Autologous cell therapies face big hurdles, like complex logistics and high costs. The process is detailed, from collecting cells to making and delivering them. This complexity contributes to the high expenses associated with the process.
The demand for autologous cell therapy is rising. Despite these challenges, the need for solutions is growing.
At Liv Hospital, we aim to lead in top-notch, ethical healthcare. We know the high costs, from $373,000 to $4.25 million, are a big problem. They make it hard for patients to get these treatments.
Key Takeaways
- Autologous cell therapy involves complex logistics and multiple steps.
- The high cost of autologous cell therapies limits patient access.
- Manufacturing risks are a significant challenge in autologous cell therapy.
- The market for autologous cell therapy is expected to grow significantly.
- Overcoming the challenges of autologous cell therapy is key for success.
The Science Behind Autologous Cell Therapy
Autologous cell therapy uses a patient’s own cells to treat diseases. It’s a new way to fight complex health issues. This method is safe because it doesn’t cause rejection or bad reactions.
Definition and Fundamental Mechanisms
This therapy takes a patient’s cells, changes them, and puts them back in. It helps the body heal itself better.
It works because some cells can grow back or change the immune system. For example, stem cells can turn into different types of cells. This helps fix damaged tissues.
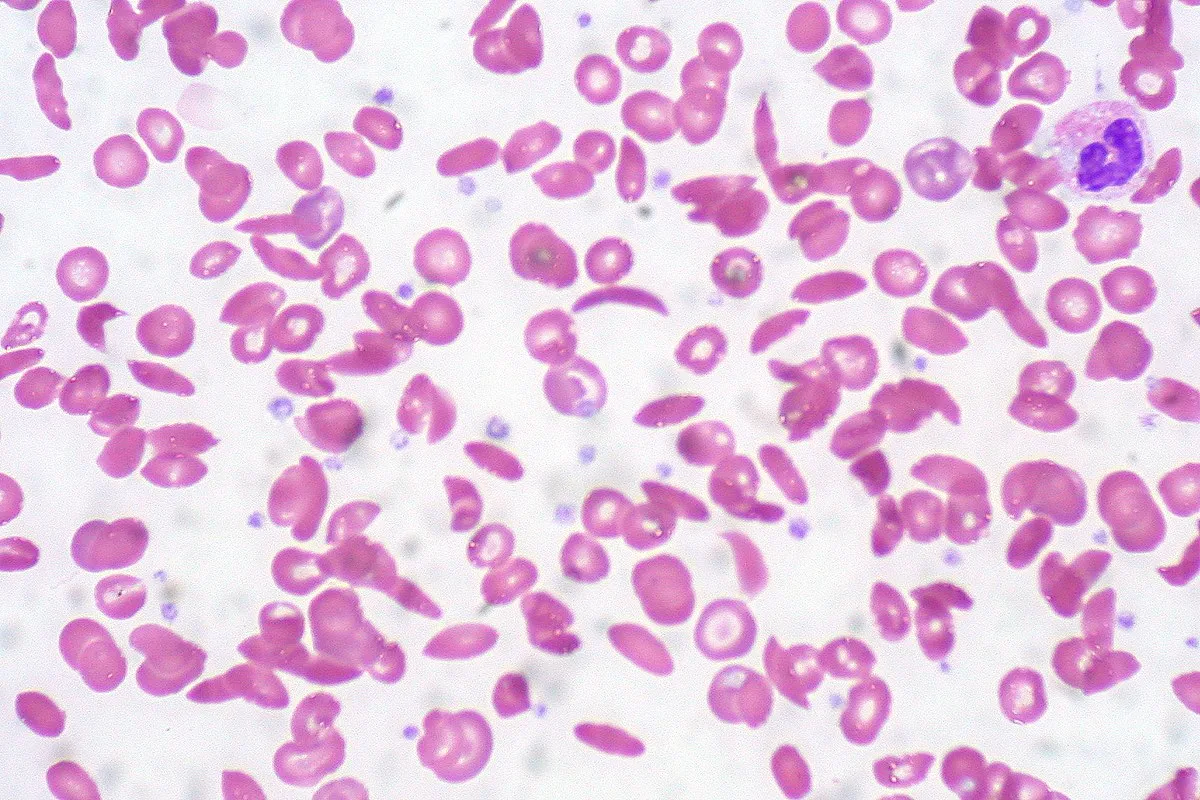
Types of Cells Used in Treatment
Many types of cells are used in this therapy. Stem cells from bone marrow or fat are common. Also, cells from menstrual blood can help with women’s health issues.
