Getting a platelet infusion can be scary, especially if you have health issues. At Liv Hospital, we aim to give top-notch care. We also support international patients fully.
After a platelet infusion, most people see their platelet count go up fast. This helps with blood clotting and lowers the chance of bleeding. It’s very important for those with low platelets or going through cancer treatments.
We know how vital it is to be well-informed and safe. In this article, we’ll talk about what happens after a platelet infusion. We’ll cover the good sides, the possible downsides, and our top-notch care methods.
Key Takeaways
- Platelet infusions quickly boost platelet count, helping with blood clotting.
- Bleeding risks drop a lot after the treatment.
- People with low platelets or cancer patients get a lot of help.
- Liv Hospital offers full support and world-class care.
- Knowing the good and bad is key for good care.
Understanding Platelets and Their Function

Platelets are key to stopping bleeding in our bodies. They are small, irregularly-shaped blood cells that help with blood clotting. Let’s dive into their role and why they’re important for healing.
The Role of Platelets in Blood Clotting
Platelets are made in the bone marrow and are essential for clotting. When a blood vessel gets hurt, platelets stick to the damage. They form a plug to stop bleeding and start the healing process.
Key steps in platelet activation and aggregation include:
- Adhesion to the site of injury
- Release of chemical signals to attract more platelets
- Aggregation of platelets to form a plug
Normal Platelet Count and Function
A normal platelet count is between 150,000 and 450,000 per microliter of blood. It’s not just about the number; how well they work is also crucial. Knowing both count and function helps manage patients needing platelet transfusions.
|
Platelet Count Range |
Status |
Description |
|---|---|---|
|
150,000 – 450,000/µL |
Normal |
Normal platelet count, indicating healthy platelet production and function. |
|
< 150,000/µL |
Thrombocytopenia |
Low platelet count, potentially leading to bleeding risks. |
|
> 450,000/µL |
Thrombocytosis |
High platelet count, potentially increasing the risk of thrombosis. |
Platelet transfusions are needed for patients with low counts or dysfunction to prevent bleeding. Understanding platelet count and function helps healthcare providers decide on transfusions and monitor patients after.
When Is a Platelet Transfusion Necessary?

Platelet transfusions are crucial for preventing and treating bleeding in patients with low platelet counts. This condition, called thrombocytopenia, can happen due to many reasons. These include bone marrow failure, cancer, and some medicines.
Medical Conditions Requiring Platelet Transfusions
Several medical conditions may need a platelet transfusion. These include:
- Cancer and its treatment, which can suppress bone marrow activity.
- Bone marrow failure syndromes, such as aplastic anemia.
- Severe infections or inflammation that can consume platelets.
- Certain medications that affect platelet production or function.
Thrombocytopenia and Its Causes
Thrombocytopenia is when the blood has fewer platelets than normal. It can be caused by many things, including:
|
Cause |
Description |
|---|---|
|
Bone Marrow Failure |
The bone marrow fails to produce enough platelets. |
|
Cancer Treatments |
Chemotherapy and radiation therapy can lower platelet production. |
|
Medications |
Certain drugs can harm platelet production or increase their destruction. |
Cancer Treatments and Platelet Depletion
Cancer treatments, especially chemotherapy and radiation, can harm the bone marrow. This can lead to thrombocytopenia. In these cases, platelet transfusions are often needed to prevent or manage bleeding.
Platelet transfusion guidelines suggest transfusions for those at high risk of bleeding. The decision to transfuse platelets depends on the patient’s condition, platelet count, and the reason for thrombocytopenia.
