Last Updated on October 21, 2025 by mcelik

We are seeing a big change in how we treat cancer with CAR T-cell therapy. This new way uses your own immune cells to fight cancer.
This immunotherapy CAR T method changes T cells to find and kill cancer cells. It gives new hope to patients, mainly those with tough-to-treat blood cancer types.
At Liv Hospital, we know how important it is to understand CAR-T cell therapy, CAR T cell infusion, and possible side effects. We want to make sure patients get the best care.
Key Takeaways
- CAR T-cell therapy is a personalized form of immunotherapy.
- It targets and destroys cancer cells.
- The treatment involves genetically modifying T cells.
- Understanding the process and possible side effects is key.
- Liv Hospital offers full care for patients getting CAR T-cell therapy.
What Is CAR T Cancer Treatment: The Breakthrough Explained

CAR T-cell therapy uses the immune system to fight cancer. It changes a patient’s T cells to find and kill cancer cells. This makes it a personalized medicine that fits each patient’s needs.
The Science Behind Chimeric Antigen Receptors
CAR T-cell therapy uses chimeric antigen receptors (CARs) to target cancer cells. These receptors are made to find specific proteins on cancer cells. This lets T cells destroy them.
To make this happen, T cells are taken from the blood, changed to have CARs, and then put back in the patient.
How Immunotherapy CAR T Transforms Cancer Care
CAR T-cell therapy is a big step forward in immunotherapy. It gives hope to patients with blood cancers that other treatments can’t help. It uses the immune system to target cancer, harming fewer healthy cells and causing less side effects.
Because CAR T cells can find and kill cancer cells, it’s a strong tool against cancer. As research grows, CAR T-cell therapy might help more cancers, changing cancer care even more.
The Evolution of CAR T-Cell Therapy in Modern Oncology

CAR T-cell therapy has changed the face of modern oncology. It brings new hope to those with certain blood cancers. This treatment uses the body’s immune system to attack cancer cells.
Historical Development and Milestones
The idea of CAR T-cell therapy started in the early 1990s. But it wasn’t until 2017 that the FDA gave it its first approval. This was a big step forward for treating children with acute lymphoblastic leukemia (ALL).
Ever after, CAR T-cell therapy has kept growing. New research and trials have made it work better and safer for more patients.
Current FDA Approvals for Blood Cancers
Today, CAR T-cell therapy is approved by the FDA for some blood cancers. This includes certain lymphomas and leukemias. It shows promise for patients who haven’t responded to other treatments.
| Indication | Product Name | Manufacturer | Approval Year |
|---|---|---|---|
| Relapsed or refractory large B-cell lymphoma | Yescarta | Kite Pharma/Gilead | 2017 |
| Relapsed or refractory large B-cell lymphoma | Breyanzi | Bristol Myers Squibb | 2021 |
| Relapsed or refractory mantle cell lymphoma | Breyanzi | Bristol Myers Squibb | 2021 |
The table shows some FDA approvals for CAR T-cell therapy. These approvals show how important CAR T-cell therapy is in modern oncology. It offers targeted treatments for patients with few other options.
The Complete CAR T Process: From Collection to Infusion
The journey of CAR T-cell therapy starts with collecting a patient’s T cells. This is done through a process called apheresis. It’s key because it gives the T cells needed to fight cancer.
T Cell Collection Through Apheresis
Apheresis separates T cells from other blood parts. The patient’s blood goes into a special machine. It keeps the T cells and returns the rest to the patient.
Genetic Engineering in the Laboratory
After collecting T cells, they go to a lab for genetic engineering. Here, they get chimeric antigen receptors (CARs) on their surface. This helps them find and attack cancer cells better.
Genetic modification is complex and needs advanced technology.
For more info on CAR T-cell therapy, check out the National Cancer Institute. They offer detailed insights and research updates.
Cell Multiplication and Quality Control
After engineering, CAR T cells multiply in the lab. This is to get enough cells for treatment. Before returning to the patient, they go through quality control.
