Bcc and squamous cell cancer have key differences. Discover the vital secrets and successful tips for identifying these skin issues today.
It’s important to know the difference between basal cell carcinoma and squamous cell carcinoma. This knowledge helps in preventing, detecting, and treating skin cancer. Every year, over five million Americans are diagnosed with these types of skin cancer. Basal cell carcinoma is found in about 80% of cases, while squamous cell carcinoma makes up 20%.
At LIV Hospital, we focus on giving top-notch care to skin cancer patients. Knowing the details about these two common cancers helps us create treatment plans that fit each patient’s needs.
Key Takeaways
- Basal cell carcinoma is the most common type of skin cancer, accounting for 80% of non-melanoma cases.
- Squamous cell carcinoma is the second most common type of skin cancer, making up around 20% of non-melanoma cases.
- Understanding the differences between basal cell carcinoma and squamous cell carcinoma is essential for effective prevention and treatment.
- Early detection and diagnosis are critical for successful treatment outcomes.
- LIV Hospital is committed to providing high-quality care for patients with skin cancer.
Understanding Skin Cancer Basics

The skin is our body’s largest organ. Knowing how it works is key to understanding skin cancer. It has several layers, with the epidermis on top, followed by the dermis, and then the hypodermis. Each layer has its own role and cells that are important for our health.
The Skin’s Structure and Function
The epidermis, the outermost layer, is made up of epithelial cells like squamous and basal cells. These cells protect us from harm, help regulate body temperature, and make vitamin D. Below the epidermis is the dermis, with tough connective tissue, hair follicles, and sweat glands. The dermis gives the skin strength, flexibility, and elasticity.
The skin’s structure is complex, and its functions are many. Knowing how the layers and cells work together helps us understand skin cancer. For example, basal cell carcinoma starts in the basal cell layer, while squamous cell carcinoma comes from squamous cells.
|
Skin Layer |
Primary Functions |
Cell Types |
|---|---|---|
|
Epidermis |
Protection, Vitamin D synthesis |
Squamous cells, Basal cells |
|
Dermis |
Strength, Elasticity, Hair follicles, Sweat glands |
Connective tissue cells |
|
Hypodermis |
Insulation, Energy storage |
Adipocytes |
How Skin Cancer Develops
Skin cancer starts when skin cells’ DNA gets damaged, often from UV radiation. This damage can cause cells to grow out of control, forming tumors. Skin cancer’s development involves genetics and the environment.
Health experts say knowing the risk factors and taking steps to prevent them can lower skin cancer rates. For more on skin cancer awareness and prevention, check out May Melanoma & Skin Cancer Awareness.
Early detection is key for effective treatment. Spotting the signs and symptoms of skin cancer, like new or changing moles, can lead to early medical help. We’ll explore basal cell carcinoma and squamous cell carcinoma in more detail later.
Basal Cell Carcinoma (BCC): The Most Common Skin Cancer

BCC, or Basal Cell Carcinoma, is the most common skin cancer. It’s important to understand how it forms and looks. Knowing its basics helps us see how it’s different from other skin cancers.
Formation of BCC
BCC starts in the basal cell layer of the skin. This layer makes new skin cells. BCC grows slowly and rarely spreads, but it can damage the skin if not treated.
UV radiation from the sun or tanning beds causes BCC. This radiation damages skin cells’ DNA, leading to cancer. Other factors include genetics and certain chemicals.
Common Locations for BCC
BCC often appears on sun-exposed skin. This includes the face, ears, neck, and scalp. This shows how UV radiation plays a big role in BCC.
Appearance of BCC
BCC can look like a shiny bump, a pink or red patch, or an open sore that won’t heal. It grows slowly and might bleed or crust. Its look can change, so it’s key to watch for new or changing skin spots.
Squamous Cell Carcinoma (SCC): The Second Most Common Skin Cancer
Squamous Cell Carcinoma (SCC) makes up about 20% of non-melanoma skin cancers. It’s important to know about it for early detection and treatment. SCC is the second most common skin cancer.