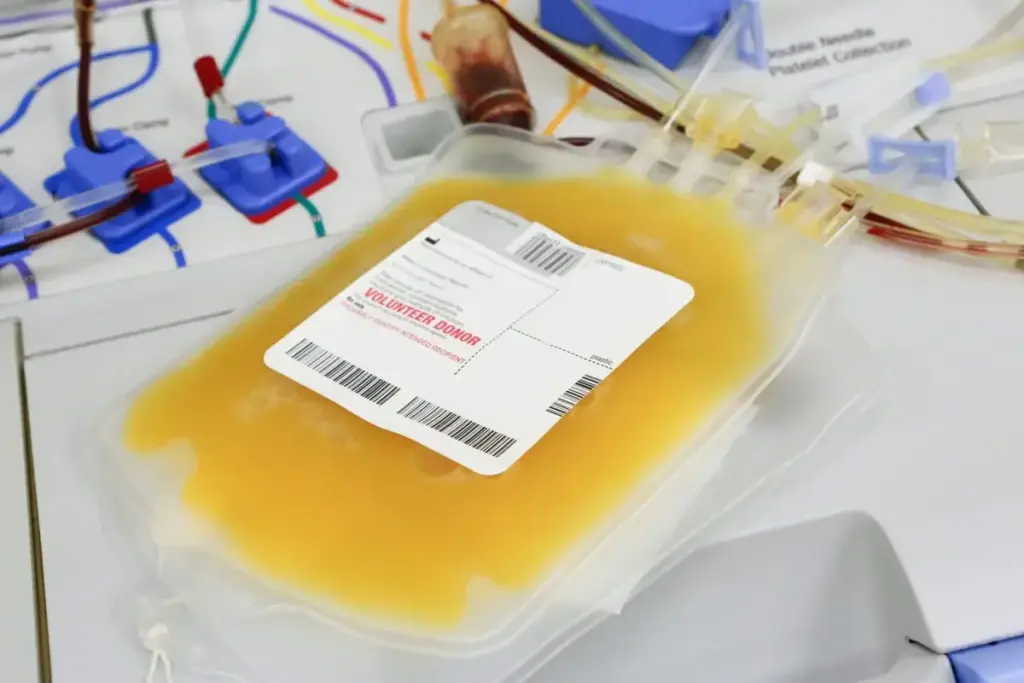
The Platelet Transfusion Process
The platelet transfusion process is key for treating many medical issues. It helps when platelet count or function is low. Knowing what to expect can make the process less scary.
Preparation for a Platelet Infusion
Before starting, we make sure patients are ready. We check their vital signs and find a vein for the transfusion. Getting ready right is important for a good transfusion.
Patients sit or lie down for comfort. We also look at their medical history for any risks.
Duration of a Typical Platelet Transfusion
The time for a platelet transfusion varies. It depends on the patient’s health and the transfusion’s needs. Usually, it takes 30-60 minutes. But, it can be shorter or longer.
We watch the patient’s vital signs closely. This helps us catch any problems fast.
What to Expect During the Procedure
Patients sit or lie down during the transfusion. We give the transfusion slowly to keep things safe. Our team watches over the patient the whole time.
If patients feel any discomfort, they should tell us. We aim to make the experience as easy as possible. We’re ready to adjust the transfusion if needed.
Immediate Effects After a Platelet Infusion
After a platelet transfusion, the patient’s platelet count quickly goes up. This fast increase helps with blood clotting and lowers the chance of bleeding.
Rapid Increase in Platelet Count
The main aim of a platelet infusion is to increase the patient’s platelet count safely. This reduces the risk of bleeding on its own. Studies show that platelet count goes up within hours after the transfusion.
Timeline of Platelet Count Changes
The time it takes for platelet count changes can vary. It depends on the patient’s health and medical condition. Usually, the count stays high for a few days after the transfusion. Regular monitoring is key to track these changes and adjust treatment plans.
Initial Monitoring Post-Transfusion
After a platelet infusion, initial monitoring is crucial. It ensures the patient is not having a bad reaction to the transfusion. This monitoring includes checking the platelet count and looking for signs of bleeding or other issues.
Healthcare providers watch patients closely during this time. They make changes to the care plan as needed to get the best results.
Benefits of Platelet Transfusion Therapy
Platelet transfusion therapy is crucial for people with certain medical conditions. It can be a lifesaver. This treatment greatly improves patient outcomes and supports critical medical procedures.
Platelet transfusions have many benefits. They mainly help with blood clotting. By increasing platelet count, they reduce the risk of bleeding.
Improved Blood Clotting Ability
Platelet transfusions greatly improve blood clotting. Platelets are key in forming clots to stop bleeding. When platelet counts are low, the risk of severe bleeding increases.
Transfusions help the body form clots better. This reduces the risk of severe bleeding.
