Last Updated on October 21, 2025 by mcelik

Did you know that sickle cell disease affects millions worldwide, causing significant health challenges? It’s a genetic disorder that impacts hemoglobin production in red blood cells. This leads to abnormally shaped red blood cells that can’t transport oxygen effectively.
Understanding the risk factors and traits associated with sickle cell disease is key for early diagnosis and management. This condition is inherited, passed down from parents to their children through genes. If you’re a carrier of the sickle cell trait, there’s a chance your child could inherit the disease.
So, what is sickle cell disease, and who is at risk? It’s vital to grasp the genetic basis of the disease to spot those who may be affected. By knowing the risk factors, we can strive for better management and care for those with sickle cell anemia.
Key Takeaways
- Sickle cell disease is a genetic disorder affecting hemoglobin production.
- The disease is inherited, and carriers of the sickle cell trait are at risk of passing it to their children.
- Understanding risk factors and traits is vital for early diagnosis and management.
- Identifying those at risk can help in providing better care and management for individuals with sickle cell disease.
- Knowing the genetic basis of the disease is key to understanding who may be affected.
Understanding Sickle Cell Disease: A Blood Disorder Overview
To understand sickle cell disease, we must look at its causes. This includes the role of abnormal hemoglobin. It’s a genetic disorder that affects how red blood cells make hemoglobin, leading to sickle-shaped cells.
The Science Behind Abnormal Hemoglobin
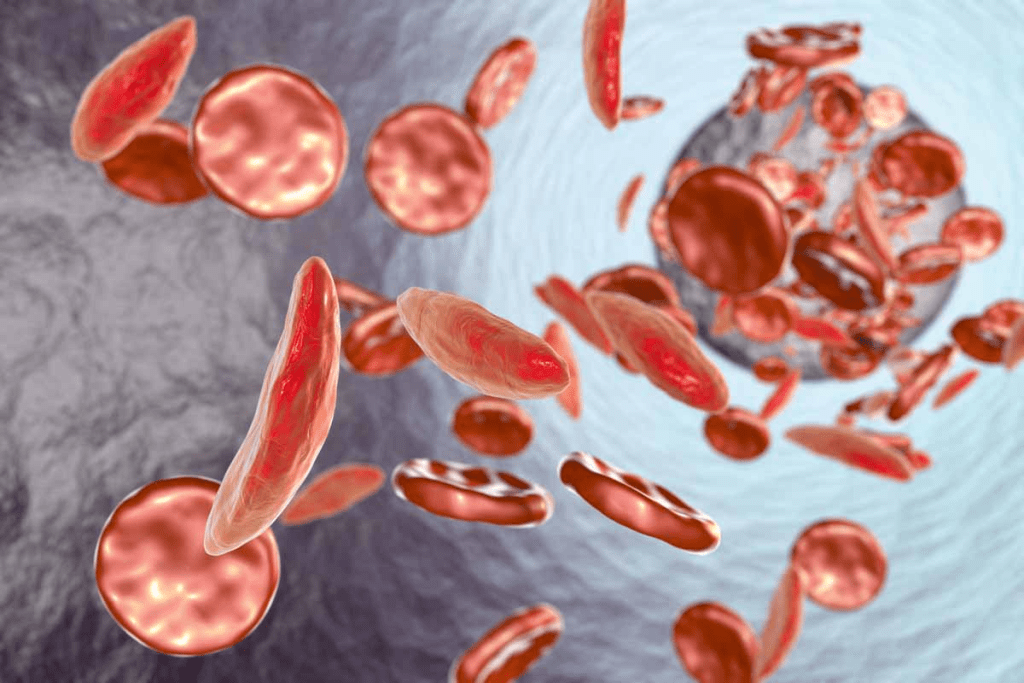
Abnormal hemoglobin is key to sickle cell disease. It comes from a gene mutation in the HBB gene. This mutation makes hemoglobin S (HbS), which changes shape under low oxygen, making red blood cells sickle-shaped.
This shape change makes cells less flexible. They can’t move well through blood vessels. This affects blood flow and oxygen delivery to tissues.
How Sickle-Shaped Cells Affect Blood Flow
Sickle-shaped red blood cells are stiff and can get stuck in small blood vessels. This can cause vaso-occlusive crises. These crises block blood flow to certain areas, causing pain and potentially harming organs over time.