Formation and Development
SCC starts in the squamous cells, which cover the outer skin layer. When these cells grow out of control, they form a tumor. SCC often comes from too much UV radiation, like from the sun or tanning beds.
The growth of SCC happens through genetic changes in squamous cells. This leads to cells dividing without control. It can spread to other tissues and even to other parts of the body. Knowing the risks, like fair skin and sunburns, helps prevent and catch it early.
Typical Locations and Characteristics
SCC usually shows up on sun-exposed parts like the face, ears, and hands. It can also appear on less common areas like the lips and genitals. SCC can look like a firm, red bump, a scaly patch, or a sore that won’t heal.
SCC often has these traits:
- Rapid growth
- Crusting or bleeding
- Pain or tenderness
Keratoacanthoma is a fast-growing SCC type. It might go away by itself, but it’s still SCC because it can spread.
Comparison of SCC Characteristics
|
Characteristics |
SCC |
Keratoacanthoma |
|---|---|---|
|
Growth Rate |
Variable, can be slow or rapid |
Typically rapid |
|
Appearance |
Varied, can be a nodule, patch, or sore |
Often dome-shaped with a keratin-filled crater |
|
Potential for Invasion |
Yes, can invade surrounding tissues |
Yes, despite sometimes resolving on its own |
Key Differences Between BCC and SCC
It’s important to know the differences between BCC and SCC for good skin cancer care. Both are skin cancers, but they start from different cells and grow in different ways. They also have different chances of spreading.
Cell Origin and Biological Differences
BCC comes from the basal cell layer of the skin. SCC starts from squamous cells. This affects how they act in the body. BCC grows slowly and stays close to where it starts. On the other hand, SCC can grow faster and spread more.
BCC grows slowly and rarely spreads. SCC grows faster and can spread more easily to other parts of the body.
Growth and Metastatic Potential
BCC and SCC grow and spread in different ways. BCC mainly stays in one place but rarely spreads. SCC can spread more easily, especially if it’s not treated quickly or if it’s a high-risk type.
- BCC: Locally invasive, rare metastasis
- SCC: Potential for local invasion and metastasis, especially in high-risk cases
Visual and Symptomatic Differences
BCC and SCC look and feel different. BCC looks like a pearly or waxy bump. SCC is a firm, red nodule or a flat sore with a scaly crust.
Knowing these differences helps catch skin cancer early. Early detection is key for better treatment of both BCC and SCC.
Epidemiology of BCC and SCC
It’s important to understand the spread of BCC and SCC to see how skin cancer affects us. These cancers are becoming more common. We need to look at the trends, who gets them, and why.
Incidence Rates and Trends
Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC) are the top skin cancers. BCC is growing by 3-8% each year, which is a big worry. SCC is less common but still rising, especially in certain groups.
- More UV radiation is a big risk factor.
- Changes in how we live and play also raise the risk.
- Better ways to find these cancers might make them seem more common.
Demographic Patterns
The spread of BCC and SCC shows clear patterns. Older adults get these cancers more often because of more UV exposure over time. Men are more likely to get SCC, but the gap is getting smaller.
|
Demographic Factor |
BCC |
SCC |
|---|---|---|
|
Age |
More common in older adults |
More common in older adults |
|
Gender |
Higher incidence in men |
Higher incidence in men |
Racial and Ethnic Considerations
The color of your skin affects your risk for BCC and SCC. People with fair skin, especially Caucasians, are at the highest risk. Hispanics, Asians, and Africans have a lower risk, but it’s still there, especially for those who spend a lot of time in the sun.
- Caucasians face the highest risk because of less melanin.
- Those with albinism or other melanin issues are also at higher risk.
- It’s key for everyone to know about prevention.
Risk Factors for Developing BCC and SCC
Several factors can increase your chance of getting skin cancer, especially BCC and SCC. Knowing these factors helps in preventing and catching cancer early.
UV Exposure and Sun Damage
UV rays from the sun or tanning beds are big risks for skin cancer. UV rays harm skin cells’ DNA, causing mutations that can lead to cancer.