This ensures they are safe and work well.
The CAR T process is designed to be safe and effective. Knowing each step helps patients understand the innovation behind this cancer treatment.
Patient Preparation for CAR T Cancer Treatment
Getting ready for CAR T cancer treatment is key to a good outcome. It’s important to prepare well to make this therapy work best. Let’s look at what steps you need to take.
Comprehensive Pre-Treatment Evaluation
Before starting CAR T cell therapy, you’ll have a detailed check-up. This check-up looks at your health and how much cancer you have. It includes:
- A thorough medical history review
- Physical examination
- Laboratory tests, including blood counts and chemistry panels
- Imaging studies, such as CT scans or PET scans
- Cancer-specific tests to evaluate the extent of disease
This detailed check-up helps doctors see if CAR T cell therapy is right for you. It also finds any problems that need fixing before treatment.
Lymphodepletion Chemotherapy Protocol
Getting ready for CAR T cell infusion means going through lymphodepletion chemotherapy. This treatment uses chemotherapy to:
- Lower the number of lymphocytes in your body
- Make room for the CAR T cells to grow and work well
Lymphodepletion chemotherapy usually lasts a few days. It’s usually okay to take. The exact plan might change based on where you’re getting treated and your specific needs.
Setting Realistic Expectations and Timeline
It’s important to know what to expect from CAR T treatment and how long it will take. From the first check-up to getting the CAR T cells, it can take weeks to months. You should be ready for:
- Possible side effects from lymphodepletion chemotherapy
- The chance of staying in the hospital during or after CAR T cell infusion
- Time to recover and be watched after treatment
Knowing the process and timeline helps you prepare. It lets you make smart choices about your care.
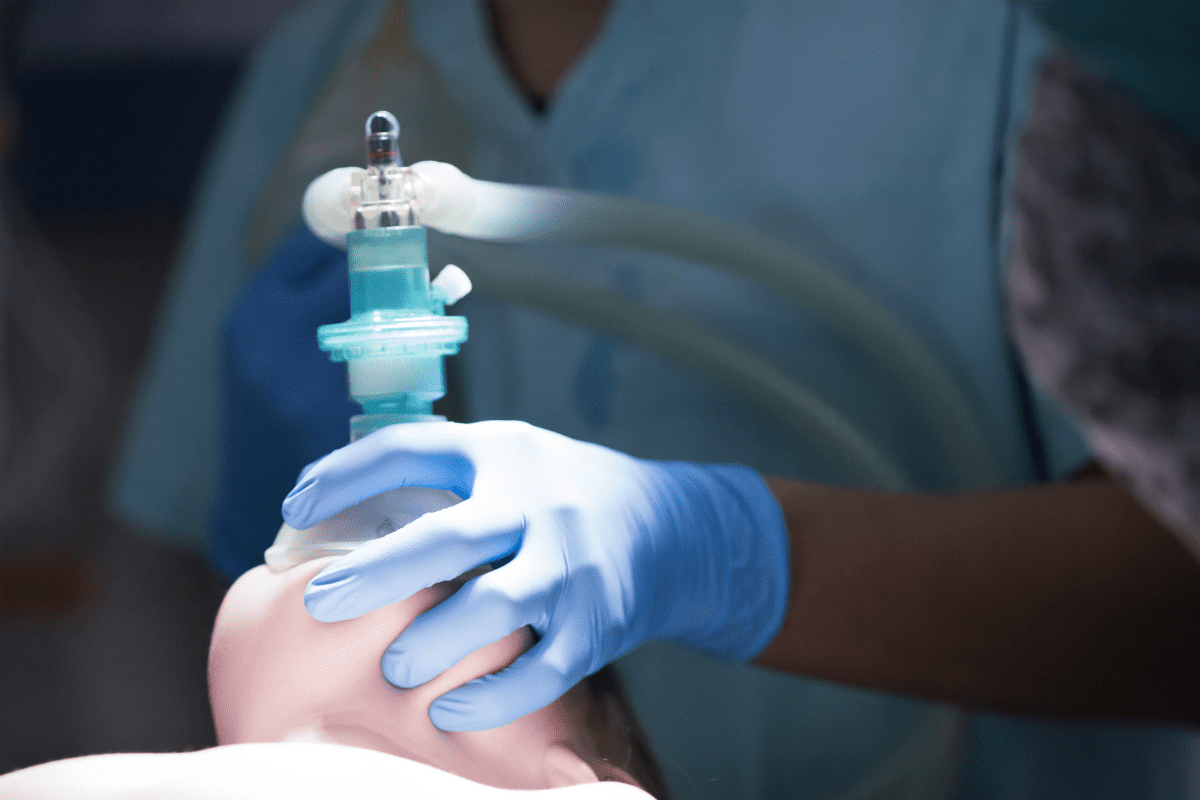
The CAR T Cell Infusion Experience
Infusion day is when CAR T cells, made to fight cancer, are given to the patient. This is the end of a detailed process. It started with taking T cells from the patient’s blood.
