Last Updated on October 21, 2025 by mcelik
Bone marrow disorders can really change how you live your life. It’s important to know about the different conditions that affect how your bone marrow makes healthy blood cells. At Liv Hospital, we are committed to providing complete care for those with bone marrow issues. We make sure they get the best treatment for their specific problem.
We will look at many bone marrow conditions, like aplastic anemia, myelodysplastic syndromes, and multiple myeloma. We will show our skill in finding and treating these complex problems. Knowing about the different bone marrow diseases is key for good diagnosis and treatment.
Key Takeaways
- Understanding bone marrow disorders is key for good diagnosis and treatment.
- Liv Hospital offers complete care for patients with bone marrow conditions.
- Bone marrow diseases cover a wide range of conditions that affect blood cell production.
- Early diagnosis is vital for managing bone marrow disorders well.
- Liv Hospital is dedicated to delivering top-notch healthcare with international patient support.
Understanding Bone Marrow and Its Function
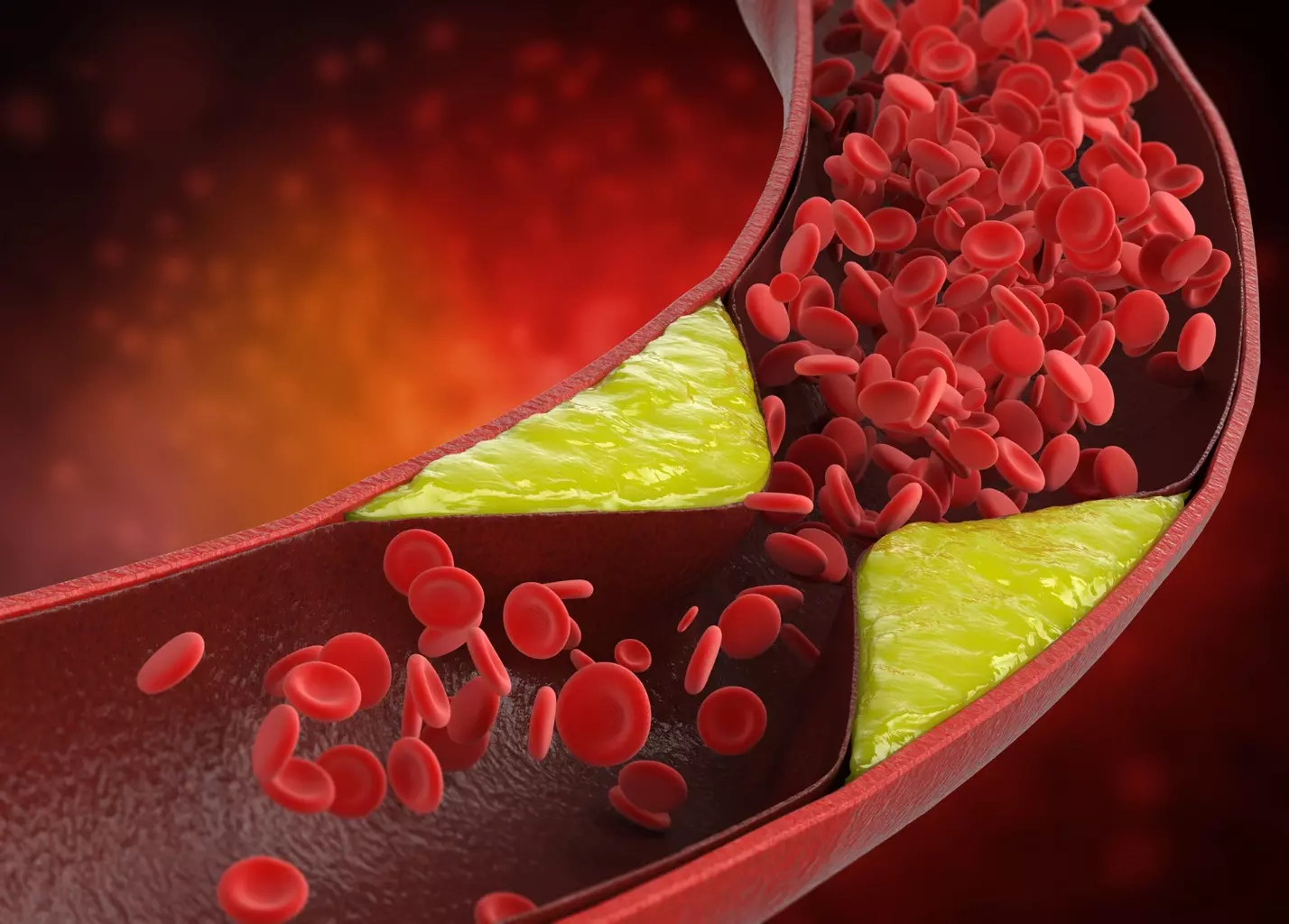
Bone marrow is more than just a part of our bones. It’s a factory that makes the blood cells we need. These cells help carry oxygen, fight off infections, and stop bleeding. To understand bone marrow diseases, we must first know its role in our body.