Historical Development and Milestones
Autologous cell therapy started with bone marrow transplantation. This has been around for decades. New ways to get, grow, and change cells have made it better.
A big step was CAR-T cell therapy. It changed how we treat some cancers.
Autologous vs Allogeneic Cell Therapies: A Comparative Look
Understanding the differences between autologous and allogeneic cell therapies is key in regenerative medicine. We will look at their unique traits, benefits, and drawbacks.
Source Material and Donor Considerations
Autologous cell therapy uses a patient’s own cells. These cells are taken, processed, and given back to the same person. This method avoids immune rejection and disease transmission from donors.
Allogeneic cell therapy, on the other hand, uses donor cells. This can be more affordable and accessible. But, it needs careful donor screening and matching to avoid immune reactions.
A study on shows the importance of choosing the right donor and cell source.
|
Characteristics |
Autologous Cell Therapy |
Allogeneic Cell Therapy |
|---|---|---|
|
Source Material |
Patient’s own cells |
Donor cells |
|
Immune Rejection Risk |
Low |
Moderate to High |
|
Availability |
Limited by patient’s condition |
More readily available |
Immunological Advantages and Limitations
Autologous cell therapy has a big advantage: it’s immunologically compatible. This means the cells are from the patient, lowering the risk of GVHD. Allogeneic cell therapy, while more scalable, faces a higher risk of immune rejection and GVHD. Researchers are working on making allogeneic cells less likely to trigger an immune response.
Manufacturing Complexity Differences
Autologous cell therapies are highly personalized. They involve collecting, processing, and giving back a patient’s cells. This makes production complex and costly.
Allogeneic cell therapies, on the other hand, can be made in larger quantities. This could lower costs. But, they need strict quality control to ensure consistency.
Treatment Timeline and Patient Experience
Autologous cell therapies take longer because of the personalized process. This delay can affect patient outcomes, mainly for those with fast-moving diseases. Allogeneic cell therapies offer a quicker option. But, the need for immunosuppression to prevent rejection can make the patient’s experience more complicated.
In conclusion, both autologous and allogeneic cell therapies have their own benefits and challenges. As research progresses, we might see new approaches that combine the best of both.
Logistical Challenges in the Autologous Supply Chain
The success of autologous cell therapy relies on solving complex logistical challenges. It involves many players, like collection centers, manufacturing sites, and treatment locations. This makes the process very complex.
Chain of Identity and Custody Requirements
Keeping the chain of identity intact is key in autologous cell therapy. It means keeping accurate records and making sure the cells from a patient are the same ones given back. Chain of custody is about safely handling and storing these cells.
We need strong tracking systems and secure storage places. This keeps patients safe and the therapy effective.
Transportation Constraints and Cold Chain Management
Getting cells from collection centers to manufacturing and treatment sites is tough. Keeping the cold chain is vital to keep cells alive. This needs special transport gear and constant checks.
There are also transportation constraints like following rules, delivering on time, and handling biological stuff. Good cold chain management stops cell damage and keeps therapy working.
Coordination Between Collection, Manufacturing, and Treatment Sites
Working well together is essential for autologous cell therapy success. It’s about scheduling collection, making, and treatment right. This ensures therapy is given on time.
We must have clear communication and teamwork between sites. This means sharing updates on cell collection, making progress, and any transport problems.
By tackling these challenges, we can make the autologous supply chain better. This will lead to better results for patients.
Manufacturing Complexities and Quality Control
Autologous cell therapy manufacturing is a complex process. It needs strict quality assurance protocols. From cell harvesting to final product, each step must be controlled precisely. This ensures the therapy’s safety and effectiveness.
