancer comes from is key for treatment. A biopsy and looking at tissue under a microscope are vital for a correct diagnosis.
Rheumatological Conditions Confused with Myeloma
Some rheumatological diseases can look a lot like multiple myeloma. This makes it hard to tell them apart. Both can have similar symptoms, leading to wrong diagnoses.
Rheumatoid Arthritis Similarities
Rheumatoid arthritis (RA) is a long-term disease that can cause joint pain and swelling. It can also damage bones, making it hard to tell it apart from myeloma.
RA is treated with special drugs and biologics. But myeloma needs stronger treatments like chemotherapy and stem cell transplants.
Polymyalgia Rheumatica Overlap
Polymyalgia rheumatica (PMR) can also be mistaken for myeloma. It causes muscle pain and stiffness, mainly in older adults. It’s known for high inflammation levels.
PMR quickly gets better with corticosteroids. But myeloma doesn’t react the same way. It’s important to get the diagnosis right to treat patients correctly.
Ankylosing Spondylitis Confusion
Ankylosing spondylitis (AS) mainly hurts the spine and sometimes other joints. Its chronic pain and stiffness can be mistaken for myeloma’s bone pain.
|
Condition |
Primary Symptoms |
Diagnostic Markers |
|---|---|---|
|
Rheumatoid Arthritis |
Joint pain, swelling |
Rheumatoid factor, anti-CCP antibodies |
|
Polymyalgia Rheumatica |
Muscle pain, stiffness |
Elevated ESR, CRP |
|
Ankylosing Spondylitis |
Chronic back pain, stiffness |
HLA-B27 positivity, sacroiliitis on imaging |
|
Multiple Myeloma |
Bone pain, fatigue, weight loss |
M-protein in serum/urine, bone marrow plasmacytosis |
It’s key to know the differences to diagnose and treat right. It is essential to closely examine symptoms that might indicate either a rheumatological disease or myeloma.
Orthopedic Issues Mistaken for Myeloma
Orthopedic problems like osteoporosis and degenerative disc disease can look like multiple myeloma symptoms. This makes it hard to diagnose. Many patients are wrongly diagnosed because their symptoms are similar to those of orthopedic conditions.
Osteoporosis and Pathological Fractures
Osteoporosis weakens bones, making them break easily. Pathological fractures happen when a bone breaks because of a disease. This can be a sign of multiple myeloma.
It’s important to tell the difference between osteoporotic fractures and those from myeloma. Osteoporosis is common in older adults. But myeloma fractures often come with other symptoms like anemia or kidney problems.
Degenerative Disc Disease
Degenerative disc disease affects the spine, causing pain and stiffness. Its symptoms can be similar to those of multiple myeloma, like back pain.
To make a correct diagnosis, we use imaging and lab tests. For example, magnetic resonance imaging (MRI) can spot myeloma’s lytic lesions. This helps tell it apart from degenerative disc disease.
Knee and Hip Joint Disorders
Knee and hip joint problems, like osteoarthritis, can cause pain and mobility issues. These symptoms are similar to those of multiple myeloma. Multiple myeloma hip pain or knee pain might be mistaken for joint disease.
A detailed medical history, physical exam, and tests are key to tell these conditions apart. We must think of myeloma in patients with joint pain, if they have other symptoms too.
Monoclonal Gammopathy of Undetermined Significance (MGUS)
Understanding MGUS is key to spotting multiple myeloma early. MGUS is when abnormal proteins, called monoclonal proteins or M proteins, show up in the blood. These proteins come from plasma cells in the bone marrow.
Defining MGUS and Its Relationship to Myeloma
MGUS is a step before multiple myeloma and other plasma cell disorders. It means you’re at higher risk for myeloma, but not everyone with MGUS will get it. The exact cause of MGUS is not known, but it’s more common in older adults and some ethnic groups.