What Is Bone Marrow?
Bone marrow is the soft tissue inside bones like the hips and thighbones. It’s filled with stem cells, which turn into different blood cells. This tissue is key to our health.
How Bone Marrow Produces Blood Cells
In the bone marrow, stem cells turn into red blood cells, white blood cells, and platelets. Red blood cells carry oxygen, white blood cells fight infections, and platelets help blood clot. This process is vital for our health.
The creation of blood cells is carefully controlled. Growth factors and cytokines keep the right balance of blood cells. Any problem in this balance can cause bone marrow disorders.
Types of Bone Marrow: Red vs. Yellow
There are two types of bone marrow: red and yellow. Red bone marrow is where blood cells are made, full of blood vessels and stem cells. Yellow bone marrow is mostly fat and less active in adults, but can turn into red marrow when needed.
- Red Bone Marrow: Makes blood cells, has lots of blood vessels and stem cells.
- Yellow Bone Marrow: Mainly fat, less active in making blood cells, but can change to red marrow when needed.
Knowing the difference between red and yellow bone marrow helps us understand bone marrow diseases. The balance between these types and their functions is essential for our health.
Blood Marrow Diseases: Classification and Overview

We will look at the different types of bone marrow disorders. We’ll talk about how common they are and what increases your risk. Bone marrow diseases affect blood cell production and function, causing health problems.
Definition and Categories of Bone Marrow Disorders
Bone marrow disorders fall into several categories. These include aplastic anemia, myelodysplastic syndromes, myeloproliferative neoplasms, leukemia, lymphoma, and multiple myeloma. Each category has its own unique characteristics.
Knowing how to classify these disorders is key. It helps doctors choose the right treatment and understand what to expect. This way, they can give better care and find the best ways to help patients.
Prevalence and Statistics in the United States
Bone marrow disorders are common in the United States. For example, multiple myeloma causes over 36,000 new cases every year. Acute leukemias also affect many people, showing the importance of early treatment.
| Disease | Annual Incidence (US) |
|---|---|
| Multiple Myeloma | 36,000+ |
| Acute Leukemias | Tens of thousands |
| Myelodysplastic Syndromes | Approximately 10,000 |
Common Risk Factors for Developing Bone Marrow Conditions
Several things can increase your risk of getting bone marrow disorders. These include genetics, exposure to harmful chemicals, past treatments like chemotherapy, and some viruses. Knowing these risk factors helps with early detection and prevention.
By understanding the risk factors and how bone marrow disorders are classified, we can improve diagnosis and treatment. This helps patients get better care and outcomes.
Aplastic Anemia: When Bone Marrow Stops Producing Blood Cells
Aplastic anemia happens when the bone marrow can’t make enough blood cells. This leads to tiredness, infections, and bleeding problems. It’s when the bone marrow can’t make enough red blood cells, white blood cells, and platelets.