What Happens on Infusion Day
On infusion day, patients go to the treatment center for preparation. The CAR T cell infusion process is relatively quick, taking 30 to 60 minutes.
Before the infusion, the medical team checks the patient’s condition. They look at their health and test results.
The 30-60 Minute Infusion Procedure
The actual infusion of CAR T cells is simple. The cells are given through an intravenous line, like a blood transfusion. Patients are watched closely during this time for any immediate reactions.
Immediate Post-Infusion Monitoring Requirements
After the infusion, patients are watched for side effects. This is key to catch and manage any problems, like cytokine release syndrome.
Post-infusion care is a critical part of CAR T cell therapy. Patients often stay near the treatment center for days. This ensures they can get help quickly if needed.
Understanding CAR-T Side Effects and Complications
CAR T-cell therapy brings new hope for cancer patients. But, it’s important to know the possible complications and side effects. Let’s explore this innovative treatment and its effects on patients.
Cytokine Release Syndrome: Symptoms and Severity
Cytokine Release Syndrome (CRS) is a major side effect of CAR T-cell therapy. It happens when CAR T cells release a lot of cytokines into the blood. This can lead to a serious condition.
CRS symptoms can vary from mild to severe. They include:
- Fever
- Fatigue
- Nausea and vomiting
- Headache
- Muscle pain
- Low blood pressure
CRS is graded from 1 to 4, with 1 being mild and 4 being severe. Patients with CRS need close monitoring. Sometimes, they need medication like tocilizumab.
Neurological Events and ICANS
Neurological events, including Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), are also common. ICANS can cause mild symptoms like confusion or more severe ones like seizures.
ICANS symptoms can be divided into several areas. These include:
- Cognitive changes
- Language disturbances
- Motor weakness
- Seizures
It’s important to recognize and manage ICANS early to avoid long-term damage.
Other Possible Complications
Patients may also face other complications. These include:
- Infections due to weakened immune system
- Hemophagocytic lymphohistiocytosis (HLH)
- Tumor lysis syndrome
- B cell aplasia and hypogammaglobulinemia
Knowing about these complications helps in providing better care to patients undergoing CAR T-cell therapy.
| Complication | Symptoms | Management |
|---|---|---|
| Cytokine Release Syndrome (CRS) | Fever, fatigue, nausea, headache, low blood pressure | Tocilizumab, corticosteroids, supportive care |
| Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) | Confusion, language difficulties, motor weakness, seizures | Corticosteroids, supportive care, seizure prophylaxis |
| Infections | Varies depending on the type of infection | Antibiotics, antivirals, antifungals, supportive care |
Managing and Treating CAR-T Side Effects
CAR T-cell therapy is a game-changer but comes with side effects. It’s important to know how to handle these to help patients. This knowledge is key for their care and success in treatment.
Early Recognition and Intervention
Spotting CAR-T side effects early is vital. We watch patients for cytokine release syndrome (CRS) and neurological issues. Quick action helps improve their chances of recovery.