People at higher risk include those who:
- Have spent a lot of time in the sun
- Live near the equator or at high altitudes
- Use tanning beds
- Have fair skin that burns easily
Genetic Predisposition
Genetics also play a big part in skin cancer risk. If your family has a history of skin cancer, you’re more likely to get it. Some genetic syndromes, like Xeroderma Pigmentosum, make the risk even higher because they affect DNA repair.
Environmental and Lifestyle Factors
Other factors can also raise your risk of BCC and SCC. These include:
|
Risk Factor |
Description |
|---|---|
|
Smoking |
Increases the risk of SCC, particularly in the lips and mouth |
|
Chemical Exposure |
Exposure to certain chemicals, such as arsenic, can increase the risk |
|
Radiation Therapy |
Previous radiation therapy, especially in childhood, can increase the risk of BCC and SCC |
Diagnosing Basal Cell and Squamous Cell Carcinomas
Getting a correct diagnosis is key to managing skin cancer, like BCC and SCC. We use a mix of clinical exams, biopsies, and advanced tests to diagnose these cancers.
Clinical Examination Techniques
Our first step is a clinical exam. We use a special microscope called a dermatoscope to look at skin lesions closely. This helps us spot signs of BCC or SCC that aren’t obvious at first glance.
- Asymmetry and irregular borders
- Color variation within the lesion
- Diameter and elevation
- Symptoms such as bleeding or itching
Biopsy Procedures and Pathology
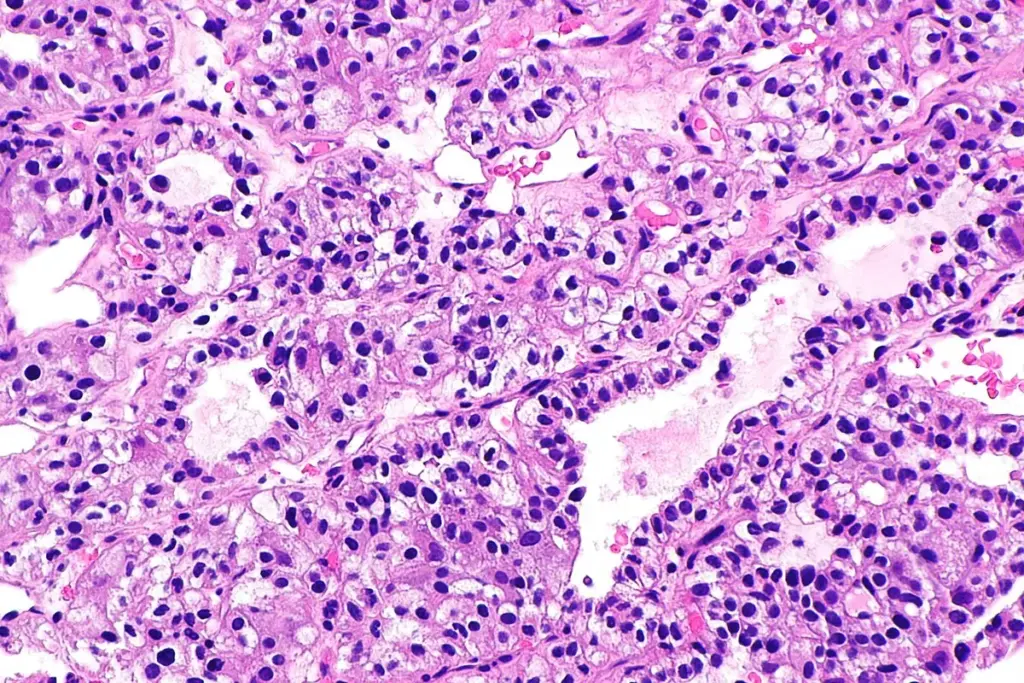
If we think a lesion might be cancer, we do a biopsy to confirm. There are different biopsy methods, like shave, punch, and excisional biopsies. The right method depends on the lesion’s size, location, and what we suspect it might be.