Current Failure Rates and Root Causes
The failure rate for autologous cell therapy manufacturing is 5-10%. Identifying the root causes of these failures is key to improving the process. Issues include contamination, cell quality variability, and equipment malfunctions.
To tackle these problems, we need to implement robust quality control measures at every production stage. This includes:
- Stringent donor screening and cell handling practices
- Advanced bioreactor technologies to minimize contamination risk
- Regular maintenance and calibration of equipment
GMP Compliance in Personalized Medicine
Ensuring Good Manufacturing Practice (GMP) compliance is vital for autologous cell therapies. GMP guidelines help maintain therapy quality, safety, and efficacy.
We must adapt GMP guidelines for personalized therapies. This involves:
- Tailoring production processes to individual patient needs
- Maintaining flexibility in manufacturing while adhering to GMP standards
- Implementing advanced tracking and tracing systems for personalized products
Scaling Challenges for Individual Patient Production
Scaling autologous cell therapy production for individual patients is challenging. Each patient’s cells need a customized process, making large-scale production complex.
To overcome these challenges, we are exploring innovative manufacturing technologies. These aim to scale production efficiently while keeping product quality high.
Quality Assurance for Biological Variability
Biological variability is a big challenge in autologous cell therapies. Each patient’s cells are unique, making consistent quality hard to achieve.
We are developing advanced quality assurance protocols to handle this variability. This includes:
- Comprehensive characterization of cell products
- Robust in-process controls to monitor product quality
- Release testing that accounts for biological variability
The Economic Burden: Cost Analysis of Autologous Therapies
Autologous therapies are groundbreaking but expensive. They cost a lot, making it hard for patients to get them. Prices can go from $373,000 to $4.25 million.
Price Range Breakdown
The cost of autologous therapies varies a lot. This is because treatments are complex and different for everyone. For example, treatments using hematopoietic stem cells can cost a lot, depending on the treatment and patient needs.
Many things affect the cost. These include the type of cells, how the treatment is made, and how it’s tailored for each patient. This makes the cost high for both patients and healthcare systems.
Cost Drivers in the Production Process
Several factors make autologous therapies expensive. These include:
- The need for personalized manufacturing processes, which increases production costs.
- The complexity of quality control measures to ensure safety and efficacy.
- The requirement for specialized facilities and skilled personnel.
A recent article on to autologous cell and gene therapies highlights these issues. These factors make it hard to make these therapies more affordable.
Economic Sustainability Challenges
The high cost of autologous therapies is a big worry. Healthcare systems and payers are finding it tough to provide these treatments while keeping costs down.
To solve this, we need to find ways to lower costs without sacrificing quality or safety. Improving manufacturing processes and investing in new technologies could help make these therapies more affordable.
Patient Access Barriers and Healthcare System Integration
Ensuring everyone can get autologous therapies is a big challenge. We need to fix patient access barriers and make healthcare systems work better together. It’s hard to make these therapies available to everyone who needs them.
Insurance Coverage and Reimbursement Obstacles
Getting autologous cell therapies can be tough because of insurance issues. Insurance companies have different rules for covering these therapies. This makes it hard for patients to get the treatments they need without spending a lot of money.
The process of getting reimbursed for these therapies is also a problem. It can take a long time to get approval. This delay can hurt patient outcomes. We need to make the reimbursement process easier and faster.
Geographic Limitations and Treatment Center Distribution
Not enough treatment centers offer autologous cell therapies. Many patients have to travel far to get these treatments. This is really hard for people with serious illnesses or mobility issues. We should find ways to bring more treatment centers to patients or offer other care options.
Being far from treatment centers is not just a travel issue. It also leads to unfair healthcare outcomes. By fixing this, we can make healthcare fairer for everyone.
Socioeconomic Disparities in Access
Socioeconomic status affects who can get autologous therapies. People with less money often face more barriers. They might not have insurance, know about the treatments, or have access to healthcare. We need to find ways to help these patients get the treatments they need.
By tackling these disparities, we can make healthcare more inclusive. This way, everyone, no matter their background, can get the advanced therapies they need.
