Last Updated on October 20, 2025 by
At Liv Hospital, we are committed to delivering world-class healthcare with a focus on patient-centered care. Bone marrow disorders can affect the production of blood cells. This can quietly harm our health.
We will explore a wide range of bone marrow issues, from aplastic anemia to inherited syndromes. We will also discuss the latest research and treatment options. Accurate diagnosis and treatment are key to managing these conditions.
Key Takeaways
- Understanding bone marrow disorders is key for effective treatment.
- Bone marrow diseases can greatly affect our overall health.
- Getting an accurate diagnosis is vital for managing these complex conditions.
- Liv Hospital is dedicated to delivering top-notch, patient-centered care.
- We will look at various bone marrow conditions, including aplastic anemia and inherited syndromes.
Understanding Bone Marrow Issues: Function and Production of Blood Cells
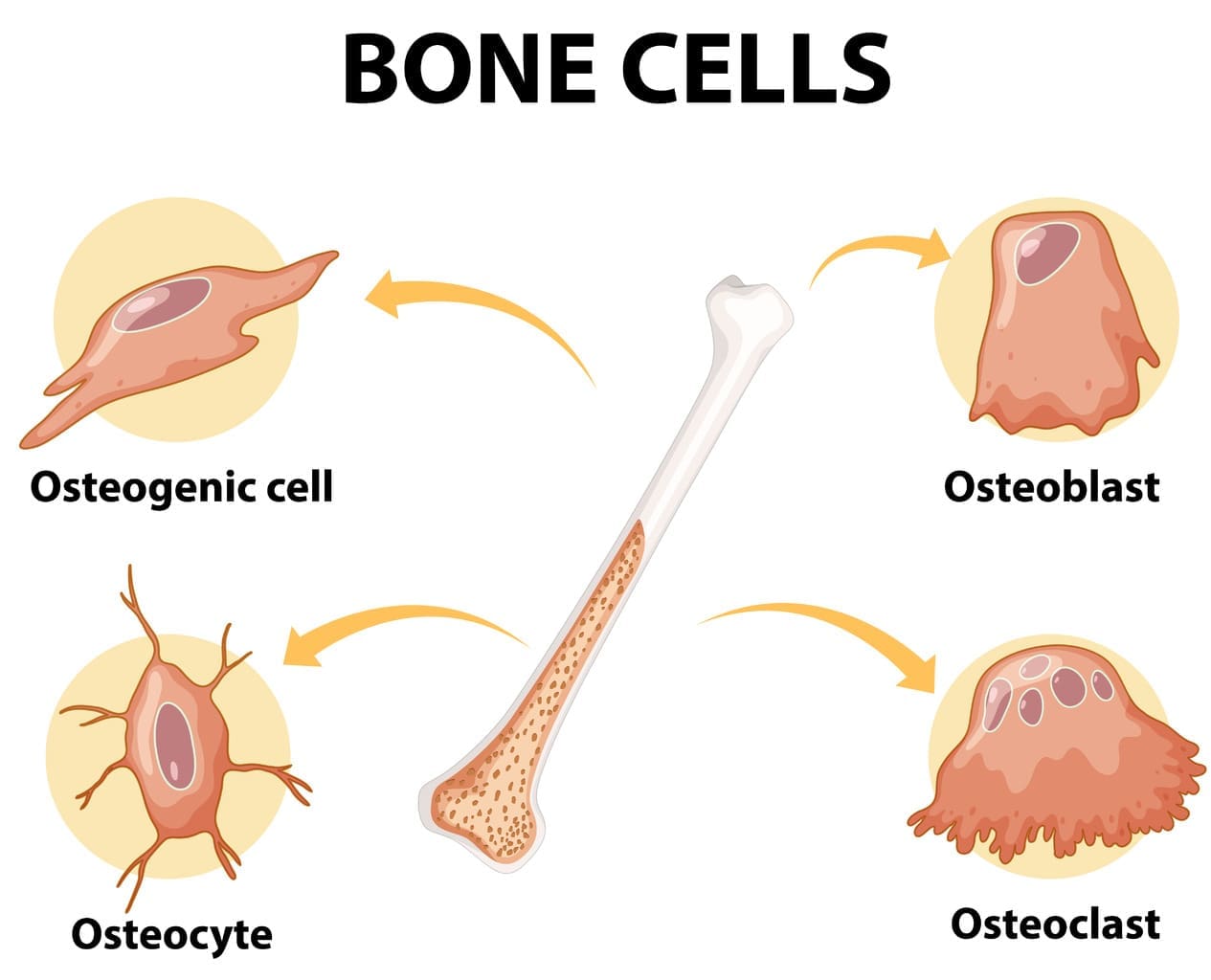
The bone marrow is key to our body’s blood production. It’s a vital tissue that can face different problems. It makes blood cells like red, white, and platelets, which carry oxygen, fight infections, and stop bleeding.