Key benefits of improved blood clotting include:
- Reduced risk of hemorrhage
- Enhanced healing process
- Minimized need for additional surgical interventions
Reduced Risk of Spontaneous Bleeding
Platelet transfusions also lower the risk of spontaneous bleeding. Patients with low platelet counts face a higher risk of spontaneous bleeding. This can be life-threatening.
By increasing platelet count through transfusion, we reduce this risk. This makes treatment safer for patients.
“Platelet transfusions are a critical component of supportive care for patients with thrombocytopenia or platelet dysfunction.”
Source: American Society of Hematology
Support During Surgical Procedures
Platelet transfusions are also vital during surgeries. They ensure patients have enough platelets. This reduces the risk of bleeding complications during surgery.
This support is crucial for the success of the surgery. It helps in the patient’s overall recovery.
|
Benefit |
Description |
|---|---|
|
Improved Blood Clotting |
Enhances the body’s ability to form clots, reducing the risk of hemorrhage. |
|
Reduced Risk of Spontaneous Bleeding |
Decreases the likelihood of spontaneous bleeding episodes. |
|
Support During Surgery |
Provides critical support during surgical procedures, minimizing bleeding risks. |
In conclusion, platelet transfusion therapy is a vital treatment. It offers many benefits, including better blood clotting, reduced bleeding risk, and support during surgeries. Understanding these benefits highlights the importance of this therapy in patient care.
Common Mild Reactions to Platelet Transfusions
Platelet transfusions are usually safe, but some people might feel mild side effects. These effects are not severe but can still cause discomfort. They are a concern for those getting transfusions.
Febrile Non-Hemolytic Transfusion Reactions
Febrile non-hemolytic transfusion reactions (FNHTR) are common, happening in 1-4% of transfusions. They show as a body temperature rise, sometimes with chills or shivering. FNHTR is usually not a cause for significant concern and can often be managed with supportive care, such as antipyretic medications.
Allergic Responses and Their Management
Allergic reactions to platelet transfusions can happen, showing as hives, itching, or severe skin issues. These reactions are typically mild and can be managed with antihistamines or other medications. For those with a history of allergic reactions, premedication with antihistamines or corticosteroids might be considered.
Chills and Other Minor Symptoms
Some patients might feel chills, mild discomfort, or other minor symptoms during or after a transfusion. These symptoms are usually short-lived and don’t need special treatment. However, close monitoring is essential to tell these mild reactions from more serious ones.
We know that any reaction during a medical treatment can be worrying. But, our medical team is ready to handle these situations. We provide the care needed to ensure your comfort and safety during the transfusion.
Moderate Complications After Platelet Infusion
Platelet transfusions save lives but can cause moderate problems. These issues can affect how well a patient does and their quality of life. We’ll look at two big problems: Transfusion-Associated Circulatory Overload (TACO) and Transfusion-Related Acute Lung Injury (TRALI), and how to handle them.
Transfusion-Associated Circulatory Overload
TACO happens when too much fluid from transfusions overloads the body. This can cause breathing problems. Signs include trouble breathing, needing to sit up to breathe, and high blood pressure.
Key symptoms of TACO include:
- Dyspnea
- Orthopnea
- Hypertension
- Tachycardia
A study in the Journal of Critical Care shows TACO is a big worry for sick patients getting blood transfusions.
“TACO is a serious complication that can be mitigated with careful transfusion practices.”
– Journal of Critical Care
Transfusion-Related Acute Lung Injury
TRALI is a severe lung problem that can lead to not being able to breathe. It’s caused by fluid in the lungs not due to heart issues. It often happens when blood products with certain antibodies are given.
|
Characteristics |
TACO |
TRALI |
|---|---|---|
|
Primary Cause |
Fluid Overload |
Non-cardiogenic Pulmonary Edema |
|
Symptoms |
Dyspnea, Orthopnea, Hypertension |
Respiratory Distress, Hypoxemia |
|
Management |
Diuretics, Oxygen Therapy |
Supportive Care, Mechanical Ventilation |
Management of Moderate Complications
Handling TACO and TRALI involves supportive care and sometimes special treatments. For TACO, doctors use diuretics and oxygen. For TRALI, patients might need oxygen and a breathing machine.