CRS needs fast attention because it can be serious. We use tests and doctor checks to find and treat CRS quickly.
Tocilizumab and Steroid Protocols
Tocilizumab, an IL-6 receptor antagonist, is key in fighting CRS. We give it to patients with grade 2 or higher CRS. Steroids help with neurological side effects and when tocilizumab doesn’t work.
We balance treating side effects with keeping CAR-T therapy effective. We adjust tocilizumab and steroid doses based on side effects and patient response.
Supportive Care Strategies
Supportive care is essential for CAR-T side effects. We use inpatient monitoring, symptom management, and infection prevention. These steps help patients a lot.
By recognizing side effects early, using tocilizumab and steroids, and providing supportive care, we can manage CAR-T side effects well. This improves patient outcomes and quality of life.
Efficacy and Success Rates of White Blood Cell Therapy
CAR T-cell therapy has changed how we treat blood cancers. We look at how well this therapy works for different blood cancers. We focus on remission rates and how patients do.
Remission Rates in B-Cell Lymphomas
CAR T-cell therapy is very effective against B-cell lymphomas. Many patients see their cancer go into complete remission. This is a big win for those with relapsed or refractory B-cell lymphoma.
A study in the Journal of Clinical Oncology found impressive results. It showed that 50% to 80% of patients with diffuse large B-cell lymphoma got complete remission with CAR T-cell therapy.
Response in Multiple Myeloma Patients
Multiple myeloma patients also see good results with CAR T-cell therapy. Clinical trials show that CAR T-cell therapy targeting BCMA works well. It helps even those who have tried many treatments before.
A recent study in Table 1 shows how well CAR T-cell therapy works for multiple myeloma patients.
| Treatment Outcome | Percentage of Patients |
|---|---|
| Complete Response | 40% |
| Partial Response | 30% |
| Stable Disease | 15% |
| Progressive Disease | 15% |
Outcomes in Acute Lymphoblastic Leukemia
CAR T-cell therapy is also effective against acute lymphoblastic leukemia (ALL). It works best in pediatric patients. Clinical trials show high remission rates, giving hope to those with relapsed or refractory ALL.
A study in the New England Journal of Medicine found over 90% complete remission in pediatric ALL patients. This is a huge success for CAR T-cell therapy.
Life After CAR T Transplant: Recovery and Follow-Up
The journey doesn’t end with CAR T-cell infusion; it’s just the start of a new chapter. After CAR T-cell therapy, patients need careful monitoring and follow-up care. We guide patients through this, covering short-term and long-term needs.
Short-Term Recovery Expectations
Patients will be closely watched for side effects like cytokine release syndrome (CRS) and neurological events. CRS can cause symptoms like fever, fatigue, and nausea. Our team works hard to manage these side effects.
Right after the infusion, patients usually stay in the hospital for close monitoring. The team checks for CRS and other complications, acting quickly if needed. Patients also learn to spot symptoms that need immediate medical help.
| Symptom | Severity | Action |
|---|---|---|
| Fever | Mild to Severe | Monitor temperature; report to healthcare provider if persistent |
| Fatigue | Moderate to Severe | Rest; maintain hydration; report to healthcare provider if worsening |
| Nausea | Mild to Moderate | Take anti-nausea medication; report to healthcare provider if severe |
Long-Term Monitoring Protocol
Long-term care is key for CAR T-cell therapy patients. Regular check-ups help monitor for relapse, check immune function, and manage side effects. We also watch for long-term issues like infections or secondary cancers.
Our long-term plan includes:
- Regular blood tests to check for signs of relapse or infection
- Imaging studies as needed to assess disease status
- Assessment of immune function to ensure recovery
Quality of Life Considerations
Quality of life is very important for patients after CAR T-cell therapy. They may face physical, emotional, and social challenges. Our support team helps manage these through care and resources.