Key characteristics of MGUS include:
- Presence of monoclonal proteins in the blood or urine
- Less than 10% plasma cells in the bone marrow
- No symptoms of multiple myeloma or other plasma cell disorders
MGUS Cancer Symptoms vs. Myeloma Symptoms
MGUS often doesn’t show symptoms, making it hard to catch without tests. Myeloma, on the other hand, has clear symptoms like bone pain, fatigue, and anemia. Even though MGUS doesn’t have symptoms, it’s important to watch for any signs of myeloma.
Progression Risk and Monitoring
People with MGUS need regular check-ups to watch for signs of myeloma or other disorders. The chance of moving to myeloma varies, depending on the monoclonal protein level and genetic changes.
|
Risk Factor |
Description |
Impact on Progression Risk |
|---|---|---|
|
Level of Monoclonal Protein |
Higher levels indicate a greater risk |
Increased risk of progression |
|
Genetic Abnormalities |
Presence of certain genetic changes |
Higher risk of progressing to myeloma |
|
Age and Health Status |
Older age and poorer health |
Increased vulnerability to progression |
Regular visits to healthcare providers are vital for MGUS patients. It helps manage the condition and quickly address any issues.
Smoldering Multiple Myeloma (SMM)
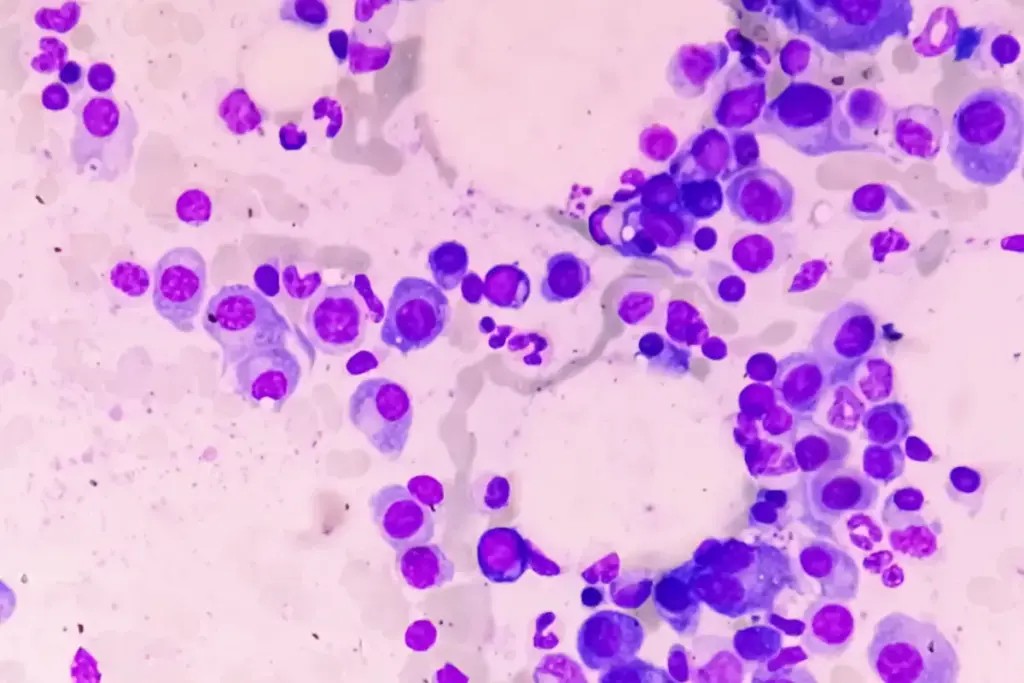
Smoldering multiple myeloma (SMM) is a plasma cell disorder. It falls between monoclonal gammopathy of undetermined significance (MGUS) and active multiple myeloma. Knowing about SMM is key because it’s a higher risk stage than MGUS.
Diagnostic Criteria for SMM
To diagnose SMM, doctors look for certain signs. These signs help tell it apart from MGUS and active multiple myeloma. The criteria include:
- A serum M-protein level of 3 g/dL or higher, or 500 mg or more of M-protein in the urine.
- The presence of clonal plasma cells in the bone marrow, typically between 10% to 59%.
- The absence of myeloma-defining events or amyloidosis.
These criteria are important for spotting SMM. They help doctors tell it apart from MGUS or active myeloma.
Distinguishing SMM from Active Myeloma
The main difference between SMM and active multiple myeloma is the presence of myeloma-defining events. Active myeloma has:
- CRAB criteria (hypercalcemia, renal insufficiency, anemia, and bone lesions).
- Biomarkers of malignancy, such as a high level of circulating plasma cells or certain genetic abnormalities.
Patients with SMM don’t have these signs. But, they are more likely to turn into active disease.
Monitoring Approaches and Progression Indicators
Keeping an eye on SMM is important. It helps catch signs of turning into active myeloma early. This includes:
- Regular blood tests to check M-protein levels and other important factors.
- Periodic bone marrow biopsies to see how many clonal plasma cells there are.
- Imaging studies, like PET/CT scans, to find new bone lesions.
Signs of getting worse include rising M-protein levels, CRAB criteria, or new bone lesions. Catching these signs early means doctors can act fast.
Kidney-Related Conditions Mimicking Myeloma
Kidney problems can look a lot like multiple myeloma, making it hard to tell them apart. We’ll look at how kidney diseases can be mistaken for myeloma. This shows why we need to be careful when diagnosing.
Chronic Kidney Disease Similarities
Chronic kidney disease (CKD) slowly damages the kidneys. Symptoms like tiredness, swelling, and changes in how you pee can be seen in both CKD and myeloma. CKD can also cause toxins to build up in the body, leading to symptoms seen in myeloma patients.
Here are some key similarities between CKD and myeloma:
- Fatigue and weakness
- Swelling in legs and feet
- Changes in urination patterns
Nephrotic Syndrome Overlap
Nephrotic syndrome is a kidney problem that makes you lose too much protein in your pee. This can cause infections and blood clots, just like in myeloma patients.
|
Condition |
Symptoms |
Complications |
|---|---|---|
|
Nephrotic Syndrome |
Severe swelling, fatigue |
Infections, blood clots |
|
Multiple Myeloma |
Bone pain, fatigue |
Fractures, infections |
Amyloidosis Confusion
Amyloidosis is when amyloid fibrils build up in body tissues. This can harm the kidneys and cause symptoms like weight loss and tiredness, similar to myeloma.
It’s important to know the differences and similarities between these kidney issues and myeloma. This helps us make the right diagnosis and treatment. We’ll keep exploring these details in the next sections.
Neurological Manifestations and Misdiagnoses
Neurological problems are common in multiple myeloma, making diagnosis tricky. This disease can harm the nervous system in many ways. It causes symptoms that might be mistaken for other illnesses.
Spinal Cord Compression Symptoms
Spinal cord compression is a serious issue in multiple myeloma. It happens when tumors or bone pieces press on the spinal cord. Symptoms include:
- Back pain
- Radicular pain (pain that radiates along a nerve)
- Weakness or numbness in the legs
- Loss of bladder or bowel control
It’s vital to spot these symptoms early. This helps prevent lasting damage to the nervous system.
Peripheral Neuropathy Confusion
Peripheral neuropathy is damage to the nerves outside the brain and spinal cord. It can cause numbness, tingling, and pain in the hands and feet. It’s often mistaken for diabetes or vitamin deficiencies. So, it’s key to think of multiple myeloma when diagnosing.
Multiple Myeloma of the Spine vs. Other Spinal Disorders
Multiple myeloma can affect the spine, causing fractures or tumors. These can look like other spinal problems like degenerative disc disease or osteoporosis. Accurate diagnosis needs imaging studies (like MRI, CT scans) and lab tests (like serum protein electrophoresis, bone marrow biopsy) to tell it apart from other conditions.
We stress the need for a thorough diagnostic process. This helps find the real cause of neurological symptoms in patients with suspected multiple myeloma. It leads to better treatment and outcomes for patients.
Hematological Disorders Confused with Myeloma
Diagnosing multiple myeloma can be tricky because its symptoms are similar to other blood disorders. Getting the right diagnosis is key to treating the patient effectively.
Anemia of Chronic Disease
Anemia of chronic disease can look like multiple myeloma because both cause fatigue and weakness. It happens in people with long-term illnesses like infections or cancer. Doctors figure out the cause by checking for other anemia reasons and finding the chronic illness.
Key differences between anemia of chronic disease and multiple myeloma:
|
Characteristics |
Anemia of Chronic Disease |
Multiple Myeloma |
|---|---|---|
|
Underlying Cause |
Chronic infection, autoimmune disorder, or cancer |
Malignant plasma cell proliferation |
|
Bone Marrow Involvement |
Typically not directly involved |
Direct involvement with clonal plasma cells |
|
Serum Protein Electrophoresis (SPEP) |
Usually normal or non-specific changes |
Often shows monoclonal protein spike |
Other Plasma Cell Disorders
Waldenström macroglobulinemia and plasma cell leukemia can also be mistaken for multiple myeloma. They share some traits but have unique features that need different treatments.
Benign Monoclonal Gammopathies
Benign monoclonal gammopathies, like MGUS, have monoclonal proteins in the blood but are usually harmless. Yet, they can turn into myeloma or other plasma cell disorders, so they need to be watched closely.
Telling benign monoclonal gammopathies apart from myeloma is important. It helps decide the best treatment and what to expect for the patient’s future.
Diagnostic Delays: Statistics and Consequences
Diagnostic delays in multiple myeloma are a big worry. They affect how well patients do and their quality of life. Getting a diagnosis for multiple myeloma often takes a long time.
Average Time from Symptoms to Diagnosis
Research shows that it can take months to over a year to get diagnosed. This prolonged waiting period can exacerbate the condition and diminish treatment opportunities.
Impact of Delayed Diagnosis on Disease Progression
Not getting diagnosed fast enough can make the disease worse. This leads to more serious symptoms and problems. Getting help early is key to better outcomes.
Risk of Complications from Diagnostic Delays
Waiting too long to get diagnosed raises the risk of serious issues. These include bone breaks, kidney failure, and high calcium levels. These problems can really hurt a patient’s life and chances of survival.
Psychological Impact of Diagnostic Uncertainty
The uncertainty of waiting for a diagnosis can be significantly distressing for patients. It causes a lot of worry and stress. Doctors should help and support patients during this tough time.
|
Aspect |
Impact of Diagnostic Delays |
|---|---|
|
Disease Progression |
Increased risk of severe symptoms and complications |
|
Complications |
Bone fractures, renal failure, hypercalcemia |
|
Psychological Impact |
Anxiety, stress, and uncertainty |
Modern Diagnostic Approaches for Multiple Myeloma
Diagnosing multiple myeloma has gotten much better thanks to new techniques. These advances have made it easier and more accurate to spot this disease.
Blood Tests and Biomarkers
Blood tests are key in finding multiple myeloma. Complete Blood Count (CBC) and blood chemistry tests check for unusual blood cells and kidney problems.
Looking for monoclonal proteins (M-protein) in the blood is important. serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) help find and measure these proteins.
Imaging Techniques
Imaging is vital for seeing how much bone disease there is. Whole-body low-dose computed tomography (CT) scans find bone lesions well.
Magnetic Resonance Imaging (MRI) is great for checking the spine and bone marrow.
Bone Marrow Biopsy Procedures
A bone marrow biopsy is a must for diagnosing multiple myeloma. It takes a bone marrow sample for testing.
The biopsy shows how many plasma cells are in the marrow. This is key for diagnosing and knowing how serious the disease is.