Clinical Challenges: Efficacy Data and Outcome Measurement
Autologous cell therapy faces big challenges in getting strong evidence and standardizing how we measure results. It’s key to tackle these issues to make sure these treatments work well in the long run.
Evidence Limitations for Payer Decision-Making
The lack of solid evidence makes it hard for payers to decide on coverage. Payers need strong data to make smart choices. Without enough evidence, good treatments might not get used much, which limits patients’ access to life-changing therapies.
A study in a top medical journal pointed out that the evidence for autologous cell therapies is often scattered and not consistent. This makes it tough for payers to really understand their value. We need better, more complete research to help payers make good choices.
|
Evidence Type |
Description |
Impact on Payer Decision-Making |
|---|---|---|
|
Randomized Controlled Trials (RCTs) |
High-quality evidence comparing treatment outcomes |
High confidence in treatment efficacy |
|
Observational Studies |
Real-world data on treatment outcomes |
Moderate confidence, may be influenced by biases |
|
Case Series |
Limited data on small patient groups |
Limited confidence, often considered preliminary evidence |
Long-term Follow-up Complexities
Following patients for a long time is key to knowing if autologous cell therapies are safe and work well over time. But, it’s hard to keep track of patients for a long time and collect data. Creating strong follow-up plans is key to getting useful long-term data.
“Long-term follow-up is not just about monitoring adverse events; it’s about understanding the therapy’s impact on patients’ quality of life and functional outcomes over time.”
Standardizing Outcome Metrics Across Patients
It’s hard to standardize how we measure results in autologous cell therapy. Different patients and diseases make it tough to find common metrics. Creating and using the same outcome measures will help compare studies and patients better.
Researchers are looking into using core outcome sets (COS) to define the essential data to collect in trials. This way, studies can be more alike and the data collected will be more useful and meaningful.
By tackling these challenges, we can make autologous cell therapies more effective and safe. This will lead to better results for patients. As we keep moving forward, it’s important to keep investing in research and development to overcome these obstacles and unlock the full promise of these new treatments.
Process-Related Complications and Treatment Delays
The process of autologous cell therapy can face many challenges. These include delays in manufacturing and changes in product quality. These problems can affect how well and safely the treatment works.
Impact of Manufacturing Delays on Patient Outcomes
Delays in making autologous cell therapy can harm patients. If the production slows down or stops, patients might not get their treatment on time. This can make their condition worse.
Delays can happen for many reasons. These include:
- Complex production processes
- Limited manufacturing capacity
- Stringent quality control measures
Cell Viability and Potency Challenges
Keeping cells alive and strong is key for autologous cell therapy to work. Problems in keeping cells alive during making can lower the treatment’s success.
We use special cell handling methods and strict quality checks. This helps make sure the cells stay alive and effective.
“The ability to maintain cell viability is critical for the success of autologous cell therapy.”
Expert Opinion
Product Quality Variability and Clinical Implications
Changes in product quality can greatly affect treatment safety and success. These changes can come from different patient materials, making processes, and storage conditions.
To reduce these risks, we have strong quality assurance steps. These include:
- Standardized manufacturing protocols
- Regular quality control checks
- Comprehensive product testing
By tackling these issues, we can make autologous cell therapy better and safer. This will help improve patient results.
Regulatory Hurdles and Compliance Requirements
Understanding regulatory hurdles is key for autologous cell therapies to succeed. As we improve these therapies, it’s vital to follow rules for their safety and use.
FDA Approval Pathways for Cellular Therapies
The FDA has set up special ways to approve cellular therapies, like autologous cell therapies. These paths help make sure these treatments are safe and work well. They also help get these treatments to patients faster.
- Investigational New Drug (IND) Application: Needed before starting clinical trials. It shares details on the therapy, how it’s made, and early test results.
- Biologics License Application (BLA): A detailed application for market approval. It includes trial data, how it’s made, and labeling.
- Regenerative Medicine Advanced Therapy (RMAT) Designation: The FDA’s fast-track for regenerative medicine, including autologous cell therapies.