Causes and Mechanisms
There are many reasons aplastic anemia can occur. It might be due to toxins, certain medicines, viral infections, or autoimmune diseases. Sometimes, the exact cause is not known.
Toxins and Chemicals: Exposure to harmful chemicals like pesticides can increase the risk of aplastic anemia. These chemicals can harm the bone marrow, making it hard to produce blood cells.
Medications: Some medicines, like antibiotics and anti-inflammatory drugs, can cause aplastic anemia. This happens when the bone marrow reacts badly to the medicine.
Symptoms and Diagnostic Approaches
The symptoms of aplastic anemia include tiredness, infections, and easy bleeding. These happen because there are not enough blood cells.
To diagnose aplastic anemia, doctors use blood tests and bone marrow biopsies. Blood tests show low counts of blood cells. A bone marrow biopsy checks how well the bone marrow is working.
Treatment Options and Prognosis
Treatment for aplastic anemia depends on how severe it is and what caused it. It can include blood transfusions or medicines to help the bone marrow. In some cases, a bone marrow transplant is needed.
The outlook for people with aplastic anemia varies. With the right treatment, some see big improvements. Others need ongoing care. We’ll look at the latest treatments and their results to understand how to manage aplastic anemia better.
Myelodysplastic Syndromes (MDS): Disorders of Blood Cell Production
Myelodysplastic syndromes (MDS) are complex disorders where the bone marrow fails to make healthy blood cells. This failure leads to anemia, infections, and bleeding disorders. These issues greatly affect patients’ quality of life.
Types of Myelodysplastic Syndromes
MDS has several subtypes, each with its own characteristics and outlook. The classification is based on the number of blasts in the bone marrow and genetic abnormalities. The World Health Organization (WHO) system is used to categorize MDS into subtypes.
Risk Factors and Causes
Several factors can lead to MDS, including exposure to chemicals like benzene and radiation. Prior chemotherapy, and certain genetic disorders, also increase the risk. These include Fanconi anemia and dyskeratosis congenita.
Symptoms and Clinical Presentation
Patients with MDS often have symptoms like anemia, neutropenia, and thrombocytopenia. They may feel tired, weak, and short of breath. They also get infections easily and may bleed more due to low platelets.
Treatment Strategies and Management
Treatment for MDS depends on the patient’s subtype, risk, and health. Supportive care, like blood transfusions and growth factors, helps manage symptoms. For those at higher risk, treatments like immunosuppressive therapy, chemotherapy, or stem cell transplantation may be considered. These treatments aim to cure the disease.
Myeloproliferative Neoplasms: When Blood Cells Overproduce
Myeloproliferative neoplasms are blood cancers where too many blood cells are made. They start in the bone marrow. This can cause problems like blood clots and can turn into acute leukemia.
Types of Myeloproliferative Disorders
There are several types of myeloproliferative neoplasms. Each has its own features. The main types are:
- Polycythemia Vera (PV): This is when too many red blood cells are made, making blood thicker.
- Essential Thrombocythemia (ET): It’s when too many platelets are made. This can cause blood clots or bleeding.
- Primary Myelofibrosis (PMF): This is when the bone marrow gets scarred. It can cause anemia, a big spleen, and other issues.
Knowing these types helps doctors choose the right treatment.
Symptoms and Progression
Symptoms of myeloproliferative neoplasms vary by type. They often include tiredness, weight loss, and a big spleen. As the disease gets worse, problems like blood clots, bleeding, or turning into acute myeloid leukemia can happen.
Current Treatment Approaches
Treatment for myeloproliferative neoplasms aims to prevent serious problems and ease symptoms. Options include:
| Treatment | Description | Benefits |
|---|---|---|
| Hydroxyurea | Chemotherapy that reduces blood cell production | Reduces risk of thrombosis |
| Interferon | Protein that helps regulate the immune system | Can reduce blood cell count and spleen size |
| JAK Inhibitors | Targeted therapy that blocks specific enzymes | Improves symptoms and reduces spleen size |
We’re always working to improve treatments for myeloproliferative neoplasms. Research is ongoing for new therapies and ways to manage the disease.
