
Acute myeloid leukemia (AML) is a fast-growing blood cancer. It can have different outcomes, even with common treatments. Getting a diagnosis of AML can feel overwhelming. But, new allogeneic hematopoietic stem cell transplantation methods offer hope for a cure and a fresh start for many.
At top centers, patients get the latest in leukemia care. This includes advanced stem cell and bone marrow transplants. Studies show that while high-dose chemotherapy works for many, relapse rates are high. This makes allo-HSCT a key choice for those at high risk of coming back.
Trust in expert care is key when outcomes are unsure. Our team offers caring, team-based care. We blend global protocols with personal support.
Key Takeaways
- Allogeneic hematopoietic stem cell transplantation is a key treatment for AML patients at high risk of coming back.
- Standard chemotherapy may lead to remission, but relapse rates are high.
- Advanced stem cell and bone marrow transplants offer new hope for AML patients.
- Specialized centers offer the latest treatments and caring support.
- Expert care is vital for dealing with uncertain outcomes in AML treatment.
Understanding Acute Myeloid Leukemia (AML)
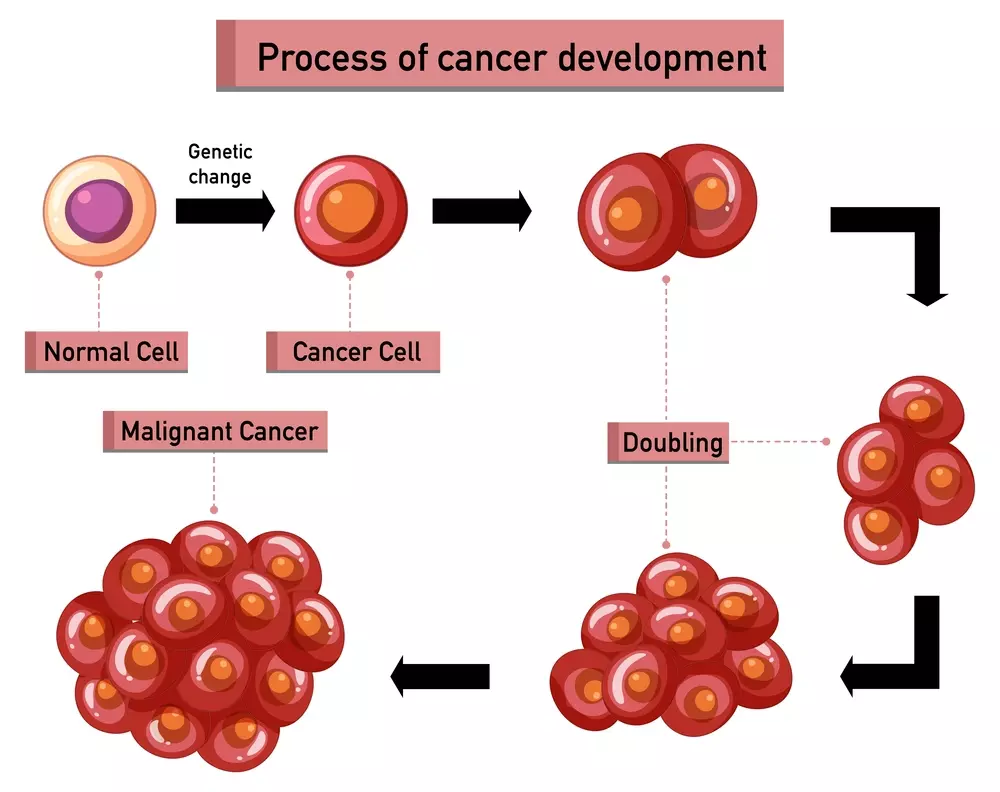
It’s important for patients and doctors to know about Acute Myeloid Leukemia (AML). This is a fast-growing blood cancer that needs special treatment. AML happens when abnormal white blood cells grow too fast in the bone marrow.
The Nature of This Aggressive Blood Cancer
AML grows quickly and can spread fast. Without treatment, it can cause serious problems like infections and bleeding. This is why finding and treating AML quickly is so important.