After the biopsy, we send the tissue to a lab for a detailed look. A pathologist checks the tissue under a microscope to see if there are cancer cells and what type they are.
Advanced Diagnostic Methods
In some cases, we use extra tests to help diagnose skin cancer or see how far it has spread. These tests include:
- Imaging tests: Like ultrasound or MRI, to check how deep the cancer is or if it has spread to lymph nodes.
- Molecular diagnostic tests: To find specific genetic changes linked to skin cancer.
|
Diagnostic Method |
Basal Cell Carcinoma (BCC) |
Squamous Cell Carcinoma (SCC) |
|---|---|---|
|
Clinical Examination |
Looks for characteristic features like pearly appearance and telangiectasias |
Examines for signs like scaling, crusting, and induration |
|
Biopsy |
Confirms diagnosis by showing basaloid cells |
Confirms diagnosis by showing squamous cells with atypia |
|
Advanced Diagnostic Tests |
May use imaging for large or deeply invasive tumors |
May use imaging and molecular tests for high-risk SCC |
By using these different methods, we can accurately diagnose BCC and SCC. This is important for choosing the best treatment plan.
Treatment Approaches for BCC
There are many ways to treat basal cell carcinoma (BCC). We use both surgery and non-surgical methods. The right treatment depends on the tumor’s size, where it is, and how aggressive it is. It also depends on the patient’s health and what they prefer.
Surgical Treatment Options
Surgery is a common and effective way to treat BCC. It involves removing the tumor and some healthy tissue around it to make sure it’s all gone. There are a few surgical techniques used:
- Standard Excision: A simple method where the tumor and some healthy tissue are removed.
- Mohs Surgery: This precise method removes the tumor layer by layer. Each layer is checked under a microscope until no cancer is found.
- Curettage and Electrodesiccation: The tumor is scraped out with a curette. Then, an electric current is used to kill any remaining cancer cells.
A study in the Journal of the American Academy of Dermatology found Mohs surgery works well for BCC. It’s especially good for high-risk tumors.
“Mohs surgery is particularly useful for treating BCC in cosmetically sensitive areas or in cases where the tumor’s margins are not clear.”
– Journal of the American Academy of Dermatology
Non-Surgical Interventions
Not all BCCs need surgery. Some can be treated without it. These include:
- Topical Treatments: Creams or gels, like imiquimod or 5-fluorouracil, can work for superficial BCCs.
- Photodynamic Therapy (PDT): This treatment uses a light-sensitive medication and light to kill cancer cells.
- Radiation Therapy: Used for BCCs that are hard to treat with surgery or are in sensitive areas.
|
Treatment Modality |
Indications |
Advantages |
|---|---|---|
|
Surgical Excision |
Tumors that are large or in sensitive areas |
High cure rate, allows for histological examination |
|
Mohs Surgery |
High-risk tumors, tumors in cosmetically sensitive areas |
High cure rate, preserves healthy tissue |
|
Topical Treatments |
Superficial BCCs |
Non-invasive, good cosmetic outcome |
Treatment Selection Criteria
Choosing a treatment for BCC depends on several things. It’s important to talk about the risks and benefits of each option with a healthcare provider.
We look at many factors when picking a treatment plan. We make sure it fits the patient’s needs and preferences.
Treatment Approaches for SCC
SCC treatment options include surgery, radiation, and systemic therapies. Each choice depends on the tumor’s size, location, and the patient’s health.
Surgical Management Strategies
Surgery is a key treatment for SCC. It involves several techniques:
- Surgical Excision: This method removes the tumor and some healthy tissue to ensure all cancer is gone.
- Mohs Surgery: It’s a precise method that removes the tumor layer by layer. Each layer is checked under a microscope until no cancer is found.
- Curettage and Electrodesiccation: This involves scraping away the tumor with a curette and then using electric current to kill any remaining cancer cells.
These surgical methods work well for localized SCC. They offer high cure rates when chosen correctly.
Radiation and Systemic Therapies
When surgery isn’t possible or the cancer has spread, other treatments are used:
- Radiation Therapy: It uses high-energy rays to kill cancer cells. It’s good for SCCs in sensitive areas or for patients who can’t have surgery.