Less blood flow means less oxygen for tissues. This makes health issues from sickle cell disease worse.
Differentiating Between Sickle Cell Disease and Sickle Cell Trait
It’s important to know the difference between sickle cell disease and sickle cell trait. People with sickle cell trait have one normal and one mutated HBB gene. They are carriers but usually don’t have the full disease.
But, carriers can face health problems under certain conditions. There’s also a chance they can pass the mutated gene to their kids. These kids might get sickle cell disease if they get two mutated genes.
The Genetic Basis of Sickle Cell Disease
Understanding sickle cell disease’s genetic basis is key. It shows how the condition is passed down and appears. The disease is caused by a change in the HBB gene. This gene codes for a part of hemoglobin.
This change leads to abnormal hemoglobin, known as sickle hemoglobin or HbS. This is what causes the disease.
The HbS Gene Mutation
The HbS gene mutation is a specific change in the HBB gene. It replaces glutamic acid with valine at the sixth position. This change makes hemoglobin turn into a sickle shape when oxygen levels are low.
This is the main reason for sickle cell disease.
Autosomal Recessive Inheritance Pattern
Sickle cell disease follows an autosomal recessive pattern. This means a person needs two copies of the mutated HBB gene to have the disease. One copy comes from each parent.
Carriers have one normal and one mutated gene. They usually don’t show the disease’s full symptoms. But they can pass the mutated gene to their children.
This pattern is important for family planning and genetic counseling. It helps predict the risk of passing the disease to future generations.
Genetic Variations and Their Impact
While the HbS mutation is the main cause, other genetic changes can affect the disease’s severity. For example, having other hemoglobinopathies like beta-thalassemia can lead to different forms of sickle cell disease.
Genetic changes can also impact fetal hemoglobin production. This can help reduce some symptoms of sickle cell disease. Knowing about these variations is vital for treating the disease effectively.
| Genetic Variation | Effect on Sickle Cell Disease |
| HbS Mutation | Causes sickle cell disease |
| Beta-Thalassemia | Can result in HbS-beta-thalassemia, a variant of sickle cell disease |
| Fetal Hemoglobin Production | Can mitigate some symptoms of sickle cell disease |
Sickle Cell Disease Traits: Carriers vs. Those With the Disease
Sickle cell trait and sickle cell disease are different. People with sickle cell trait are usually healthy. But they can pass the mutated gene to their kids.
What It Means to Have Sickle Cell Trait
Having sickle cell trait means you carry the sickle cell gene. You have one normal and one mutated hemoglobin gene. People with this trait usually don’t show sickle cell disease symptoms but can pass it to their kids.
Key aspects of being a carrier include:
- Generally, carriers are healthy and lead normal lives.
- They can pass the sickle cell gene to their offspring.
- In rare cases, extreme physical conditions can lead to complications.
Carrier Status and Health Implications
Being a carrier of the sickle cell trait has health implications. Most carriers are healthy and don’t show symptoms. But, extreme physical exertion or high altitudes can cause problems.
Health implications for carriers can include:
- Increased risk of dehydration during intense exercise.
- Potential for kidney problems or issues related to blood concentration.
- Rare instances of splenic infarction at high altitudes.
When Traits Lead to Disease
The sickle cell trait can turn into sickle cell disease in children if both parents are carriers. If both parents carry the trait, there’s a 25% chance each child will have the disease.
Understanding the risk:
- If both parents are carriers, there’s a 25% chance a child will have sickle cell disease.
- There’s a 50% chance a child will be a carrier like the parents.
- And a 25% chance a child will neither have the disease nor be a carrier.
Inheritance Patterns and Risk of Transmission
It’s important to know how sickle cell disease is passed down in families. This disease follows an autosomal recessive pattern. This means a person needs two abnormal hemoglobin genes, one from each parent, to have the disease.
Parent-to-Child Transmission Probabilities
When both parents carry the sickle cell trait, there are certain chances for each child. There’s a 25% chance the child will get two normal genes. A 50% chance they’ll get one normal and one sickle cell gene, making them a carrier. And a 25% chance they’ll get two sickle cell genes, leading to sickle cell disease.