Management strategies include:
- Supportive care
- Oxygen therapy
- Diuretics for TACO
- Mechanical ventilation for TRALI
Knowing about these complications and how to manage them is key for doctors to help patients. By understanding the risks and acting early, we can lessen the effects of these problems.
Rare but Serious Platelet Transfusion Risks
Platelet transfusions are usually safe, but there are rare risks. It’s important for patients and doctors to know about these risks. This way, they can manage them quickly and properly.
Transfusion-Related Infections
Transfusion-related infections are a serious risk, happening in less than 0.05% of transfusions. These infections can cause sepsis and other dangerous problems. Strict screening processes are in place to minimize this risk, including rigorous testing of donated blood products.
Even with these precautions, the risk of these infections is still a worry. We must watch patients closely after transfusion. We also need to be ready to handle any bad reactions quickly.
Posttransfusion Purpura
Posttransfusion purpura is a rare condition where platelet count drops suddenly after a transfusion. This can cause serious bleeding problems. The exact cause is often related to immune system reactions, and managing it usually involves additional medical therapy to help platelet count recover.
It’s key to understand the risk factors and spot symptoms early to manage posttransfusion purpura well. We work closely with patients to keep an eye on their condition and adjust treatment as needed.
Anaphylactic Reactions
Anaphylactic reactions, though rare, can be deadly and need immediate medical help. These severe allergic reactions can happen when the body reacts to parts of the transfused platelets. Prompt recognition and treatment with epinephrine and other supportive measures are crucial in managing anaphylaxis.
We stress the importance of knowing the signs of anaphylactic reactions. These include trouble breathing, a fast heartbeat, and a drop in blood pressure. This way, we can act fast to help.
Platelet Transfusion in Special Populations
Special groups, like extremely preterm babies, pregnant women, and the elderly, often need platelet transfusions. This is because of their unique health issues or complications.
Extremely Preterm Infants and Associated Risks
Extremely preterm babies face a high risk of bleeding. This makes platelet transfusions very important. Their organs and systems are still developing, which can lead to brain bleeding.
We watch these babies closely for signs of bleeding. We also check their platelet counts often. This helps us decide if they need a transfusion. Our goal is to stop or reduce bleeding that could harm their growth and health.
Pregnant Women
Pregnant women might need platelet transfusions because of issues like preeclampsia or placental abruption. Preeclampsia causes high blood pressure and protein in the urine. This can lead to low platelet counts.
When there’s a big risk of bleeding, platelet transfusions can save lives. We handle these cases carefully to protect both the mother and the baby.
Elderly Patients
Elderly people might need platelet transfusions because of health issues like cancer or bone marrow problems. These conditions can affect platelet production. Age can also make it harder for the body to make platelets.
We look at the health of elderly patients, including any other health problems. This helps us figure out the best way to manage their platelet counts and prevent bleeding.
Long-Term Effects of Multiple Platelet Transfusions
Multiple platelet transfusions save lives but can cause long-term issues. It’s key to know these effects to improve care and avoid problems.
Transfusion-Related Immunomodulation
One major issue is transfusion-related immunomodulation (TRIM). TRIM weakens the immune system after transfusions. This can lead to more infections and affect cancer coming back.
Studies show TRIM can cause more infections and longer hospital stays. We must think carefully about the benefits and risks of transfusions, especially for those needing many.
Platelet Refractoriness Development
Platelet refractoriness is another problem from repeated transfusions. It makes it hard to stop bleeding because the body doesn’t respond well to transfusions. This usually happens because of alloimmunization, where the body makes antibodies against the transfused platelets.
To handle platelet refractoriness, we need to find compatible donors and sometimes use immunosuppressive treatments.
Alloimmunization Concerns
Alloimmunization is a big worry for those getting many transfusions. When the immune system sees transfused platelets as foreign, it makes antibodies. This makes future transfusions harder and can lead to platelet refractoriness.
To reduce alloimmunization, we use leukoreduction and match platelet products for certain antigens.
|
Long-Term Effect |
Description |
Management Strategies |
|---|---|---|
|
Transfusion-Related Immunomodulation |
Immune system suppression increasing infection risk |
Careful transfusion planning, monitoring for infections |
|
Platelet Refractoriness |
Reduced response to platelet transfusions |
Compatible donor selection, immunosuppressive therapies |
|
Alloimmunization |
Production of antibodies against transfused platelets |
Leukoreduction, antigen-matched platelet products |
Knowing the long-term effects of multiple platelet transfusions helps us care for patients better. It’s important to weigh the benefits against the risks and use strategies to avoid complications.