- Systemic Therapies: This includes chemotherapy and targeted therapy. They’re used for SCC that has spread.
Managing High-Risk SCC
High-risk SCC needs aggressive treatment. This includes large tumors, deep invasion, poor differentiation, and perineural invasion. Treatment for such cases may involve:
- Multidisciplinary Care: This means working together with dermatologists, surgeons, oncologists, and other specialists to create a treatment plan.
- Advanced Surgical Techniques: Like Mohs surgery for complex cases.
- Adjuvant Therapies: Using radiation or systemic therapies after surgery to lower the chance of recurrence.
Understanding SCC treatment options helps healthcare providers give personalized care. This improves patient outcomes.
When to Seek Medical Attention
Knowing when to get medical help is key to treating skin cancer well. We’ll show you the signs of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). It’s vital to get help early.
Warning Signs for BCC
Basal cell carcinoma has clear signs you shouldn’t ignore. Look out for:
- A new growth or sore on the skin that doesn’t heal
- A shiny, pink, or red bump, which may be translucent or have visible blood vessels
- A flat, scaly, or crusty patch on the skin
- A scar-like area that is white, yellow, or waxy
If you see any of these, see a dermatologist right away.
Warning Signs for SCC
Squamous cell carcinoma has its own signs. Watch for:
- A firm, red nodule or a flat sore with a scaly or crusted surface
- A new growth or an open sore that doesn’t heal within a few weeks
- A wart-like growth or a sore that bleeds easily
Seeing these signs means you should see a healthcare professional.
The Importance of Early Detection
Finding cancer early is key to treating it well. Early detection means better treatment options. Waiting too long can make treatment harder and less effective.
We strongly advise watching for skin changes and getting medical help if you notice anything odd. Regular self-exams and yearly dermatologist visits help catch cancer early.
Prognosis and Long-term Outlook
Knowing the prognosis for BCC and SCC is key for patients. It helps them understand their treatment paths. The prognosis depends on the cancer type, its stage, and the patient’s health.
Survival Rates for BCC
Basal cell carcinoma has a good prognosis. It grows slowly and rarely spreads. Early detection makes it highly treatable, with cure rates over 90%.
|
Treatment Method |
Cure Rate |
|---|---|
|
Surgical Excision |
95% |
|
Mohs Surgery |
99% |
Survival Rates for SCC
Squamous cell carcinoma is also treatable but has a higher risk of spreading. The prognosis depends on the stage and any high-risk features.
Early-stage SCC has a high cure rate with treatments like surgical excision or Mohs surgery.
|
Stage at Diagnosis |
5-Year Survival Rate |
|---|---|
|
Localized |
95% |
|
Regional |
70% |
|
Distant |
40% |
Recurrence Risks and Follow-up Care
Both BCC and SCC can come back if not treated right. Regular check-ups are crucial to catch any new cancers early.
Follow-up recommendations include skin exams every 6 to 12 months for a few years. The visits can be less often if there’s no sign of cancer.
By knowing the prognosis and following up, patients can improve their outcomes. This helps lower the chance of cancer coming back.
Prevention Strategies for Skin Cancer
We can fight skin cancer with sun protection, self-checks, and healthy living. Knowing and using these steps can lower our risk of skin cancer a lot.
Sun Protection Best Practices
Keeping our skin safe from the sun’s UV rays is key. Here are some top tips for sun protection:
- Use broad-spectrum sunscreen with SPF 30 or higher
- Stay in the shade, especially from 10 am to 4 pm
- Wear clothes that cover you, like hats and sunglasses that block UV
- Stay away from tanning beds and artificial UV light
Regular Skin Self-Examinations
Checking your skin often is important for catching skin cancer early. Here’s how to do it:
- Check your skin every month for new moles or changes
- Use the ABCDE rule to spot possible cancer signs (Asymmetry, Border, Color, Diameter, Evolving)
- See a dermatologist if you find anything odd
Lifestyle Modifications and Preventive Measures
There are more ways to lower your skin cancer risk besides sun protection and self-checks. Here are some:
|
Lifestyle Change |
Benefit |
|---|---|
|
Don’t smoke or use tobacco |
It lowers your risk of all cancers, including skin cancer |
|
Eat a diet full of fruits, veggies, and omega-3s |
It helps keep your skin healthy and boosts your immune system |
|
Drink plenty of water and manage stress |
It helps your body fix and protect your skin cells better |
By adding these prevention steps to our daily lives, we can greatly reduce skin cancer cases.