Let’s look at the chances of being normal, a carrier, or having sickle cell disease when both parents are carriers:
- 25% chance of being normal (not a carrier): Getting two normal hemoglobin genes.
- 50% chance of being a carrier: Getting one normal and one sickle cell gene.
- 25% chance of having sickle cell disease: Getting two sickle cell genes.
Genetic Counseling for At-Risk Couples
For couples where both are carriers, getting genetic counseling is a good idea. Counselors can explain the risks of each pregnancy. They can also talk about testing options and help with family planning decisions.
Genetic counseling covers a few key points:
- Assessing the risk of passing on sickle cell disease to offspring.
- Discussing the implications of being a carrier or having the disease.
- Exploring available reproductive options, including prenatal testing.
Family Planning Considerations
Knowing the genetic risks can affect family planning choices. At-risk couples might look into:
- Prenatal testing to see if the fetus has sickle cell disease.
- Preimplantation genetic diagnosis (PGD) during IVF procedures.
- Adoption.
It’s key for at-risk couples to talk to a healthcare provider or genetic counselor. This way, they can make choices that fit their needs.
Demographic Distribution: Who Is Most Affected?
It’s important to know who gets sickle cell disease to help them better. This disease changes how red blood cells work. It’s more common in some groups because of history and genes.
Prevalence in African and African American Populations
In the U.S., 1 in 500 African Americans has sickle cell disease. It’s also common in the Caribbean and parts of Central and South America. This is because of history and genetics.
The sickle cell trait helps protect against malaria. This was important in areas where malaria was common.
Sickle Cell Disease in Mediterranean, Middle Eastern, and Indian Populations
Sickle cell disease isn’t just in Africa. It also affects people in the Mediterranean, Middle East, and India. In places like Greece and Turkey, it’s more common in certain groups.
In India, it’s found in some tribal communities. It’s a big health issue there, where getting care can be hard.
Global Distribution and Migration Patterns
Migration has spread sickle cell disease worldwide. People moving carried the genes with them. This has brought the disease to new places, like North America and Europe.
Knowing where the disease is helps doctors plan better. They can focus on helping those most affected, providing the right care and support.
The Evolutionary Advantage: Malaria Protection
The sickle cell trait offers a special advantage, mainly in areas with lots of malaria. This benefit is linked to its ability to fight off malaria. Malaria has long been a big problem in many parts of the world.
Protection Against Malaria
The sickle cell trait helps protect against malaria. The malaria parasite finds it hard to survive in red blood cells with sickle hemoglobin. This protection is not absolute, but it greatly lowers the risk of severe malaria. This gives people with the trait a better chance of surviving in areas where malaria is common.
Geographic Correlation with Malaria-Endemic Regions
There’s a clear link between the sickle cell trait and places where malaria used to be common. In places like sub-Saharan Africa, the Mediterranean, and parts of the Middle East and India, more people have the trait. This shows how the trait helps protect against malaria in these areas.
| Region | Prevalence of Sickle Cell Trait | Malaria Endemicity |
| Sub-Saharan Africa | High | Historically high |
| Mediterranean | Moderate | Historically moderate |
| Middle East | Variable | Historically variable |
| India | Variable | Historically variable |
The Balance Between Protection and Disease
The sickle cell trait protects against malaria but also increases the risk of sickle cell disease in children. This creates a delicate balance between the benefits and risks of the trait. Understanding this balance is key to grasping the genetics and spread of sickle cell disease.
In summary, the sickle cell trait’s protection against malaria is a big plus in areas with lots of malaria. But, it also means there’s a chance of sickle cell disease in kids. This shows why genetic counseling and awareness are so important.
Types of Sickle Cell Disease and Their Prevalence
Sickle cell disease comes in several types, each with its own genetic traits and severity levels. Knowing these differences is key for diagnosis, treatment, and genetic advice.
Hemoglobin SS (Sickle Cell Anemia)
Hemoglobin SS, or sickle cell anemia, is the most common and severe form. It happens when someone gets two HbS genes, one from each parent. This leads to sickle-shaped red blood cells under certain conditions.
Prevalence: Sickle cell anemia is widespread in sub-Saharan Africa. It also affects many African Americans and people from Mediterranean, Middle Eastern, and Indian backgrounds.