Symptoms of AML include feeling very tired, losing weight, and getting sick often. These happen because the leukemia cells take over the bone marrow. This means there are fewer healthy blood cells.
Why Standard Treatments Often Fall Short
Most treatments for AML are chemotherapy and sometimes targeted therapy. These can work well at first but often don’t last. The main problem is that AML can come back, even if the treatment seems to work.
AML patients might also not respond well to treatment or could face serious side effects. This is a big worry because AML can be hard to treat.
Some big challenges with AML treatments are:
- AML can come back because some cancer cells are left behind
- Chemotherapy can have very bad side effects
- Older patients or those with certain genetic traits might not respond well
For some patients, a stem cell transplant might be the best option. It replaces the bad bone marrow with healthy stem cells. This could lead to a long-term cure and better survival chances.
What Is an AML Stem Cell Transplant?

An AML stem cell transplant is a complex procedure. It replaces diseased bone marrow with healthy stem cells. This treatment is for patients with Acute Myeloid Leukemia (AML) at high risk of relapse or who have relapsed after initial treatment.
The Science Behind Replacing Diseased Bone Marrow
The goal of an AML stem cell transplant is to get rid of leukemia cells in the bone marrow. It replaces them with healthy stem cells. This is done through hematopoietic stem cell transplantation.
In this process, stem cells are infused into the patient’s bloodstream. They then go to the bone marrow and start making healthy blood cells.
The stem cell transplant for AML involves several steps. These include:
- Pre-transplant conditioning to eliminate existing bone marrow and leukemia cells
- Infusion of healthy stem cells from a donor or the patient’s own cells
- Post-transplant care to monitor for complications and support recovery
Determining Transplant Eligibility
Not all AML patients can get a bone marrow transplant for leukemia. Who can get one depends on their health, leukemia stage, and donor availability. Patients thinking about an AML stem cell transplant should talk to their doctor about it.
Things that affect transplant eligibility include:
- Age and overall health status
- AML subtype and genetic characteristics
- Response to previous treatments
- Availability of a suitable donor for allogeneic transplantation
Knowing about the leukemia stem cell transplantation process and who can get it is key. It helps in making informed choices about AML treatment.
Key Fact #1: Types of Transplants for AML Patients
Understanding the different stem cell transplants for Acute Myeloid Leukemia (AML) is key. AML patients have two main options: allogeneic and autologous stem cell transplantation. Each has its own benefits and things to consider.
Allogeneic Transplantation Using Donor Cells
Allogeneic hematopoietic stem cell transplantation uses stem cells from a donor. It’s important for AML patients because it replaces the diseased bone marrow with healthy cells. It also brings in a new immune system to fight leukemia.
Benefits of Allogeneic Transplantation:
- Graft-versus-leukemia effect, where the donor’s immune cells help fight remaining leukemia cells
- Potential for cure, even for high-risk AML patients
Autologous Transplantation Using Patient’s Own Cells
Autologous transplantation uses the patient’s own stem cells. This method is less common for AML because of the risk of bringing back malignant cells. But, it’s an option for some patients, like those in complete remission.
Considerations for Autologous Transplantation:
- Lower risk of graft-versus-host disease (GVHD)
- Potential for faster engraftment
Why Allogeneic Is Often Preferred for AML
Allogeneic transplantation is often chosen for AML patients because it can cure the disease. It has risks like GVHD, but the benefits are worth it for high-risk or relapsed AML patients.
| Transplant Type | Donor Source | Graft-Versus-Leukemia Effect | Risk of GVHD |
|---|---|---|---|
| Allogeneic | Related or unrelated donor | Yes | Higher |
| Autologous | Patient’s own cells | No | Lower |
The table shows the choice between allogeneic and autologous transplantation depends on several factors. These include the patient’s condition, donor availability, and the specific characteristics of their AML.
A renowned hematologist says, “Choosing between allogeneic and autologous transplantation for AML patients is complex. It requires looking at the patient’s health, the leukemia specifics, and the benefits and risks of each transplant type.”
“The graft-versus-leukemia effect is a powerful tool in our fight against AML, and allogeneic transplantation makes this possible.” -Hematologist
Key Fact #2: The Donor Selection Process
For AML patients, finding the right donor is the first step towards a successful stem cell transplant. This process is key to the transplant’s success and the patient’s survival.
Finding Related vs. Unrelated Donors
Choosing between a related or unrelated donor is the first decision. Related donors, like siblings or parents, have a higher chance of being a good match because they share more genes. But, not everyone has a related donor, so unrelated donors are also important.
Unrelated donors are people who offer to donate stem cells to those in need. Organizations like the National Marrow Donor Program (NMDP) help find these donors by keeping a big database.
HLA Typing and Compatibility Requirements
HLA (Human Leukocyte Antigen) typing is a key part of finding a donor. It checks if the donor and recipient’s genes match well. A good match lowers the risk of complications after the transplant.
HLA typing looks for specific genetic markers to see if the donor and recipient are compatible. The closer the match, the better the chances of a successful transplant.
Alternative Donor Sources When Matches Aren’t Available
If no good match is found, other options are considered. Cord blood and haploidentical donors are two such options.
Cord blood comes from the umbilical cord after birth and is a quick source of stem cells. Haploidentical donors, who are half-matched to the patient, offer another choice. These alternatives face their own challenges but help more patients find a donor.
Key Fact #3: Pre-Transplant Conditioning Regimens
Before an AML stem cell transplant, patients must undergo pre-transplant conditioning. This step is key to get the body ready for the transplant. It removes the diseased bone marrow and weakens the immune system to stop the new stem cells from being rejected.
Myeloablative vs. Reduced-Intensity Conditioning
There are two main conditioning regimens: myeloablative and reduced-intensity conditioning. Myeloablative conditioning uses high doses of chemotherapy and/or radiation to wipe out the bone marrow. It’s more aggressive and best for younger patients or those with fewer health problems.
Reduced-intensity conditioning (RIC) uses lower doses of chemotherapy and/or radiation. RIC is better for older patients or those with serious health issues. It’s less harsh and lowers the risk of complications.
“The choice between myeloablative and reduced-intensity conditioning depends on various factors, including the patient’s age, overall health, and the specific characteristics of their AML.”
How Conditioning Affects Transplant Success
The conditioning regimen is vital for the success of the AML stem cell transplant. Good conditioning kills leukemia cells, makes room for new stem cells, and prevents graft rejection. The intensity of the regimen can affect the risk of complications like GVHD and infections.
Tailoring Conditioning to Patient Factors
We customize the conditioning regimen for each patient to increase transplant success. This personalized approach considers the patient’s age, health, AML characteristics, and genetics. It helps reduce complications and improve the chance of long-term remission.
“The art of medicine lies in the ability to tailor treatments to the individual needs of each patient,” a principle that guides our approach to pre-transplant conditioning regimens.
Key Fact #4: The Transplantation Procedure and Recovery
A stem cell transplant is a lifesaving procedure for patients with Acute Myeloid Leukemia (AML). This complex process involves replacing diseased bone marrow with healthy stem cells. These stem cells come from a donor or the patient themselves.
What Happens During the Actual Transplant
The stem cell transplant procedure is quite straightforward. It involves a few key steps:
- Infusing the stem cells into the patient’s bloodstream through a central line.
- Monitoring the patient for any immediate reactions to the infusion.
- Providing supportive care to manage symptoms and prevent complications.
The infusion process usually takes about 1-2 hours. But the whole process, including preparation and recovery, can take several hours.
Critical Post-Transplant Milestones
After the transplant, several critical milestones mark the patient’s progress:
- Engraftment: The point at which the transplanted stem cells begin producing new blood cells.
- Graft function: The transplanted cells start functioning properly, producing healthy blood cells.
- Immune system recovery: The patient’s immune system begins to recover, reducing the risk of infections.
Timeline for Blood Count Recovery
Blood count recovery is a key indicator of the transplant’s success. Typically:
- Neutrophil recovery occurs within 2-4 weeks post-transplant.
- Platelet recovery may take longer, often requiring 3-6 weeks or more.
- Red blood cell recovery can take several months, sometimes requiring transfusions.
Understanding the transplantation procedure and recovery process is vital for patients and their families. Knowing what to expect helps us prepare for the challenges and opportunities ahead.
Key Fact #5: Possible Complications and Side Effects
AML stem cell transplant can cure leukemia, but it comes with risks. We need to know these risks and how to handle them.
Understanding Graft-Versus-Host Disease
Graft-versus-host disease (GVHD) is a big risk with allogeneic stem cell transplant. It happens when the donor’s immune cells attack the recipient’s body. GVHD can be mild or very serious.
Acute GVHD happens early, affecting skin, liver, and gut. Chronic GVHD can take months or years, affecting many organs and causing a lot of suffering.
Dealing with GVHD needs a careful plan. This includes medicines and supportive care. We watch patients closely for GVHD signs and adjust their treatment as needed.
Infection Risks and Immune System Recovery
After an AML stem cell transplant, patients face high infection risks. The treatment before the transplant kills off their immune cells. This leaves them open to infections until their new immune system kicks in.
- Bacterial infections are a big worry, mainly during the neutropenic phase.
- Viral infections, like CMV reactivation, need constant watching and prevention.
- Fungal infections can be deadly and need antifungal prevention.
We use many ways to lower these risks. This includes using antibiotics, checking for infections, and treating them quickly.
Long-Term Health Considerations
Survivors of AML stem cell transplant face long-term health issues. These include managing chronic GVHD, watching for late transplant effects, and keeping overall health good. They might face problems like endocrine issues, secondary cancers, and heart disease.
“Long-term survivors of AML stem cell transplant need ongoing care to manage late effects and improve their quality of life.”
We stress the need for follow-up care and healthy lifestyle choices. This helps ensure long-term health and well-being.
Key Fact #6: Can AML Stem Cell Transplant Cure Leukemia?
Many people wonder if AML stem cell transplant can cure leukemia. We’ll look into what it means to be “cured” in AML. We’ll also explore the graft-versus-leukemia effect and how often leukemia comes back after transplant.
Defining “Cure” in the Context of AML
In AML, a “cure” means the disease doesn’t come back after treatment. It’s hard to achieve because AML is aggressive and relapse is a risk. AML stem cell transplant is seen as a cure because it replaces the patient’s bad bone marrow with healthy cells.
The Graft-Versus-Leukemia Effect
The graft-versus-leukemia (GVL) effect is key to AML stem cell transplant’s success. It happens when the donor’s immune cells fight the leukemia in the patient. This effect helps get rid of any leftover leukemia cells, lowering the chance of relapse.
Relapse Rates After Transplantation
Even with the chance of a cure, relapse is a big worry after AML stem cell transplant. The risk depends on the patient’s health, AML stage at transplant, and how well the donor and recipient match. Knowing these factors helps manage expectations and make treatment choices.
| Factor | Influence on Relapse Rate |
|---|---|
| Patient’s Age | Generally, younger patients have lower relapse rates. |
| AML Stage at Transplant | Patients transplanted in remission have lower relapse rates than those with active disease. |
| Donor Match Quality | A better donor match can reduce the risk of relapse. |
Understanding what makes AML stem cell transplant successful helps patients and doctors. While some may be cured, all need ongoing care to catch and manage any relapse.
Key Fact #7: Survival Rates and Quality of Life
The journey doesn’t end with the transplant. Understanding survival rates and quality of life is vital. After an AML stem cell transplant, patients want to know about their survival chances and future quality of life. We will look at short and long-term survival rates, factors that affect transplant outcomes, and what life is like after a successful transplant.
Statistical Overview of Short and Long-Term Survival
Survival rates after an AML stem cell transplant have improved a lot. This is thanks to better medical technology and care after the transplant. Studies show that survival rates depend on age, health, and leukemia stage at transplant time. For example, a study found that the 3-year overall survival rate can be between 40% and 60%.
For more detailed information on survival rates and success rates of stem cell transplants, you can visit LivHospital’s resource on stem cell transplant success. This resource gives detailed insights into survival rates and transplant success factors.
Factors That Influence Transplant Outcomes
Several factors are key in determining transplant outcomes. These include:
- The patient’s age and overall health
- The stage of AML at the time of transplant
- The degree of HLA matching between donor and recipient
- The conditioning regimen used before the transplant
Knowing these factors helps set realistic expectations and make informed transplant decisions.
Life After Successful Transplantation
After a successful AML stem cell transplant, patients go through a recovery period. This can last several months to a year or more. They are closely monitored for any complications or relapse signs.
The quality of life after transplant varies. Some patients can return to normal activities, while others face long-term side effects. It’s important for patients to follow a healthy lifestyle, including a balanced diet and regular exercise, to improve recovery and well-being. Regular follow-up appointments with their healthcare provider are also key to monitor health and address concerns promptly.
Conclusion: Making Informed Decisions About AML Treatment
Exploring AML stem cell transplant shows how important it is to make smart choices about aml treatment. Knowing about leukemia treatment, like transplant types and donor selection, helps patients and families. It lets them be more involved in their care.
A stem cell transplant for aml can save lives, but it’s vital to consider the pros and cons. We suggest talking to doctors to find the right leukemia treatment for each person.
Being well-informed and working with healthcare teams helps patients make informed decisions. This can lead to better treatment results and a better life. As we keep improving aml treatment, we’re dedicated to supporting those with this tough disease.
What is an AML stem cell transplant?
An AML stem cell transplant is a procedure. It replaces diseased bone marrow with healthy stem cells. This is to treat Acute Myeloid Leukemia (AML).
How does a stem cell transplant work for AML?
The transplant process replaces the patient’s diseased bone marrow. It uses healthy stem cells, either from a donor or the patient’s own cells. This helps produce healthy blood cells.
What are the types of stem cell transplants available for AML patients?
There are two main types. Allogeneic transplantation uses donor cells. Autologous transplantation uses the patient’s own cells. Allogeneic transplantation is often preferred for AML because of its graft-versus-leukemia effect.
How is a donor selected for an AML stem cell transplant?
Donor selection involves HLA typing and compatibility testing. This is to find a matching donor, whether related or unrelated. If a match is not available, alternative donor sources are considered.
What is the pre-transplant conditioning regimen for AML stem cell transplant?
Pre-transplant conditioning regimens prepare the patient’s body for the transplant. They suppress the immune system and eradicate diseased bone marrow. These regimens can be myeloablative or reduced-intensity.
What are the possible complications and side effects of AML stem cell transplant?
Possible complications include Graft-Versus-Host Disease (GVHD) and infection risks. Long-term health considerations are also important. Managing these complications is key for long-term health.
Can AML stem cell transplant cure leukemia?
AML stem cell transplant can cure leukemia, thanks to the graft-versus-leukemia effect. But, relapse rates after transplantation vary. “Cure” is defined as long-term remission.
What are the survival rates and quality of life after AML stem cell transplant?
Survival rates depend on factors like patient health, donor match, and transplant type. Successful transplantation can improve quality of life. Many patients achieve long-term survival.
What is the difference between myeloablative and reduced-intensity conditioning?
Myeloablative conditioning is more aggressive. It completely eradicates the patient’s bone marrow. Reduced-intensity conditioning is less aggressive. It preserves some of the patient’s bone marrow function.
How long does it take for blood counts to recover after AML stem cell transplant?
Blood count recovery time varies. It usually takes several weeks to months for blood counts to normalize after transplant.
What is the graft-versus-leukemia effect in AML stem cell transplant?
The graft-versus-leukemia effect is a beneficial reaction. The transplanted donor cells recognize and attack residual leukemia cells. This helps prevent relapse.
Is AML stem cell transplant the only treatment option for AML?
No, AML stem cell transplant is not the only treatment option. Standard chemotherapy and other treatments are available. But, transplant is often considered for eligible patients. This is because it has the chance for long-term remission or cure.
References
- Leukemia Research Foundation. Transplants. https://leukemiarf.org/patients/treatment/options/transplants/
- Cancer Research UK. Stem cell or bone marrow transplant for AML. https://www.cancerresearchuk.org/about-cancer/acute-myeloid-leukaemia-aml/treating-aml/stem-cell-bone-marrow-transplant
- PubMed. Research. https://pubmed.ncbi.nlm.nih.gov/34012445/




