Leukemia: Cancer of the Blood and Bone Marrow
Leukemia is a cancer that affects the blood and bone marrow. It happens when abnormal white blood cells grow too much. This disrupts the normal production of blood cells. Leukemia is divided into different types based on the cell involved and how fast it grows.
Acute vs. Chronic Leukemia
Leukemia is either acute or chronic, based on how fast it grows. Acute leukemia grows quickly, causing symptoms fast. Chronic leukemia grows slower, sometimes not causing symptoms for a while.
- Acute Leukemia: Needs quick treatment because it’s aggressive.
- Chronic Leukemia: May not need immediate treatment, focusing on watching the disease.
Different Types of Leukemia
Leukemia is also classified by the cell type affected. The main types are:
- Acute Lymphoblastic Leukemia (ALL): Affects lymphoid cells, common in kids.
- Acute Myeloid Leukemia (AML): Starts in myeloid cells, more in adults.
- Chronic Lymphocytic Leukemia (CLL): Affects lymphoid cells, slow-growing, common in older adults.
- Chronic Myeloid Leukemia (CML): Involves myeloid cells, can grow slowly or fast.
Treatment Innovations and Survival Rates
Leukemia treatment has improved a lot. It now includes chemotherapy, targeted therapy, and hematopoietic stem cell transplantation. The right treatment depends on the leukemia type, patient’s age, and health. Thanks to these advances, survival rates have gone up, with some types having high survival rates if caught early.
Knowing the leukemia type and its outlook is key for the best treatment. We keep seeing new treatments for leukemia, giving hope to patients everywhere.
Lymphoma: When Bone Marrow Involvement Occurs
Lymphoma is divided into Hodgkin and non-Hodgkin types. When it affects the bone marrow, it can be serious. We’ll look at the differences between these types, the effects of bone marrow involvement, and how to diagnose and treat them.
Hodgkin vs. Non-Hodgkin Lymphoma
Hodgkin lymphoma has Reed-Sternberg cells. Non-Hodgkin lymphoma is more common and has many subtypes. Non-Hodgkin lymphoma is more complex to diagnose and treat.
Knowing the type of lymphoma is key for treatment. We’ll talk about Hodgkin and non-Hodgkin lymphoma. We’ll highlight their differences in symptoms and treatment.
Bone Marrow Involvement in Lymphoma
Bone marrow involvement is important in lymphoma staging. It can affect blood cell production and overall health. It can cause anemia, infections, and bleeding problems.
The extent of bone marrow involvement affects treatment choices and outcomes. We’ll look at how it’s assessed and its role in managing lymphoma.
Diagnostic and Treatment Considerations
Diagnosing lymphoma involves imaging, bone marrow biopsy, and histopathology. Treatment depends on the lymphoma type, stage, and patient factors. It may include chemotherapy, radiation, immunotherapy, or a mix.
We’ll discuss current treatments for lymphoma. This includes and new therapies. Understanding diagnosis and treatment is vital for caring for lymphoma patients.
Multiple Myeloma: Cancer of Plasma Cells
Multiple myeloma is a cancer where bad plasma cells grow in the bone marrow. This causes many problems. Plasma cells help fight infections by making antibodies.
Understanding Plasma Cell Disorders
Plasma cell disorders include multiple myeloma. They happen when bad plasma cells build up in the bone marrow. This can cause anemia, bone pain, and more infections.
It’s key to understand these disorders to treat multiple myeloma well. The cancer makes too many bad plasma cells. This leads to problems like making too much of a certain protein.