Hemoglobin SC Disease
Hemoglobin SC disease comes from one HbS and one HbC gene. It’s milder than sickle cell anemia but shares some traits.
Prevalence: It’s common in West Africa. It’s also found in areas where sickle cell trait is common.
Hemoglobin S Beta Thalassemia
Hemoglobin S beta thalassemia happens with one HbS and one beta thalassemia gene. Its severity varies based on the beta thalassemia mutation.
Prevalence: Its prevalence depends on the HbS and beta thalassemia gene frequencies. It’s seen in Africa, the Mediterranean, and the Middle East where these genes are common.
Rarer Forms of Sickle Cell Disease
There are rarer forms like Hemoglobin SD, SE, and others. These result from the HbS gene mixing with other abnormal hemoglobin genes.
Prevalence: These rarer forms are less common. Their prevalence varies by region and ethnicity.
| Type of Sickle Cell Disease | Genetic Characteristics | Prevalence |
| Hemoglobin SS (Sickle Cell Anemia) | Two copies of the HbS gene | Common in sub-Saharan Africa and African American populations |
| Hemoglobin SC Disease | One HbS gene and one HbC gene | Prevalent in West Africa |
| Hemoglobin S Beta Thalassemia | One HbS gene and one beta thalassemia gene | Varies by region, influenced by the frequency of both genes |
| Rarer Forms (e.g., Hemoglobin SD, SE) | Combination of HbS with other abnormal hemoglobin genes | Generally lower prevalence, varies by region and ethnicity |
A study shows sickle cell disease’s diversity reflects the genetic variety of affected populations. This highlights the need for detailed genetic testing and counseling for those at risk.
Recognizing Symptoms and Complications
It’s important to know the early signs and complications of sickle cell disease. This helps in getting the right treatment early. Sickle cell disease affects people differently, so it’s key to know the various symptoms and complications.
Early Signs in Infants and Children
Infants and kids with sickle cell disease might show signs like jaundice, anemia, and swelling in the hands and feet. These happen because of sickled red blood cells blocking blood vessels. This can hurt tissues. Catching it early through newborn screenings helps start treatments early.
Acute Complications: Pain Crises and Infections
People with sickle cell disease often face pain crises and infections. Pain crises happen when sickled cells block blood flow, causing pain. Infections are a big worry because the spleen, which fights off germs, doesn’t work right. Quick medical help is needed to manage these issues.
Chronic Complications: Organ Damage and Disabilities
Long-term, sickle cell disease can cause organ damage and disabilities. Damage to organs like the kidneys, liver, and heart can happen from repeated blockages. Some might also face disabilities from strokes or other problems. Regular medical care helps lessen these long-term effects.
Psychological and Social Impact
The mental and social effects of sickle cell disease are big concerns. Dealing with a chronic illness can lead to depression and anxiety. It can also affect social life and daily activities. Getting help from mental health professionals and counselors is vital.
Diagnosis and Testing: Identifying Sickle Cell Disease
Diagnosing sickle cell disease starts with newborn screening, blood tests, and prenatal tests. Finding the disease early is key. It helps manage it better and improves life quality for those affected.
Newborn Screening Programs
Newborn screening is vital for catching sickle cell disease early. It involves a simple blood test from the newborn’s heel, usually in the first few days. This test looks for abnormal hemoglobin, showing if the disease or trait is present. Early detection lets doctors closely watch the child and start care when needed.
Blood Tests and Hemoglobin Electrophoresis
Blood tests are essential for diagnosing sickle cell disease at any age. Hemoglobin electrophoresis is a key test. It separates and identifies different hemoglobins in the blood. This test is vital for sickle cell disease diagnosis and differentiating it from other conditions.
Prenatal Testing Options
Pregnant women can get tested to see if their fetus has sickle cell disease. Tests like CVS and amniocentesis analyze fetal cells for genetic mutations. Prenatal diagnosis gives expectant parents important information for making informed choices about their pregnancy.
Carrier Testing for Family Members
Family members of those with sickle cell disease or trait should get carrier tested. This test finds carriers with one normal and one mutated hemoglobin gene. Knowing carrier status is critical for family planning and understanding the risk of passing the condition to future generations. Genetic counseling is often suggested for carriers to discuss their options and the implications of their carrier status.