International Regulatory Frameworks
Rules for autologous cell therapies differ worldwide, making global development and use tricky. Key points include:
- Different rules in each country and area.
- The importance of international guidelines and working together.
- The hard part of following many rules at once.
Knowing these differences is essential for companies wanting to sell these therapies worldwide.
Post-Market Surveillance Challenges
After approval, autologous cell therapies need constant checks to stay safe and effective. Challenges include:
- Keeping track of long-term results in a wide range of patients.
- Handling the complexity of collecting and analyzing data.
- Keeping up with changing rules.
Good post-market surveillance is key for keeping public trust and the long-term success of these treatments.
In summary, tackling regulatory hurdles and following rules is a big challenge in making autologous cell therapies. By understanding and dealing with these issues, we can make these new treatments available to more people.
Technological Innovations Addressing Current Limitations
The field of autologous cell therapy is on the verge of a big change. New technologies are helping to solve its problems. These advancements are key to overcoming the challenges we face today.
Automation in Cell Processing and Manufacturing
Automation is a big step forward in autologous cell therapy. Automated systems make the production process smoother. They cut down on mistakes and make things more efficient.
For example, tools that count and check cells quickly are important. They help make sure the cells are good to use.
These systems also make it easier to make more cells. This means we can treat more people without losing the personal touch.
Closed-System Bioreactors and Contamination Control
Closed-system bioreactors are another big innovation. They help keep cells safe from contamination. This is because they create a clean space for cells to grow.
- Improved sterility and reduced risk of contamination
- Enhanced control over cell culture conditions
- Increased efficiency in cell expansion and culture
Digital Solutions for Chain of Identity
Digital solutions help keep track of cells during production. They use things like RFID and barcodes to follow cells in real-time. This makes things safer and easier to track.
Some companies are even using blockchain technology. This creates a permanent record of how the cells were made. It makes sure the product is real and trustworthy.
Point-of-Care Manufacturing Developments
New point-of-care manufacturing technologies are changing how we make cell therapies. They let us make treatments right where they’re needed. This cuts down on the time it takes to get treatments to patients.
These technologies make treatments more accessible. They bring the manufacturing process closer to the patient. This could be a game-changer for how we deliver cell therapies.
Market Dynamics and Growth Projections
Understanding the cell therapy market is key for all involved. The autologous cell therapy market is changing fast. This is due to new tech, rules, and what patients need.
Current Market Size and Segmentation
The autologous cell therapy market is big and getting bigger. It’s expected to hit $5.51 billion by 2025. This growth comes from more people wanting personalized medicine and new cell therapy tech.
|
Segment |
2025 Projection ($ Billion) |
Market Share (%) |
|---|---|---|
|
Oncology |
2.5 |
45 |
|
Cardiovascular Diseases |
1.2 |
22 |
|
Orthopedic |
0.8 |
15 |
|
Others |
1.01 |
18 |
Growth Forecast and Investment Trends
The autologous cell therapy market is set to grow a lot. It’s expected to reach $22.3 billion by 2032. This is a 22% annual growth rate. Investors are pouring money into new cell therapy startups.
Several things are driving this growth:
- More people getting chronic diseases
- New gene editing and cell processing tech
- More demand for treatments tailored to each person
- New therapies getting approved by regulators
Competitive Landscape and Industry Consolidation
The autologous cell therapy market is very competitive. It has everything from small biotechs to big pharma. The market is full of:
- Intense R&D efforts
- Partnerships and collaborations
- Mergers and acquisitions
- More focus on making products cheaper and better
Big companies are likely to keep buying smaller ones. This helps them grow their product lines and skills.
Ethical Considerations in Personalized Cell Therapy
Personalized medical treatments are changing the field of cell therapy. As we move forward, we must tackle the ethical issues that come with these new treatments.
Patient Consent and Expectation Management
Ensuring patients understand and agree to treatments is key. Patient consent must be given after explaining the benefits and risks. It’s also important to manage what patients expect, as results can vary.
For example, looking ahead to , we must balance hope with realistic expectations about availability and effectiveness.