Post-Transfusion Monitoring and Follow-Up
Monitoring after a platelet infusion is key. It includes checking the patient’s platelet count and bleeding risk. This phase is vital for the transfusion’s success and the patient’s health.
Platelet Count Assessment
We check the platelet count after a transfusion to see if it’s safe. This test shows if the transfusion worked well.
Platelet count assessment is important. It helps us see if the transfusion was successful. It also guides future treatment plans.
Bleeding Risk Evaluation
Checking for bleeding risk is crucial. We look for signs of bleeding or factors that might increase it.
Identifying high-risk patients helps us take steps to prevent bleeding. This way, we can reduce the risk of hemorrhage.
Follow-Up Schedule Recommendations
The follow-up schedule varies based on the patient’s needs. We usually recommend regular check-ups to monitor the platelet count and bleeding risk.
A personalized follow-up plan is essential. It ensures patients get the care they need during recovery. We work with patients to create a schedule that fits their needs.
Through careful monitoring and follow-up, we can improve patient outcomes. Our commitment to care goes beyond the transfusion. It includes the entire recovery process.
Current Platelet Transfusion Guidelines
Platelet transfusions have changed a lot. Now, we focus on both preventing and treating bleeding. It’s key to know these guidelines to help patients better.
Prophylactic vs. Therapeutic Transfusion
Platelet transfusions can be used to prevent or treat bleeding. Prophylactic transfusions help patients at risk of bleeding. Therapeutic transfusions are for those with active bleeding.
Studies show the choice between these depends on the patient’s health and platelet count. For example, patients getting chemotherapy often get prophylactic transfusions to avoid severe low platelets.
Threshold Recommendations for Different Conditions
How often to give platelet transfusions varies by condition. For instance, the American Society of Clinical Oncology suggests giving transfusions to patients with platelets below 10,000/μL to stop bleeding. But, patients having major surgery might need a higher count, over 50,000/μL.
|
Clinical Condition |
Recommended Platelet Count Threshold |
|---|---|
|
Prophylaxis in hematologic malignancies |
10,000/μL |
|
Major surgery |
50,000/μL |
|
Neurosurgery or critical bleeding |
100,000/μL |
These guidelines come from many medical groups, including the National Institutes of Health. They help us make sure transfusions are safe and effective.
Best Practices in Transfusion Medicine
Good practices in platelet transfusions include watching patients closely and using the right amount of transfusions. We also need to think about the risks, like TRALI and GVHD.
“The goal of transfusion medicine is to provide safe and effective blood components to patients in need, while minimizing risks and complications.”
– Source: International Society of Blood Transfusion
Following current guidelines and best practices helps us use platelet transfusions wisely. This improves care for patients with low platelets and bleeding issues.
Alternatives to Platelet Transfusion
Platelet transfusions are crucial but not the only option. New treatments are being developed to help patients who need these transfusions.
Stimulating Platelet Production
Thrombopoietin receptor agonists are a promising alternative. These drugs help the bone marrow make more platelets. This could mean fewer transfusions for patients.
These agents work by mimicking thrombopoietin. This natural hormone helps the body produce more platelets.
Examples of these drugs include:
- Romiplostim
- Elthrombopag
- Avatrombopag
Studies show they are effective against low platelet counts. They help prevent bleeding and reduce the need for transfusions.
Stabilizing Clots with Antifibrinolytic Agents
Antifibrinolytic agents are another option. Drugs like tranexamic acid help keep clots stable. They stop excessive bleeding by preventing fibrin breakdown.
These drugs are especially useful in surgeries. They can greatly reduce blood loss and the need for transfusions.