Living with Sickle Cell Disease: Management Strategies
Managing sickle cell disease is a big job. It involves medical care, lifestyle changes, and support. These steps help improve life quality. A good plan includes treatments, lifestyle changes, and strong support.
Medical Management and Treatment Options
Medical care is key for sickle cell disease. There are several treatments:
- Hydroxyurea to reduce pain crises
- Blood transfusions to help tissues get oxygen
- Pain meds for both sudden and ongoing pain
- Antibiotics to stop infections
Current Treatments and Emerging Therapies
| Treatment | Description | Benefits |
| Hydroxyurea | Reduces pain crises | Improves life quality |
| Blood Transfusions | Boosts oxygen delivery | Lessens complications risk |
| Gene Therapy | Fixes genetic issue | Potential cure |
Lifestyle Adaptations for Better Health
Changing your lifestyle is important for sickle cell disease. Patients should:
- Drink plenty of water to avoid dehydration
- Avoid very hot or cold temperatures
- Exercise but not too hard
- Eat a balanced diet
A healthcare expert says, “Lifestyle changes can really help sickle cell disease patients.”
“Managing sickle cell disease needs both medical care and lifestyle changes. Being informed and proactive helps patients live full lives.”
Support Systems and Resources
Having support is essential for sickle cell disease patients. There are many resources:
- Support groups for patients and families
- Counseling for emotional help
- Info on the disease
By using medical care, lifestyle changes, and support, sickle cell disease patients can have better lives.
Special Considerations for Different Life Stages
Sickle cell disease is a lifelong condition that needs special care at different ages. As people grow, their needs change. Healthcare plans must adjust to meet these changes.
Childhood and Adolescence with Sickle Cell Disease
Children and teens with sickle cell disease face special challenges. Regular doctor visits and monitoring are key during these years. Early diagnosis and intervention can greatly improve their lives.
Managing pain, preventing infections, and helping with growth and development are important. These steps are vital for their care.
Reproductive Health and Pregnancy
For those with sickle cell disease, reproductive health and pregnancy need careful planning. Women with the disease face higher risks during pregnancy. Close monitoring is essential to avoid complications.
Genetic counseling is also important for those thinking about starting a family. It helps them understand the risks and chances of passing the condition to their children.
Aging with Sickle Cell Disease
As people with sickle cell disease get older, they may face more health issues. Comprehensive care is vital to address these problems. Managing chronic pain, living a healthy lifestyle, and staying current with vaccinations are key for older adults.
Understanding the unique challenges at different ages helps individuals with sickle cell disease and their healthcare providers. Together, they can develop effective management strategies. This improves overall health and well-being.
Advances in Treatment and Research
Research and development have changed how we treat sickle cell disease. We now focus on improving patient outcomes and quality of life.
Current FDA-Approved Medications
The U.S. Food and Drug Administration (FDA) has approved several medications for sickle cell disease. These include:
- Hydroxyurea: The first FDA-approved medication for sickle cell disease, known to reduce the frequency of pain crises.
- L-Glutamine: Approved to reduce the frequency of pain crises in adults and children with sickle cell disease.
- Crizanlizumab: Used to reduce the frequency of vaso-occlusive crises.
- Voxelotor: The first treatment approved to increase hemoglobin levels in patients with sickle cell disease.
These medications are a big step forward in managing sickle cell disease. They give patients more ways to control their condition.
Stem Cell Transplantation
Stem cell transplantation is the only cure for sickle cell disease. It replaces the patient’s bone marrow with healthy stem cells, usually from a donor. This treatment is effective but comes with risks and complications.
| Treatment Aspect | Description | Benefits |
| Donor Matching | Finding a compatible donor is key for transplant success. | Reduces the risk of graft-versus-host disease. |
| Conditioning Regimen | Chemotherapy or radiation prepares the patient’s body for the transplant. | Eliminates diseased bone marrow, making room for healthy stem cells. |
| Post-Transplant Care | Monitoring for complications and managing side effects. | Improves survival rates and reduces morbidity. |
Gene Therapy and CRISPR Technology
Gene therapy and CRISPR technology are leading the way in sickle cell disease treatment. They aim to fix the genetic mutation causing the disease.