The Role of Bone Marrow in Blood Production
Bone marrow is the spongy tissue in bones like hips and thighbones. It makes blood cells through a process called hematopoiesis. Hematopoiesis turns stem cells into different blood cells. This ensures we get the right blood cells.
How Healthy Bone Marrow Functions
In healthy people, bone marrow works well to make blood cells. It needs stem cells, progenitor cells, and mature cells to do this. For example, red blood cells come from erythroblasts that lose their nucleus.
White blood cells, like neutrophils and lymphocytes, also have their own paths. Healthy bone marrow can adjust to our body’s needs. For example, it makes more white blood cells when we’re sick.
Common Signs of Bone Marrow Abnormalities
Problems with bone marrow can cause health issues. Signs include tiredness, infections, and easy bruising or bleeding. For instance, not enough red blood cells can make us weak.
| Signs | Description | Possible Cause |
|---|---|---|
| Fatigue | Persistent feeling of tiredness or weakness | Anemia due to reduced red blood cell production |
| Infections | Frequent or recurrent infections | Reduced white blood cell production |
| Bruising or Bleeding | Easy bruising or prolonged bleeding | Low platelet count due to bone marrow dysfunction |
Knowing these signs and their causes is important. It helps us catch and treat bone marrow problems early. For more on conditions like eltrombopag for refractory immune thrombocytopenia, we can look at the latest research and treatments.
Aplastic Anemia: When Bone Marrow Stops Producing Blood Cells
Aplastic anemia is a serious condition where the bone marrow fails to make blood cells. This includes red blood cells, white blood cells, and platelets. It’s important to seek medical help right away.
Causes and Risk Factors
Many things can cause aplastic anemia. These include genetics, toxins, certain medicines, and viruses. Knowing what causes it helps doctors treat it better.
Here are some risk factors for aplastic anemia:
- Exposure to chemicals like pesticides and benzene
- Use of certain drugs, such as antibiotics and anti-inflammatory medications
- Viral infections, including hepatitis and HIV
- Autoimmune disorders
- Genetic conditions, such as Fanconi anemia
Clinical Presentation and Symptoms
The symptoms of aplastic anemia vary. They depend on how bad the condition is and which blood cells are affected. Common symptoms include:
- Fatigue and weakness due to low red blood cell count (anemia)
- Frequent infections resulting from a low white blood cell count
- Bleeding or bruising easily due to low platelet count
- Shortness of breath
- Dizziness or lightheadedness
Diagnosis and Treatment Approaches
To diagnose aplastic anemia, doctors use blood tests and bone marrow biopsies. These help check the bone marrow’s function and rule out other conditions.
Treatment for aplastic anemia varies. It depends on how severe the condition is. Treatments may include:
| Treatment Approach | Description |
|---|---|
| Immunosuppressive Therapy | Medications that suppress the immune system to allow the bone marrow to recover |
| Bone Marrow Transplantation | Replacing the damaged bone marrow with healthy marrow from a donor |
| Supportive Care | Blood transfusions, antibiotics, and other treatments to manage symptoms and prevent complications |
Early diagnosis and treatment are key. They help manage aplastic anemia well and improve patient outcomes.
Myelodysplastic Syndromes (MDS): Precursors to Leukemia
Myelodysplastic syndromes (MDS) are complex bone marrow disorders. They are caused by ineffective blood cell production. We will look into the different types, symptoms, and treatments of MDS to understand it better.
Types of Myelodysplastic Syndromes
MDS has several subtypes, each with its own features. Knowing the type of MDS is key to understanding the prognosis and treatment. The main types are:
- Refractory Anemia (RA): This type is marked by anemia with few blasts in the bone marrow.
- Refractory Anemia with Ringed Sideroblasts (RARS): It is characterized by anemia and ringed sideroblasts.