Genetic and Molecular Testing
Fluorescence In Situ Hybridization (FISH) and other tests find specific genetic changes in multiple myeloma.
These tests give important info on how likely the disease is to come back. They help doctors decide the best treatment and how to manage the disease.
The Role of Multidisciplinary Teams in Accurate Diagnosis
Multidisciplinary teams are key to getting accurate diagnoses for patients with multiple myeloma. This plasma cell disorder is complex. It needs a team effort from different medical fields.
Coordination Between Specialists
Good teamwork is essential for accurate diagnosis. We team up hematologists, oncologists, radiologists, and pathologists. They share their knowledge and insights. This teamwork makes sure all parts of the patient’s condition are looked at, lowering the chance of wrong diagnoses.
Key benefits of coordination between specialists include:
- Comprehensive review of patient data
- Integration of various diagnostic tests and results
- Enhanced understanding of the disease’s progression
- Better-informed treatment decisions
Comprehensive Assessment Approaches
Getting a complete picture is vital for diagnosing multiple myeloma. We use many tools like blood tests, bone marrow biopsies, imaging studies, and genetic testing. This wide range of methods helps us understand the patient’s condition fully.
The use of advanced diagnostic techniques has significantly improved our ability to diagnose multiple myeloma accurately. By combining these techniques with our clinical knowledge, we can create treatment plans that meet each patient’s needs.
Case Conferences and Expert Consultation
Case conferences and expert consultations are key to our diagnostic process. These meetings let us discuss tough cases, share knowledge, and get extra help when needed. By combining our experiences and insights, we can make more accurate diagnoses and develop effective treatment plans.
The benefits of case conferences include:
- Improved diagnostic accuracy through collaborative discussion
- Access to a broader range of expertise
- Enhanced patient care through coordinated treatment plans
By using the strengths of a multidisciplinary team, we can give our patients the most accurate diagnoses and best treatment options.
Patient Experiences: The Journey to Correct Diagnosis
Getting a diagnosis of multiple myeloma is often a long and tough journey. It involves many doctor visits and wrong diagnoses. This can lead to delayed treatment and more problems.
Common Misdiagnosis Patterns
Multiple myeloma symptoms can be hard to spot because they’re similar to other diseases. Patients might feel bone pain, get tired easily, and have kidney problems. These signs can point to many other illnesses.
Many patients are first thought to have osteoporosis, rheumatoid arthritis, or chronic kidney disease. This mistake happens because the symptoms are similar. Also, some doctors might not know much about multiple myeloma.
|
Common Misdiagnoses |
Similar Symptoms |
|---|---|
|
Osteoporosis |
Bone pain, pathological fractures |
|
Rheumatoid Arthritis |
Joint pain, fatigue |
|
Chronic Kidney Disease |
Renal dysfunction, fatigue |
Red Flags That Suggest Myeloma
Some symptoms and lab results can hint at multiple myeloma. Look out for ongoing bone pain, unexplained anemia, and high calcium levels.
Key red flags include:
- Persistent bone pain
- Unexplained anemia
- Elevated calcium levels
- Renal impairment
Spotting these signs early is key to getting the right treatment fast.
Advocating for Appropriate Testing
When myeloma is suspected, both patients and doctors should push for the right tests. This means blood tests, PET scans, and bone marrow biopsies.
Early and accurate diagnosis is vital for starting the right treatment. Knowing the common mistakes and the red flags helps us act quickly.
Improving Early Detection of Multiple Myeloma
It’s key to get better at finding multiple myeloma early. This cancer affects plasma cells in the bone marrow. It’s hard to catch early because it doesn’t always show clear symptoms.
To find it sooner, we must focus on three main areas. We need to screen those at high risk, teach doctors about it, and make patients aware.
Screening High-Risk Populations
Finding people at high risk for multiple myeloma is a big step. Those at risk include people with a family history, MGUS, or certain genetic issues. By checking these groups, we can spot the disease early. This could lead to better treatment results.