Emerging Therapies and Research
The field of transfusion medicine is always changing. Emerging therapies offer new hope for patients. Researchers are looking into gene therapy and new drugs to tackle platelet transfusion challenges.
|
Therapy |
Description |
Potential Benefits |
|---|---|---|
|
Thrombopoietin Receptor Agonists |
Stimulate platelet production in the bone marrow |
Reduce need for platelet transfusions, manage thrombocytopenia |
|
Antifibrinolytic Agents |
Stabilize clots and prevent excessive bleeding |
Reduce blood loss during surgery, minimize transfusion requirements |
|
Gene Therapy |
Modify genes to correct bleeding disorders or improve platelet function |
Potential long-term solution for certain bleeding conditions |
As research keeps advancing, we’ll see more effective treatments. These will improve patient care and outcomes.
Living with Conditions Requiring Repeated Platelet Transfusions
Living with a condition that needs regular platelet transfusions can be tough. But, with the right strategies, patients can live fulfilling lives. Managing such a condition requires a mix of healthcare and daily living adjustments.
Lifestyle Adjustments
Patients with conditions needing repeated platelet transfusions must make big lifestyle changes. They should avoid activities that raise bleeding risks, like contact sports. It’s important to talk to a healthcare provider to create a personal plan.
Small steps can greatly reduce injury and bleeding risks. For instance, using a soft-bristled toothbrush and avoiding sharp objects can help. Eating a healthy diet full of nutrients also supports overall health and condition management.
Managing Bleeding Risk
Managing bleeding risk is key for those with conditions needing repeated platelet transfusions. Regularly checking platelet counts and knowing bleeding signs are crucial. Patients should quickly tell their healthcare provider about any unusual bleeding or bruising.
Being mindful of your surroundings and taking precautions can help. This might mean removing tripping hazards at home or using handrails on stairs. Understanding your condition’s risks and taking proactive steps can greatly improve your life quality.
Support Resources for Patients
Support resources are vital for patients dealing with the emotional and psychological sides of their condition. Organizations and counseling services offer emotional support. They help patients and their families face the challenges of repeated platelet transfusions.
We suggest patients look into these resources and connect with others facing similar issues. Sharing experiences and advice can be very helpful. These support networks provide valuable guidance and reassurance.
Conclusion
Platelet transfusions are key in helping blood clot and reducing bleeding in patients with low platelets or those getting cancer treatments. At Liv Hospital, we aim to offer top-notch healthcare. We support international patients fully.
Knowing the good and bad of platelet transfusions helps us give our best care. These transfusions save lives for many. We follow the latest guidelines to ensure the best results for our patients.
We are dedicated to providing excellent care and making a difference in our patients’ lives. Focusing on platelet transfusions and other advanced treatments, we stay true to our mission of outstanding healthcare services.
FAQ
What is a platelet infusion, and how long does it take?
A platelet infusion is when platelets are given to a patient to help with blood clotting. It’s done to lower the risk of bleeding. This process usually takes 30-60 minutes.
What are the benefits of platelet transfusion therapy?
Platelet transfusion therapy has many benefits. It improves blood clotting and lowers the risk of bleeding. It’s also crucial during surgeries.
What are the common mild reactions to platelet transfusions?
Common mild reactions include febrile non-hemolytic transfusion reactions, allergic responses, and chills. These reactions are usually treated with medication and are short-lived.
What are the risks associated with platelet transfusions?
Rare but serious complications can happen, like infections and allergic reactions. Moderate issues, like lung problems, can also occur. These risks are why careful monitoring is key.
How is platelet count monitored after a transfusion?
After a transfusion, a patient’s platelet count is checked. This ensures the count has gone up. Regular checks help spot patients at risk for bleeding.
What are the guidelines for platelet transfusions?
Guidelines for platelet transfusions are clear. They cover both preventive and therapeutic uses. The right approach depends on the patient’s condition. Following these guidelines is crucial.
Are there alternatives to platelet transfusions?
Yes, alternatives like thrombopoietin receptor agonists and antifibrinolytic agents are being explored. New treatments and research aim to improve patient care.
How can patients manage bleeding risk after a platelet transfusion?
Patients can manage bleeding risk by keeping an eye on their platelet count. They should also watch for bleeding signs and avoid activities that increase bleeding risk.
What support resources are available for patients requiring repeated platelet transfusions?
Support resources like patient organizations and counseling offer emotional support. They help patients cope with their condition. Patients can also get advice on managing bleeding risk and making lifestyle changes.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/article-abstract/2834703**