- Refractory Cytopenia with Multilineage Dysplasia (RCMD): This involves dysplasia in multiple blood cell types.
- Refractory Anemia with Excess Blasts (RAEB): It is defined by a higher number of blasts in the bone marrow.
Symptoms and Disease Progression
Symptoms of MDS vary but often include fatigue, weakness, and shortness of breath. As MDS worsens, it can lead to infections and bleeding. The disease can progress slowly or quickly, sometimes turning into acute myeloid leukemia (AML).
It’s important to understand the risk factors and watch how the disease progresses. Regular check-ups and tests help manage MDS effectively. This way, treatment plans can be adjusted as needed.
Treatment Options and Prognosis
Treatment for MDS depends on the patient’s specific situation. It can range from supportive care like blood transfusions to more aggressive treatments like stem cell transplantation. The outcome varies based on the MDS type and how well the patient responds to treatment.
Every patient’s experience with MDS is different. Treatment plans must be tailored to meet their unique needs. Thanks to ongoing research, we are getting better at managing MDS, giving patients hope for a better future.
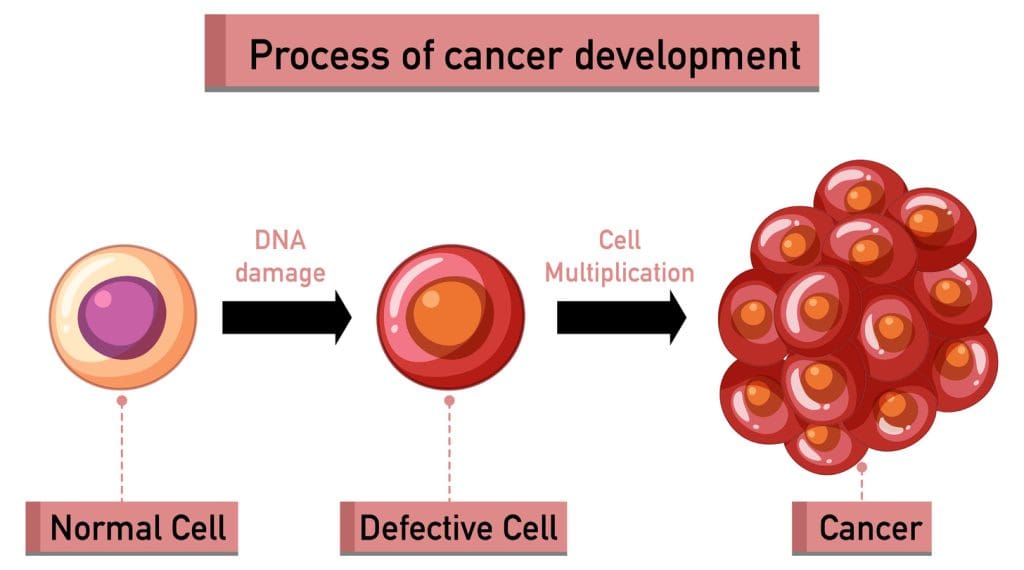
Leukemia: Cancer of the Bone Marrow
Leukemia is a serious bone marrow cancer that messes with blood cell making. It’s when bad white blood cells grow too much. This can cause many health problems.
Acute vs. Chronic Leukemia
Leukemia comes in two types: acute and chronic. Acute leukemia grows fast with young blood cells. Chronic leukemia grows slower with older cells.
- Acute leukemia needs quick treatment because it’s aggressive.
- Chronic leukemia might not show symptoms right away. It’s watched before treatment starts.
Major Types: ALL, AML, CLL, and CML
The main types of leukemia are based on the cell type and how fast it grows. The four main types are:
- Acute Lymphoblastic Leukemia (ALL): Affects lymphoid cells and is common in children.
- Acute Myeloid Leukemia (AML): Originates in myeloid cells and is more prevalent in adults.
- Chronic Lymphocytic Leukemia (CLL): Involves lymphoid cells and typically affects older adults.
- Chronic Myeloid Leukemia (CML): Characterized by the proliferation of myeloid cells and is often associated with a specific genetic abnormality.
Modern Treatment Approaches
Leukemia treatment has changed a lot. Now, we use targeted therapies and immunotherapies. Targeted therapy attacks specific cancer molecules. Immunotherapy boosts the immune system to fight cancer.