Resource Allocation and Healthcare Priorities
Deciding how to use healthcare resources is another big issue. Autologous cell therapies are costly and require a lot of resources. Resource allocation must weigh clinical benefits against costs and system impact.
- Comparing the costs of autologous vs. allogeneic cell therapies
- Looking at the infrastructure needed for widespread use
- Thinking about the fairness of limiting access to pricey treatments
Equity in Access to Advanced Therapies
Ensuring fair access to advanced therapies like autologous cell therapy is vital. Disparities in access can be due to location, money, and insurance. We must work to reduce these gaps so everyone can benefit from cell therapy.
“The true measure of a society is how it treats its most vulnerable members.” This quote highlights the need for fair access to treatments like autologous cell therapy.
Conclusion: Balancing Challenges and Promise in Autologous Cell Therapy
Autologous cell therapy has shown great promise in treating many diseases. But, we must face the challenges it brings. We’ve looked into the science, the practical issues, and the rules that govern it.
Comparing autologous and allogeneic cell therapies shows their unique strengths and weaknesses. Autologous therapy offers personalized care but faces complex manufacturing and high costs.
To beat these hurdles, we need new tech. Things like automated cell processing and digital tracking can help. This way, we can make autologous cell therapy more available and effective.
Looking ahead, we must weigh the good and bad of autologous cell therapy. We should keep funding research, improve how we make it, and tackle regulatory issues. This will help us fully use this groundbreaking treatment.
FAQ
What is autologous cell therapy?
Autologous cell therapy uses a patient’s own cells. These cells are then treated and put back into the patient. It’s used to treat diseases like cancer and gynecological disorders.
How does autologous cell therapy differ from allogeneic cell therapy?
Autologous cell therapy uses the patient’s own cells. Allogeneic cell therapy uses cells from another person. This affects the source, immune issues, and how it’s made.
What are the main challenges in manufacturing autologous cell therapies?
Making autologous cell therapies is hard. It involves many steps and needs strict quality control. Ensuring it meets GMP standards, scaling for each patient, and dealing with biological differences are key.
What is the cost range for autologous cell therapies?
Autologous cell therapies can cost between $373,000 and $4.25 million. This makes them a big financial burden for patients and healthcare systems.
What are the main patient access barriers to autologous cell therapies?
Getting access to autologous cell therapies is hard. Insurance and reimbursement issues, location, and money problems are big barriers. These need to be fixed for fair access.
What are the clinical challenges associated with autologous cell therapies?
There are big challenges in using autologous cell therapies. Limited evidence, long-term follow-up, and standardizing results are issues. These need to be solved for success.
How can process-related complications be mitigated in autologous cell therapies?
Complications like delays, cell issues, and quality problems can be fixed. This can be done by improving quality control and making manufacturing better.
What are the regulatory hurdles for autologous cell therapies?
There are big hurdles in getting autologous cell therapies approved. FDA rules, international laws, and keeping an eye on them after approval are challenges. These need to be overcome for success.
How are technological innovations addressing the limitations of autologous cell therapies?
New tech like automation and digital solutions is helping. These advancements aim to solve current problems in autologous cell therapy.
What are the ethical considerations in personalized cell therapy?
Ethical issues like consent, fairness, and access are important. These need to be handled carefully to ensure responsible use of autologous cell therapies.
What is the current market size and growth projection for autologous cell therapies?
The market is growing fast. It’s expected to go from $5.51 billion in 2025 to $22.3 billion by 2032. This growth is driven by more demand and investment.
What is the significance of immunotherapy in autologous cell therapy?
Immunotherapy is key in autologous cell therapy. It uses the patient’s immune cells to fight diseases, like cancer.
How does stem cell transplantation relate to autologous cell therapy?
Stem cell transplantation is a type of autologous cell therapy. It uses the patient’s stem cells to replace damaged cells. It’s used for some cancers and blood disorders.
What is the role of hematopoietic stem cells in autologous cell therapy?
Hematopoietic stem cells are used in autologous cell therapy. They help treat blood disorders, like leukemia and lymphoma.
References:
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC12022644/