Conclusion
It’s important to know the difference between Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC) for good skin cancer care. We’ve covered the basics of skin cancer, the traits of BCC and SCC, and their unique features.
BCC and SCC are the top two kinds of skin cancer, each with its own cell type, growth style, and chance of spreading. Catching them early and preventing them is key to treating them well. We stress the need for sun protection, checking your skin regularly, and making healthy lifestyle choices to lower your risk.
In short, knowing about BCC and SCC is vital for skin cancer management. By grasping the differences between these two, as we’ve explained, people can handle skin cancer diagnosis and treatment better. We urge readers to protect their skin and see a doctor if they spot anything unusual.
FAQ
What is the difference between basal cell carcinoma (BCC) and squamous cell carcinoma (SCC)?
BCC and SCC are both skin cancers. BCC comes from basal cells and grows slowly. It rarely spreads. SCC comes from squamous cells, grows faster, and can spread more.
What are the common characteristics and appearance of BCC?
BCC looks like a shiny, pearly bump or a flat, flesh-colored spot. It can also be a pink or red patch. You usually find it on sun-exposed areas like the face and ears.
Where does SCC typically develop?
SCC often shows up on sun-exposed spots like the face and hands. It can also appear on the scalp, neck, and forearms.
What are the risk factors for developing BCC and SCC?
UV exposure, genetics, and lifestyle choices like smoking increase your risk. People with fair skin and a history of sunburns are at higher risk.
How are BCC and SCC diagnosed?
Doctors first look and then take a biopsy to confirm cancer. They might use dermoscopy for more detailed checks.
What are the treatment approaches for BCC?
BCC can be treated with surgery, Mohs surgery, cryotherapy, or topical treatments. The choice depends on the tumor’s size, location, and the patient’s health.
How is SCC treated?
SCC treatment includes surgery and sometimes radiation or systemic therapies. For high-risk SCC, a detailed care plan is needed.
What are the warning signs for BCC and SCC?
Look out for new growths, sores that don’t heal, and skin texture or color changes. If you notice anything unusual, see a doctor.
What is the prognosis for BCC and SCC?
BCC has a good prognosis if caught early. SCC also has a good chance of being cured if treated quickly. But, SCC can spread if not treated.
How can skin cancer be prevented?
Prevent skin cancer by protecting your skin from the sun, doing skin checks, and avoiding smoking. Limit UV exposure too.
What is the importance of follow-up care for BCC and SCC?
Regular check-ups are key to catch any new cancers early. This is especially important for those with a history of skin cancer.
What is a blind carbon copy (BCC) in email communication?
A BCC in email lets the sender add recipients without showing their emails. It’s used to keep recipients’ privacy and avoid reply-all messages.
What is the role of melanocytes in skin cancer?
Melanocytes produce melanin, the skin’s pigment. They’re not directly linked to BCC or SCC but play a role in melanoma.
What is keratoacanthoma?
Keratoacanthoma is a skin growth that looks like SCC. It grows fast, then stays stable, and might go away. It’s hard to tell apart from SCC but is considered different.
What is the meaning of “in situ” in the context of skin cancer?
“In situ” means cancer that only affects the skin’s outer layer. It’s used to describe early-stage skin cancers like carcinoma in situ.
What is the epidermis, and how is it related to skin cancer?
The epidermis is the skin’s outer layer. Skin cancer usually starts here. Knowing about the epidermis helps understand skin cancer’s development and growth.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20231424/