Today’s treatments include:
- Chemotherapy
- Targeted therapy
- Immunotherapy
- Stem cell transplantation
These new methods have made treatments better. We keep looking for more ways to fight leukemia.
Multiple Myeloma: Plasma Cell Disorder
Multiple myeloma is a serious bone marrow disorder. It happens when cancerous plasma cells grow too much. This disrupts the normal production of blood cells, causing many problems.
Pathophysiology and Development
The growth of cancerous plasma cells in multiple myeloma is complex. Genetic and epigenetic changes turn normal plasma cells into cancer. This leads to a lack of normal blood cells, causing anemia, low platelets, and low white blood cells.
- Genetic abnormalities such as translocations and mutations
- Interactions with the bone marrow microenvironment
- Resistance to apoptosis and increased proliferation
Clinical Manifestations
People with multiple myeloma show many symptoms. These include:
- Bone pain from bone damage
- Fatigue and weakness from anemia
- Recurring infections because of weak immune system
- High calcium levels from bone destruction
The disease can also harm the kidneys and cause neurological problems.
Diagnostic Criteria and Management
To diagnose multiple myeloma, doctors look at several things. These include:
- Monoclonal protein in blood or urine
- Clonal plasma cells in bone marrow
- Signs of damage to organs (CRAB criteria: high calcium, kidney problems, anemia, bone damage)
Treating multiple myeloma involves several steps. These include:
- Chemotherapy
- Targeted treatments like proteasome inhibitors and immunomodulatory drugs
- Stem cell transplant for some patients
- Supportive care to manage symptoms and improve life quality
Fanconi Anemia: A Rare Inherited Bone Marrow Failure Syndrome
We will look into Fanconi anemia, a rare genetic disorder. It causes bone marrow failure and raises the risk of cancer. This condition affects the body’s blood cell production, leading to health issues.
Genetic Basis and Inheritance Patterns
Fanconi anemia is due to DNA repair gene mutations. These mutations cause genomic instability. This leads to bone marrow failure and a higher cancer risk. It’s inherited in an autosomal recessive pattern, meaning a child needs two defective genes to have the condition.
Those with a family history of Fanconi anemia are at higher risk. Genetic testing can find carriers and affected individuals. Knowing the genetic cause is key for early diagnosis and treatment.
Clinical Features and Complications
Fanconi anemia symptoms vary among people. Common signs include:
- Bone marrow failure causing anemia, infections, and bleeding disorders
- Congenital anomalies like short stature, skeletal issues, and skin color changes
- Higher risk of cancer, like leukemia and other blood cancers
Screening and Treatment Strategies
Early diagnosis and treatment are key for Fanconi anemia management. Screening includes clinical checks, blood tests, and genetic tests. Treatment options include:
- Hematopoietic stem cell transplantation to fix bone marrow function
- Supportive care like blood transfusions and antibiotics for complications
- Regular cancer surveillance
Understanding Fanconi anemia’s genetics, symptoms, and treatments helps healthcare providers. They can offer better care to those affected and their families.
Diamond-Blackfan Anemia: Congenital Pure Red Cell Aplasia
We will look into Diamond-Blackfan anemia, a disorder that affects the bone marrow. It stops the bone marrow from making enough red blood cells. This leads to anemia and other health issues.
Genetic Factors and Pathogenesis
Diamond-Blackfan anemia is linked to gene mutations in ribosomal proteins. These mutations mess up the ribosome’s job, causing fewer red blood cells. It often runs in families but can also happen without a family history.
Genes and environment play a big role in how the condition develops. Knowing this helps doctors diagnose and treat it better.
Key Genetic Factors:
- Mutations in ribosomal protein genes
- Autosomal dominant inheritance
- Variable penetrance and expressivity
Clinical Presentation and Associated Anomalies
Children with Diamond-Blackfan anemia often show severe anemia early on. They might look pale, feel tired, and have trouble breathing. They also might not grow as expected.
- Pallor
- Fatigue
- Shortness of breath
- Failure to thrive
They might also have physical issues like:
- Craniofacial abnormalities
- Thumb abnormalities
- Cardiac defects
Management and Long-term Outlook
Managing Diamond-Blackfan anemia involves several steps:
- Corticosteroid therapy to stimulate red blood cell production
- Regular blood transfusions
- Bone marrow transplantation in severe cases
Thanks to new treatments, the outlook has gotten better. But, patients need ongoing care to handle any complications and watch for treatment side effects.