Gene therapy introduces a healthy copy of the HBB gene into stem cells. CRISPR technology edits the defective gene precisely. Both methods could lead to a cure.
Clinical Trials and Emerging Treatments
Many clinical trials are exploring new treatments for sickle cell disease. These include gene therapies, small molecule inhibitors, and more.
Joining clinical trials gives patients access to new treatments. It also helps advance medical knowledge and develop future therapies.
Prevention Strategies and Genetic Counseling
Preventing sickle cell disease requires a few steps. These include genetic counseling and preconception testing. Knowing the disease’s genetic roots helps families plan their families better.
The Role of Genetic Counseling
Genetic counseling is key in stopping sickle cell disease. It tells families about the chances of passing the disease to their kids. Genetic counselors explain what it means to carry the gene and the odds of having a sickle cell child.
“Genetic counseling helps families make smart choices about having kids,” says a top genetic counselor. “It’s a vital step in stopping sickle cell disease.”
Preconception and Prenatal Testing
Testing before and during pregnancy is important. It finds carriers of the sickle cell gene and checks the risk of passing it to kids. Prenatal tests can spot sickle cell disease in the womb, giving parents options.
- Carrier screening before pregnancy
- Prenatal diagnosis through amniocentesis or chorionic villus sampling
- Preimplantation genetic diagnosis for IVF
Public Health Initiatives and Education
Public health efforts are vital in spreading the word about sickle cell disease. Education programs teach communities about genetic counseling and testing.
Genetic counseling, testing, and public health work together to lower sickle cell disease rates. Prevention is the best way to handle this complex condition.
Conclusion: Understanding Your Risk and Taking Action
Knowing your risk for sickle cell disease is key to managing and preventing it. We’ve looked at the disease’s genetic roots, where it’s common, and its different forms. By knowing who’s at risk, people can start taking steps to stay healthy.
New ways to manage sickle cell disease have greatly improved life for those with it. New treatments and therapies are showing great promise. It’s vital for people to learn about their risk and the options for managing it.
By planning ahead, getting regular health checks, and living a healthy lifestyle, you can lower your risk. We urge everyone to learn about their risk and take action for better health and disease management.
FAQ
What is sickle cell disease?
Sickle cell disease is a blood disorder. It makes red blood cells look like sickles. This affects their ability to carry oxygen.
What causes sickle cell disease?
It’s caused by a gene mutation. This leads to abnormal hemoglobin. It’s inherited in a specific way.
Who is at risk of getting sickle cell disease?
People from African, African American, Mediterranean, Middle Eastern, and Indian backgrounds are at higher risk. They might have the disease or be carriers.
What is the difference between sickle cell disease and sickle cell trait?
Sickle cell disease means having two abnormal genes. Sickle cell trait means having one normal and one abnormal gene. This makes someone a carrier.
Can sickle cell trait lead to sickle cell disease in offspring?
Yes, if both parents are carriers, their child might get sickle cell disease. This happens if they inherit two abnormal genes.
How is sickle cell disease diagnosed?
It’s diagnosed through newborn screening and blood tests. Hemoglobin electrophoresis and prenatal testing are also used.
What are the symptoms of sickle cell disease?
Symptoms include pain crises and infections. Anemia and organ damage are also possible.
How is sickle cell disease managed?
Management involves medical treatment and lifestyle changes. Support systems help too.
Are there any treatments available for sickle cell disease?
Yes, treatments include FDA-approved medications and stem cell transplantation. Gene therapy and CRISPR technology are also being explored.
Can sickle cell disease be prevented?
While it can’t be prevented, genetic counseling helps. It identifies carriers and at-risk couples for informed planning.
What is the role of genetic counseling in sickle cell disease?
Genetic counseling helps couples understand their risk. It guides them in planning their family.
How does sickle cell trait protect against malaria?
Sickle cell trait offers some protection against malaria. The parasite finds it hard to survive in sickled red blood cells.
References
- National Human Genome Research Institute. (2024, April 17). About Sickle Cell Disease. https://www.genome.gov/Genetic-Disorders/Sickle-Cell-Disease
- World Health Organization. (2023, July 6). Sickle-cell disease. https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease