Last Updated on October 20, 2025 by

Removing skin cancer from the nose is a delicate task. At Liv Hospital, our team focuses on patient care. We treat basal cell carcinoma with great care and precision.
Basal cell carcinoma on the nose needs a careful surgical method. Our guide will show you the steps, from start to finish. It highlights the need for a team effort for the best results.
Key Takeaways
- Mohs surgery is a highly effective technique for removing basal cell carcinoma, even on the nose.
- A team approach ensures the best results and less chance of scarring.
- Our expert team at Liv Hospital offers patient-focused care and support.
- Reconstruction techniques are key for looking good after surgery.
- Our main goal is to remove all cancer cells.
Understanding Basal Cell Carcinoma of the Nose
It’s important to know about basal cell carcinoma on the nose for good treatment. Basal cell carcinoma (BCC) is the most common skin cancer. It’s tricky on the nose because of its complex shape and how it looks.
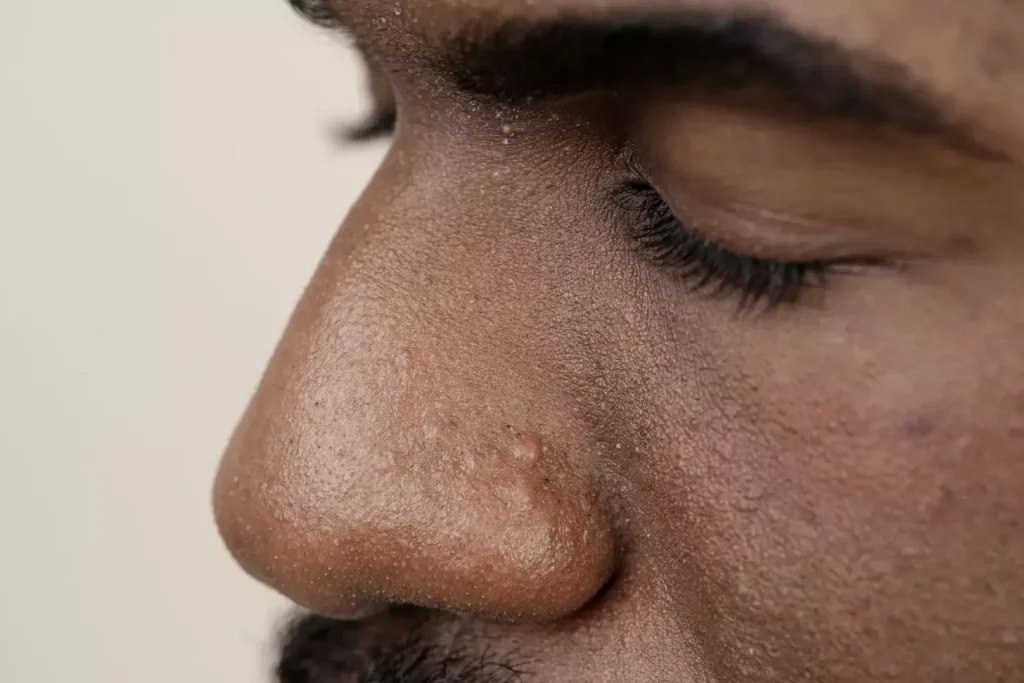
Common Presentations and Diagnosis
Basal cell carcinoma on the nose can look different. This makes finding it and treating it key. Common looks include:
- Nodular lesions
- Pigmented lesions
- Sclerodermiform or morpheaform lesions
- Superficial lesions
Doctors use a mix of looking at the skin and lab tests to find BCC. Dermoscopy helps tell BCC apart from other skin issues.
Risk Factors and Prevention
Many things can make basal cell carcinoma on the nose more likely. These include:
| Risk Factor | Description |
|---|---|
| UV Radiation Exposure | Too much UV from the sun or tanning beds raises BCC risk. |
| Fair Skin | People with fair skin are more at risk because they have less melanin. |
| Genetic Predisposition | Having skin cancer in your family can up your risk. |
To prevent BCC, use sunscreen with high SPF, wear clothes that cover you, and stay out of the sun when it’s strongest.
“Prevention is key when it comes to basal cell carcinoma. By understanding the risk factors and taking proactive measures, individuals can significantly reduce their likelihood of developing this condition.”
Importance of Early Detection
Finding basal cell carcinoma on the nose early is very important. Early on, BCC is easy to treat. There are many ways to treat it, like surgery, Mohs surgery, and creams.
Early detection helps treatment work better and lowers the chance of big scars and changes in how you look. So, watch your skin closely and see a doctor if you notice anything odd.
Pre-Surgical Assessment and Planning

Before surgery, we assess and plan carefully for o. This ensures the surgery fits the patient’s needs perfectly.
Patient Evaluation and Medical History
We start with a detailed patient evaluation and medical history. This is key to knowing what might affect the surgery or recovery. Important parts of the medical history include past surgeries, allergies, and current medications.
We also check the patient’s health and any surgery risks. This helps us create a plan that reduces risks and improves results.
Imaging and Diagnostic Techniques
Imaging and diagnostic techniques are essential for diagnosing basal cell carcinoma. Tools like dermoscopy and biopsy give us vital information about the tumor. This lets us choose the best treatment.
- Dermoscopy helps us see the tumor’s shape and any special features.
- Biopsy confirms the diagnosis and shows how aggressive the tumor is.
These tools are key in planning the surgery. They help us understand the tumor’s size and how it affects nearby tissues.
Determining Optimal Surgical Approach
Finding the best surgical approach is a big part of the pre-surgery process. We look at the tumor’s size, location, and depth. We also consider the patient’s health and what they want.
“The goal of pre-surgical assessment is to develop a surgical plan that balances oncological efficacy with aesthetic and functional outcomes.” – Expert in Dermatologic Surgery
By carefully looking at these factors, we choose the best surgical method. This could be Mohs surgery, standard excision, or another option. We aim for the best outcome for the patient.
Basal Cell Nose Surgery: Preparation and Setup
To make basal cell nose surgery a success, we need to prepare everything carefully. This includes the equipment, how the patient is positioned, and the anesthesia used.
Surgical Equipment and Materials
The right equipment and materials are key to a successful surgery. Essential equipment includes:
- Surgical scalpels and blades
- Electrocautery units for hemostasis
- Sutures and needles of various sizes
- Surgical loupes or microscopes for magnification
High-quality equipment helps with precision and better patient results.
Patient Positioning and Preparation
Getting the patient in the right position is important. It helps the surgeon access the area and keeps the patient comfortable and safe.
- Patients are positioned supine with their head slightly elevated.
- The surgical site is cleaned and prepared with antiseptic solutions.
- Draping is applied to isolate the surgical field and maintain sterility.
Anesthesia Options and Administration
Anesthesia is vital for patient comfort during surgery. Common anesthesia options include:
- Local anesthesia: numbs the specific area of the surgery
- Conscious sedation: helps relax the patient while remaining awake
- General anesthesia: renders the patient unconscious, used in more complex cases
The choice of anesthesia depends on the surgery’s extent, patient preference, and the surgeon’s advice. Effective anesthesia administration is essential for a stress-free surgery.
Mohs Surgery for Basal Cell Carcinoma on Nose
Mohs surgery is a precise treatment for basal cell carcinoma on the nose. It’s great because it saves the tissue around the tumor. This is key for keeping the nose looking and working right.
Principles and Step-by-Step Technique
Mohs surgery carefully removes the tumor in stages. It checks each layer under a microscope to make sure all cancer is gone. First, the area is numbed with local anesthesia.
The surgeon then takes out the tumor and a thin layer of tissue. They check it under a microscope for cancer. If they find cancer, they take out more tissue. This keeps going until there’s no cancer left.
Benefits of Tissue-Sparing Approach
Mohs surgery is good because it saves as much tissue as it can. This is very important on the nose. It helps keep the nose looking and working well.
This method also means less need for big surgeries later. This can lead to less scarring and better looks.
99% Cure Rate for Primary Cases
Mohs surgery has a 99% success rate for first-time cases. This is because it checks every part of the tumor. This makes sure all cancer is removed.
| Treatment Characteristics | Mohs Surgery | Standard Excision |
|---|---|---|
| Cure Rate for Primary BCC | Up to 99% | Variable, often lower |
| Tissue Preservation | High | Variable, often less |
| Margin Control | 100% margin examination | Limited margin examination |
Mohs surgery is a top choice for nose tumors. It’s effective and helps keep the nose looking good.
Standard Excision Techniques for BCC Removal
Removing BCC through standard excision is a careful process. It aims to remove the tumor fully while keeping healthy tissue. This method is key in treating BCC and has a high success rate when done right.
Determining Appropriate Surgical Margins
Finding the right surgical margins is key in BCC removal. The size of the margin depends on the tumor’s size, location, and type. For example, high-risk BCCs need wider margins than low-risk ones. Knowing the difference between high-risk and low-risk is vital for planning the surgery.
| Tumor Risk Category | Recommended Margin |
|---|---|
| Low-risk BCC | 2-3 mm |
| High-risk BCC | 5-10 mm or more |
Step-by-Step Excision Procedure
The excision process has several important steps:
- Preoperative planning, including marking the tumor and planned margins
- Administration of local anesthesia
- Surgical excision of the tumor with the planned margins
- Achieving hemostasis
- Closure of the wound, either directly or with reconstructive techniques
Specimen Handling and Pathology
After the surgery, the removed tissue is sent for examination. This step is vital to confirm the tumor is fully removed. The pathology report will guide further actions, like re-excision if needed.
Proper specimen handling means orienting the tissue correctly and giving the pathologist all necessary information. This ensures accurate margin assessment and diagnosis.
Special Considerations for BCC on Nose Tip
Treating basal cell carcinoma (BCC) on the nose tip is tricky. It’s because of its complex anatomy and how visible it is. It’s important to keep the area safe from cancer while also keeping it looking good.
Anatomical Challenges of the Nasal Tip
The nasal tip has a complex mix of skin, cartilage, and deeper structures. This makes surgery here very challenging. The skin on the nasal tip is thin and tightly stuck to the cartilage underneath, which can lead to problems during and after surgery.
Understanding the nasal tip’s structural nuances is key. Surgeons need to know about the risks and how to avoid them.
Modified Techniques for Nose Tip BCC
Modified techniques like Mohs surgery are used for BCC on the nose tip. Mohs surgery lets surgeons remove tumor tissue carefully while keeping healthy tissue. This is important for keeping the nasal tip looking good.
“Mohs surgery has revolutionized the treatment of skin cancers, including BCC on the nose tip, by providing a highly effective and tissue-sparing approach.” – Dermatologic Surgeon
A study showed Mohs surgery works better than standard excision for BCC on the nose tip. It has fewer recurrences and better looks.
| Treatment Method | Recurrence Rate | Cosmetic Outcome |
|---|---|---|
| Mohs Surgery | 1% | Excellent |
| Standard Excision | 5% | Good |
Preserving Aesthetic Outcomes
Keeping the nose tip looking good after removing BCC is very important. Surgeons use different methods to reduce scarring and keep the nose tip’s natural look. They do this by closing wounds carefully and using local flaps or grafts when needed.
By using these methods, we can get the best look while making sure the BCC is removed. Advanced surgery and knowing the nasal tip’s anatomy help us give our patients the best care.
Immediate Post-Excision Wound Assessment
Right after removing basal cell carcinoma, we assess the wound. This helps us figure out the best way to treat it next.
Wound Size and Depth Evaluation
Checking the wound’s size and depth is key. We measure its length, width, and depth to see how much tissue is lost. This tells us how to fix it.
We measure in centimeters, looking at the longest side and width. We also check how deep the wound is, looking at skin, fat, and sometimes bone.
Determining Reconstruction Needs
After assessing the wound, we decide if reconstruction is needed. This choice depends on the wound’s size, depth, and where it is, along with the patient’s health and wishes.
We have many ways to fix the wound, from simple stitches to more complex skin grafts or flaps. We think about the available tissue, how it looks, and how it works when choosing the best method.
| Wound Characteristics | Reconstruction Options |
|---|---|
| Small, superficial wounds | Primary closure or simple dressings |
| Moderate-sized wounds with some tissue loss | Local flap reconstruction or skin grafting |
| Large, complex wounds with significant tissue loss | Complex reconstruction involving multiple techniques |
Temporary Wound Management Options
While we plan the final fix, we need to take care of the wound first. We use dressings, cleanings, and creams to help it heal and avoid problems.
These steps include:
- Moist dressings to help healing
- Antimicrobial treatments to fight off infection
- Wound cleansings to remove dirt and germs
These temporary steps keep the wound healthy until we do the planned reconstruction.
Reconstruction Options After Basal Cell Carcinoma Removal
Removing basal cell carcinoma often means you need to fix the look and function of your nose. The choice of how to do this depends on the size and where the damage is, and your health.
Primary Closure Techniques
Primary closure is a simple way to fix the wound by sewing it shut. It usually looks better and works for small holes.
Advantages: It’s a simple process and leaves less scar.
Limitations: It only works for small holes and can put stress on the wound.
Local Flap Procedures
Local flap procedures move skin from nearby to cover the hole. This is good for medium-sized holes.
- Bilobed flaps are great for fixing the nose tip.
- Nasolabial flaps work well for holes near the nose’s edge.
Skin Grafting Methods
Skin grafting takes skin from one place and puts it on the hole. It’s best for big holes.
Types of Skin Grafts:
- Full-thickness grafts look better.
- Split-thickness grafts are more flexible but might feel different.
Complex Reconstruction for Large Defects
For really big holes, you need complex methods. These might include local flaps, skin grafts, and more.
| Reconstruction Method | Defect Size | Aesthetic Outcome |
|---|---|---|
| Primary Closure | Small | Excellent |
| Local Flap | Moderate | Good |
| Skin Grafting | Large | Variable |
| Complex Reconstruction | Extensive | Good to Excellent |
Skin Graft Techniques for Nose Reconstruction
The art of nose reconstruction through skin grafting is a mix of technical skill and aesthetic sense. It aims to restore the natural look of the nose. We use skin grafting for various defects, like those from basal cell carcinoma removal. Our approach depends on the size and location of the defect.
Full-Thickness vs. Split-Thickness Grafts
In nose reconstruction, choosing between full-thickness and split-thickness grafts is key. Full-thickness grafts are preferred for smaller defects because they look better and contract less. Split-thickness grafts, which include the top skin layer and part of the dermis, are better for larger areas. They have a higher chance of successful grafting.
| Graft Type | Characteristics | Preferred Use |
|---|---|---|
| Full-Thickness | Includes all skin layers, better cosmetic outcome | Smaller defects |
| Split-Thickness | Includes epidermis and part of dermis, higher graft take success | Larger areas |
Donor Site Selection and Preparation
Choosing the right donor site is essential for graft success. We look at skin color, texture, and thickness to match the recipient site. Common donor sites are the pre-auricular area, supraclavicular area, and inner arm. The donor site must be clean, sterile, and free of any issues that could harm the graft.
Graft Harvesting and Placement Procedure
Harvesting the graft means carefully removing it from the donor site without damaging the surrounding tissue. The graft is then trimmed to fit and any excess tissue is removed. It’s placed on the recipient site using sutures or other methods to ensure it’s in close contact with the underlying tissue.
Ensuring Graft Survival and Integration
To help the graft survive and integrate, we focus on creating the best conditions. This includes keeping the wound clean and stable, ensuring good blood flow to the recipient site, and following proper postoperative care. Patients are also advised to avoid smoking and other factors that could harm the graft. For more on basal cell carcinoma removal, like Mohs surgery, check out additional resources.
Local Flap Procedures for Nasal Reconstruction
After removing basal cell carcinoma, local flap procedures are often used to rebuild the nose. These methods are key to making the nose look and work right again. We’ll look at different local flap procedures, like bilobed, nasolabial, and forehead flaps.
Bilobed Flaps: Design and Execution
Bilobed flaps are great for fixing small to medium-sized nose defects. They have two parts: one part is the same size as the defect, and the other is a bit smaller. Getting the bilobed flap right is all about careful planning and doing it well. This ensures the flap fits the defect without too much tension.
To design a bilobed flap, you need to:
- Check the size and spot of the defect
- Make the first lobe the same size as the defect
- Create the second lobe at a 90-degree angle to the first
- Put the flap in place and tie it down with stitches
Nasolabial Flaps: Step-by-Step Approach
Nasolabial flaps are good for fixing defects on the nose’s ala or sidewall. They’re made along the nasolabial fold, which is good for areas with loose skin.
Here’s how to do a nasolabial flap:
- Draw the flap along the nasolabial fold
- Take the flap up, making sure to keep the blood supply underneath
- Turn the flap into the defect and tie it down
- Fix the donor site to hide the scar
Forehead Flaps for Larger Defects
Forehead flaps are strong for big defects or when other flaps won’t work. They give a lot of tissue and can fix complex nose defects.
Using forehead flaps means:
- Designing the flap on the forehead, thinking about blood supply
- Taking the flap to the nose defect
- Splitting the flap later to free the pedicle
- Fixing the flap and donor site for the best look
Flap Monitoring and Aftercare
After the flap surgery, watching the flap and taking care of it is very important. This helps the flap stay alive and look good. This includes:
- Checking the flap’s blood flow and health often
- Keeping the flap moist and safe
- Avoiding too much pressure or harm to the flap
- Going to follow-up visits to check healing and remove stitches
By planning and doing local flap procedures well, we can get great results in rebuilding the nose. This makes the nose look and work right again.
Postoperative Care and Complications Management
Effective postoperative care is key to avoiding complications and helping wounds heal after basal cell carcinoma removal. We know the postoperative period can be tough for patients. Our goal is to give them the best care possible, meeting their needs and ensuring the best results.
Immediate Postoperative Instructions
Right after surgery, patients get clear instructions on wound care, pain management, and watching for complications. We stress the importance of keeping the wound clean and dry. We also tell them to avoid hard activities and keep their follow-up appointments.
They learn how to handle side effects like swelling and bruising. We suggest using cold compresses and elevating the head to lessen swelling.
Wound Care Protocol
Good wound care is vital for healing and preventing infection. We give patients a wound care plan. This includes cleaning with saline solution, applying topical antibiotics, and using a dressing.
Here’s our standard wound care plan:
| Day | Wound Care Instructions |
|---|---|
| 1-2 | Keep the wound dry and covered with a dressing. |
| 3-5 | Gently clean the wound with saline solution and apply topical antibiotic ointment. |
| 6 and beyond | Continue cleaning and applying antibiotic ointment until the wound is fully healed. |
Managing Common Complications
Though rare, complications can happen after basal cell nose surgery. We watch for signs of infection, bleeding, or wound dehiscence. If any issues come up, we act fast to fix them and prevent more problems.
Here are some common complications and how we manage them:
- Infection: We prescribe antibiotics for infection. We also teach patients to watch for signs like increased redness, swelling, or fever.
- Bleeding: We tell patients to apply gentle pressure to stop bleeding. If bleeding doesn’t stop, we might need to cauterize the area.
- Wound Dehiscence: If the wound opens up, we might need to re-suture it or use other methods to help it heal.
Follow-up Schedule and Long-term Monitoring
Regular follow-up appointments are key for checking on healing and catching any complications early. We schedule these appointments at 1 week, 1 month, 3 months, and 6 months after surgery.
At these visits, we check on the wound’s healing, remove sutures or dressings, and answer any questions. Long-term monitoring is also important to catch any signs of recurrence or new skin cancers.
Conclusion
Basal cell nose surgery is a complex procedure. It needs a detailed approach for the best results. We talked about understanding basal cell carcinoma of the nose, pre-surgery checks, and different surgery methods like Mohs surgery.
Rebuilding the nose after surgery is key. We discussed how to restore the nose’s look and function. This includes skin grafts and local flap procedures.
Good care after surgery and managing any issues are also important. A team effort is needed. Dermatologists, surgeons, and others work together for top-notch care.
FAQ
What is basal cell carcinoma on the nose, and how is it diagnosed?
Basal cell carcinoma on the nose is a type of skin cancer. It can appear in different ways. Doctors use a physical exam, medical history, and imaging to diagnose it.
What are the risk factors for developing basal cell carcinoma on the nose?
UV exposure, fair skin, and a history of skin cancer increase your risk. Knowing these can help you prevent it.
What is Mohs surgery, and how is it used to treat basal cell carcinoma on the nose?
Mohs surgery removes the tumor in stages. The tissue is checked right away to make sure it’s all gone. It’s very effective for nose tumors.
What are the benefits of Mohs surgery for treating basal cell carcinoma on the nose?
Mohs surgery has a high success rate. It also causes less damage to the surrounding area. This makes it great for preserving the nose’s look.
What reconstruction options are available after basal cell carcinoma removal on the nose?
You can choose from several options like primary closure, local flaps, skin grafts, or complex reconstruction. The right choice depends on the defect size and your health.
What is the difference between full-thickness and split-thickness skin grafts?
Full-thickness grafts take the whole skin layer. Split-thickness grafts only take a part of it. The choice depends on the defect size and your health.
How is postoperative care managed after basal cell nose surgery?
Post-op care includes following immediate instructions, wound care, managing complications, and regular check-ups. It aims to ensure healing and the best results.
What are the common complications after basal cell nose surgery, and how are they managed?
Complications like infection, bleeding, and scarring can happen. They are managed by recognizing them early, treating them, and following up to ensure the best outcome.
How can I prevent basal cell carcinoma on the nose?
To prevent it, reduce UV exposure by using sunscreen, wearing protective clothes, and staying in the shade. People with fair skin or a history of skin cancer should be extra careful.
What is the importance of early detection in treating basal cell carcinoma on the nose?
Early detection is key for better treatment outcomes. Regular skin checks and quick evaluation of suspicious spots can catch basal cell carcinoma early.
What is the role of imaging techniques in diagnosing basal cell carcinoma on the nose?
Imaging like ultrasound and MRI helps diagnose basal cell carcinoma. They show how big the tumor is and help plan treatment.
How is the need for reconstruction determined after basal cell carcinoma removal on the nose?
The need for reconstruction depends on the wound size and depth, and your overall health. The goal is to restore the nose’s look and function
References:
- The Skin Cancer Foundation. (n.d.). Mohs surgery – The Skin Cancer Foundation. https://www.skincancer.org/treatment-resources/mohs-surgery/
- NCBI Bookshelf. (n.d.). Mohs micrographic surgery – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK441833/
- University of Mississippi Medical Center. (n.d.). Preoperative information for Mohs surgery patients. https://umc.edu/Healthcare/ENT/Patient-Handouts/Adult/PSCSC/Mohs_preop.html