It’s key to provide full care for those with Diamond-Blackfan anemia. This includes their medical needs and the emotional impact of the disease.
Polycythemia Vera: When Bone Marrow Produces Too Many Red Blood Cells
When the bone marrow makes too many red blood cells, it leads to polycythemia vera. This is a disorder where the bone marrow makes too many red blood cells. This can make the blood thicker and cause serious problems.
The Role of JAK2 Mutation in Pathophysiology
Polycythemia vera is caused by a JAK2 gene mutation in most patients. This mutation turns on the JAK-STAT pathway. It makes more red blood cells than needed.
JAK2 Mutation and Its Impact
The JAK2 V617F mutation is key in polycythemia vera. It changes the JAK2 protein, making it always active. This leads to more red blood cells being made.
Symptoms and Complications
People with polycythemia vera may feel headaches, dizziness, and itching, worse after bathing. The thick blood can cause strokes or heart attacks.
The symptoms and complications of polycythemia vera can really affect a person’s life. It’s important to manage these symptoms to avoid lasting damage.
Treatment Strategies and Monitoring
Treatment for polycythemia vera aims to prevent complications by making the blood less thick. This is done through phlebotomy, which removes blood to lower red blood cell count. Medications like hydroxyurea also help by slowing down bone marrow.
Monitoring is key in managing polycythemia vera. Regular blood tests help see if treatment is working and make changes as needed.
| Treatment Approach | Description | Benefits |
|---|---|---|
| Phlebotomy | Regular removal of blood to reduce red blood cell count | Reduces blood viscosity, lowering the risk of thrombosis |
| Hydroxyurea | Medication to suppress bone marrow activity | Decreases the production of red blood cells, reducing the need for frequent phlebotomy |
| Aspirin | Antiplatelet therapy to reduce the risk of thrombosis | Lowers the risk of cardiovascular events |
Myelofibrosis: Scarring of the Bone Marrow
Myelofibrosis is a disorder that scars the bone marrow. This scarring disrupts blood cell production. It can cause anemia, fatigue, and an enlarged spleen. We will look at the different types, symptoms, and treatment options.
Primary vs. Secondary Myelofibrosis
There are two main types of myelofibrosis: primary and secondary. Primary myelofibrosis happens on its own. Secondary myelofibrosis comes from another disorder, like polycythemia vera.
Primary myelofibrosis often has genetic mutations, like the JAK2 V617F mutation. Secondary myelofibrosis usually comes from another myeloproliferative disorder.
Clinical Features and Disease Progression
Myelofibrosis symptoms vary. Common ones are fatigue, weakness, weight loss, and night sweats. An enlarged spleen is also common, causing abdominal pain.
The disease can progress differently for everyone. Some stay stable for years, while others have a faster progression. Regular check-ups are key to managing the disease.
Therapeutic Options and Stem Cell Transplantation
Treatment for myelofibrosis depends on the patient. It may include medicines for symptoms like anemia and spleen enlargement. Ruxolitinib, a JAK inhibitor, is often used to shrink the spleen and ease symptoms.
In some cases, stem cell transplantation is an option, mainly for younger patients with high-risk disease. This involves replacing the bone marrow with healthy stem cells. It can cure the disease but has risks like graft-versus-host disease.
We aim to give the best care for myelofibrosis patients. We use the latest treatments to improve their quality of life and outcomes.
Hemophagocytic Lymphohistiocytosis (HLH): Rare but Severe Bone Marrow Condition
We will look into HLH, a rare condition that affects the immune system and bone marrow. It causes immune cells to act abnormally, leading to too much inflammation. This can be very dangerous.
Primary vs. Secondary HLH
HLH comes in two types: primary and secondary. Primary HLH is linked to genetic problems in immune cells. Secondary HLH is caused by infections, cancers, or autoimmune diseases.
Key differences between primary and secondary HLH:
| Characteristics | Primary HLH | Secondary HLH |
|---|---|---|
| Genetic Component | Often present | Generally absent |
| Triggers | Not typically identified | Infections, malignancies, autoimmune diseases |
| Age of Onset | Often in infancy or early childhood | Can occur at any age |
Clinical Presentation and Diagnostic Criteria
The symptoms of HLH can vary but often include fever, swollen liver and spleen, and low blood counts. Doctors use a mix of symptoms, lab tests, and sometimes genetic tests to diagnose it.