- Watching high-risk people closely can catch the disease before it gets worse.
- Using new tests and scans can help find multiple myeloma early.
Education for Primary Care Physicians
Doctors in primary care are key in spotting multiple myeloma early. Teaching them about the disease’s early signs can cut down on delays. Important things to teach include:
- Knowing the vague symptoms like bone pain, tiredness, and low blood count.
- Understanding the need for blood tests and protein tests.
- Knowing when to send patients to specialists for more checks.
Patient Awareness Initiatives
It’s also important to educate patients. Telling them about the disease’s symptoms and the need to see a doctor can speed up diagnosis. Ways to do this include:
- Running public campaigns to spread the word about multiple myeloma.
- Creating materials for patients to learn about the disease’s signs.
- Encouraging patients to push for medical checks if they notice strange symptoms.
By working on these areas, we can find multiple myeloma sooner. This leads to better care and outcomes for patients.
Conclusion: Navigating the Diagnostic Challenges of Multiple Myeloma
Multiple myeloma is hard to diagnose because its symptoms are not clear and it’s complex. We’ve looked at what this plasma cell disorder is, its symptoms, and how doctors find it today.
Getting a correct diagnosis early is key. Doctors need to know the unique signs of multiple myeloma and how it’s different from other diseases. This helps them make the right choices for treatment.
By teaching doctors and patients more about multiple myeloma, we can spot it sooner. This leads to better treatments and a better life for those with this disease.
As we learn more about multiple myeloma, we’re getting closer to better care for patients everywhere.
FAQ
What are the common symptoms of multiple myeloma?
Symptoms of multiple myeloma include bone pain and anemia. Fatigue, weakness, and kidney problems are also common. These signs can be similar to other diseases, making it hard to diagnose.
How is multiple myeloma different from other bone marrow cancers like leukemia and lymphoma?
Multiple myeloma is a unique cancer that affects plasma cells in the bone marrow. It’s different from leukemia, which affects blood and bone marrow, and lymphoma, which targets the immune system. Knowing these differences is key to correct diagnosis.
What is MGUS, and how is it related to multiple myeloma?
MGUS stands for Monoclonal Gammopathy of Undetermined Significance. It’s a condition where proteins in the blood are abnormal. MGUS can turn into multiple myeloma. It’s important to watch it closely for any signs of progression.
What is smoldering multiple myeloma (SMM), and how is it different from active myeloma?
SMM is a condition that needs close monitoring because it can turn into active myeloma. It’s diagnosed by specific criteria. Knowing the difference between SMM and active myeloma is important for treatment.
How can rheumatological conditions be confused with multiple myeloma?
Conditions like rheumatoid arthritis can be mistaken for multiple myeloma. This is because they share symptoms like joint and bone pain.
What are the diagnostic approaches used to diagnose multiple myeloma?
Doctors use blood tests, imaging, bone marrow biopsies, and genetic tests to diagnose multiple myeloma. These methods help accurately diagnose and understand the disease.
Why is early detection of multiple myeloma important?
Catching multiple myeloma early is critical. Delayed diagnosis can lead to worse outcomes and more complications. To improve early detection, we need to screen at-risk groups, educate doctors, and raise patient awareness.
What is the role of multidisciplinary teams in diagnosing multiple myeloma?
Teams of specialists are essential for diagnosing multiple myeloma. They work together to ensure patients get the right diagnosis and treatment quickly.
Can multiple myeloma be misdiagnosed as other conditions?
Yes, multiple myeloma can be mistaken for conditions like osteoporosis or rheumatoid arthritis. Its symptoms are not unique, making accurate diagnosis important.
What are the consequences of delayed diagnosis of multiple myeloma?
Delayed diagnosis can lead to serious complications and disease progression. It’s vital to recognize the warning signs and push for timely testing to avoid these issues.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC12249263/