We encourage patients to:
- Maintain a healthy lifestyle, including a balanced diet and regular exercise
- Seek emotional support from family, friends, or mental health professionals
- Stay connected with support groups to share experiences and advice
By providing full care and support, we help patients achieve the best outcomes and improve their quality of life after CAR T-cell therapy.
Cost and Access to CAR-T Therapy in the United States
Understanding the cost of CAR-T therapy is key for patients. It’s important to know how much it costs and how to get it. We’ll look at the factors that affect its price.
Treatment Costs and Insurance Coverage
CAR-T therapy is very expensive, often costing hundreds of thousands of dollars. This includes the therapy and the care needed during and after treatment. Insurance coverage can vary a lot.
Key factors influencing insurance coverage include:
- The specific CAR-T therapy product used
- The patient’s insurance plan and provider
- The medical necessity of the treatment as determined by healthcare providers
Patient Assistance Programs
There are programs to help with the cost of CAR-T therapy. These programs offer financial help and support with insurance claims. They can also help with treatment costs.
Companies that make CAR-T therapies have patient assistance programs. Also, non-profit organizations for cancer support may offer grants or other help to patients.
Certified Treatment Centers
CAR-T therapy is given at certified treatment centers. These centers have the right skills and setup for this complex treatment. They can handle the infusion and manage side effects.
Choosing a certified treatment center is important. They provide top-notch care and help with insurance and financial help.
Conclusion: The Future of CAR T Cancer Treatment
CAR T-cell therapy is getting better, with new research to make it more effective. This therapy has changed how we treat some blood cancers. It gives hope to patients who have tried other treatments without success.
Future studies aim to lessen side effects and make the treatment work better for more people. They also want to see if it can help with solid tumors. As research goes on, CAR T-cell therapy might become even more common and successful, changing cancer care.
Healthcare experts and researchers are leading the way in these advancements. They are working together to make CAR T cancer treatment better. This could greatly improve the lives of patients all over the world.
What is CAR T-cell therapy?
CAR T-cell therapy is a way to fight cancer using the body’s immune system. It starts by taking T cells from the patient. Then, these T cells are changed to find and kill cancer cells. After that, they are put back into the patient.
How does CAR T-cell therapy work?
It works by adding special receptors to T cells. These receptors help T cells find and attack cancer cells. This way, the T cells can destroy the cancer cells.
What types of cancer can be treated with CAR T-cell therapy?
It’s approved for some blood cancers. These include B-cell lymphomas, multiple myeloma, and acute lymphoblastic leukemia.
What is the process of CAR T-cell therapy?
The process includes several steps. First, T cells are collected. Then, they are changed in the lab to add CARs. Next, they multiply and go through quality checks. After that, chemotherapy is given to prepare the body. Lastly, the CAR T cells are infused back into the patient.
What are the possible side effects of CAR T-cell therapy?
Side effects can include cytokine release syndrome (CRS) and neurological problems. Other issues might be infections and low blood cell counts.
How are CAR T-cell therapy side effects managed?
Side effects are managed by recognizing them early and treating them. Tocilizumab and steroids are used to reduce CRS and ICANS. Supportive care helps with other problems.
What is the success rate of CAR T-cell therapy?
Success rates vary by cancer type. For some blood cancers, it has shown good results. Patients have seen significant improvements.
How long does it take to recover from CAR T-cell therapy?
Recovery time varies. Patients usually need short-term hospital care after infusion. They also need long-term follow-up to manage side effects and watch for disease return.
What is the cost of CAR T-cell therapy?
The cost is high, but help is available. Insurance and patient assistance programs can make it more affordable.
Where can I find certified treatment centers for CAR T-cell therapy?
You can find certified centers through the FDA’s list and cancer care organizations. They provide CAR T-cell therapy.
Is CAR T-cell therapy a one-time treatment?
It’s usually a single infusion. But, some patients might need more treatments or ongoing care based on their response and disease status.
Can CAR T-cell therapy be used in combination with other cancer treatments?
Yes, it can be used with other treatments. This includes chemotherapy or targeted therapy. It’s part of a complete treatment plan.