Treatment Protocols and Outcomes
Treatment for HLH usually involves medicines to stop the immune system from overacting. In some cases, a bone marrow transplant might be needed. Quick diagnosis and treatment are key to better outcomes.
Treatment Approaches:
- Immunosuppressive medications
- Chemotherapy
- Hematopoietic stem cell transplantation
- Supportive care
Conclusion: Advances in Bone Marrow Disorder Management and Future Directions
Recent studies have greatly improved how we diagnose and treat bone marrow disorders. We’ve looked at many conditions, like aplastic anemia and leukemia. Now, treatments range from targeted therapies to stem cell transplants.
There are many bone marrow diseases, and research keeps finding new ways to understand them. Thanks to new treatments, patients are living longer and better lives. The focus now is on making treatments even more tailored to each patient.
Looking ahead, more research and investment are key. New discoveries and technologies promise better care for patients. Healthcare teams can offer top-notch care by keeping up with these advances.
FAQ
What are bone marrow disorders?
Bone marrow disorders are conditions that affect the bone marrow’s ability to make healthy blood cells. This includes aplastic anemia, myelodysplastic syndromes, leukemia, and other serious conditions.
What is the role of bone marrow in blood production?
The bone marrow is key in making blood cells. It produces red blood cells, white blood cells, and platelets. These cells are vital for keeping blood healthy.
What are the common signs of bone marrow abnormalities?
Signs of bone marrow problems include fatigue, infections, bruising, and bleeding. These symptoms can point to underlying bone marrow disorders.
What is aplastic anemia, and how is it treated?
Aplastic anemia is when the bone marrow can’t make blood cells. Treatment includes immunosuppressive therapy and bone marrow transplantation.
What are myelodysplastic syndromes, and how do they progress?
Myelodysplastic syndromes are disorders that can turn into leukemia. Treatment options include supportive care and hematopoietic stem cell transplantation.
What are the different types of leukemia?
Leukemia is divided into acute and chronic types. The main subtypes are acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL), and chronic myeloid leukemia (CML).
What is multiple myeloma, and how is it managed?
Multiple myeloma is a plasma cell disorder. It needs a detailed treatment plan, including chemotherapy, targeted therapy, and stem cell transplantation.
What is Fanconi anemia, and how is it treated?
Fanconi anemia is a rare inherited bone marrow failure syndrome. It requires early diagnosis and treatment, including hematopoietic stem cell transplantation.
What is polycythemia vera, and how is it managed?
Polycythemia vera is when the bone marrow makes too many red blood cells. Treatment aims to manage the condition to prevent complications.
What is myelofibrosis, and how is it treated?
Myelofibrosis is a condition with scarring in the bone marrow. Treatment options include stem cell transplantation.
What is Hemophagocytic Lymphohistiocytosis (HLH), and how is it treated?
HLH is a rare but severe bone marrow condition. It needs prompt and effective treatment, including specific protocols to manage it.
What are the advances in managing bone marrow disorders?
Advances include better diagnostic tools, targeted therapies, and immunotherapies. These have improved patient outcomes and quality of life.
What is the future direction of research in bone marrow disorders?
Ongoing research is key for new treatments and better patient care. It focuses on understanding the causes of these conditions.
What are the different bone marrow conditions?
Bone marrow conditions include aplastic anemia, myelodysplastic syndromes, leukemia, multiple myeloma, Fanconi anemia, Diamond-Blackfan anemia, polycythemia vera, myelofibrosis, and Hemophagocytic Lymphohistiocytosis (HLH).
What are the symptoms of bone marrow diseases?
Symptoms include fatigue, infections, bruising, bleeding, and signs of abnormal blood cell production.
How are bone marrow disorders diagnosed?
Diagnosis involves blood counts, bone marrow biopsies, and genetic testing. These tests help find the cause of the condition.
References
- National Cancer Institute (NCI) DCEG: Bone Marrow Failure Syndromes Research
- National Cancer Institute (NCI): Bone Marrow Failure (Rare Tumors)
- National Center for Biotechnology Information (NCBI): Academic Article on Aplastic Anemia and Bone Marrow Failure Syndromes