Symptoms and Complications
The symptoms of multiple myeloma vary. They can include:
- Bone pain, often in the back, ribs, or hips
- Anemia, causing fatigue and weakness
- Recurring infections because the immune system is weak
- Problems with the kidneys
- Too much calcium in the blood
These symptoms come from the tumor, the bad protein, and less normal bone marrow. Spotting these symptoms early is very important.
Diagnostic Criteria and Staging
To diagnose multiple myeloma, doctors use tests and scans. The main signs are:
- More than 10% bad plasma cells in the bone marrow
- Bad protein in the blood or urine
- Problems with organs like the kidneys or bones
Doctors use the Revised International Staging System (R-ISS) to stage the cancer. It looks at several things to see how serious it is.
| R-ISS Stage | Criteria | Median Survival |
|---|---|---|
| I | Serum albumin ≥ 3.5 g/dL, β2-microglobulin | Not specified |
| II | Not stage I or III | Not specified |
| III | β2-microglobulin ≥ 5.5 mg/L and high-risk CA (e.g., del(17p), t(14;16), t(4;14)) | Not specified |
“The diagnosis and staging of multiple myeloma have become increasingly sophisticated, allowing for more personalized treatment approaches.” –
Current Treatment Approaches and Research
Treatment for multiple myeloma has changed a lot. New drugs and ways to treat it have been found. Doctors now use a mix of treatments based on each patient’s needs.
There’s a move towards treating each patient differently. Research into new treatments, like CAR-T cell therapy, is showing great promise. This could lead to better care for people with multiple myeloma.
Key treatment modalities include:
- Proteasome inhibitors (e.g., bortezomib, carfilzomib)
- Immunomodulatory drugs (e.g., lenalidomide, pomalidomide)
- Corticosteroids (e.g., dexamethasone)
- Stem cell transplantation in eligible patients
As research keeps going, we hope to see even better ways to treat multiple myeloma. This will help patients live better and longer.
Genetic Bone Marrow Abnormalities and Inherited Disorders
Understanding genetic bone marrow abnormalities is key to diagnosing and treating related conditions. These disorders come from inherited mutations that harm the bone marrow’s ability to make healthy blood cells. We will look at several genetic bone marrow abnormalities and how to manage them.
Fanconi Anemia: Causes and Management
Fanconi anemia is a rare genetic disorder. It causes bone marrow failure, birth defects, and a higher risk of cancer. It happens because of mutations in genes that help fix DNA. We will talk about its symptoms and why early diagnosis is important.
Managing Fanconi Anemia needs a team effort. This includes bone marrow transplants, supportive care, and watching for cancer. New genetic tests have made diagnosis and treatment more tailored.
Diamond-Blackfan Anemia: A Rare Congenital Disorder
Diamond-Blackfan anemia affects the production of red blood cells. It often comes with physical issues and a higher risk of certain cancers. We will look at the genetic causes and symptoms of this condition.
Treatment for Diamond-Blackfan anemia usually includes steroids and sometimes blood transfusions. Genetic counseling is also important for families dealing with this condition.
Shwachman-Diamond Syndrome
Shwachman-Diamond syndrome is a genetic disorder that affects the bone marrow, pancreas, and other systems. It leads to pancreatic insufficiency and a higher risk of bone marrow failure and leukemia. We will discuss the challenges in diagnosing and managing this complex condition.
Supportive care is a big part of managing Shwachman-Diamond syndrome. This includes replacing pancreatic enzymes and supporting the blood system. It’s also important to watch for signs of bone marrow failure or cancer.
Dyskeratosis Congenita
Dyskeratosis congenita is a rare genetic disorder. It is known for skin hyperpigmentation, nail dystrophy, and oral leukoplakia. It also raises the risk of bone marrow failure and cancer. We will explore the genetic basis and its clinical implications.
Managing dyskeratosis congenita involves regular checks for bone marrow failure and cancer. It also includes hematopoietic stem cell transplantation in some cases. Early diagnosis and a detailed care plan are key to better outcomes.
| Disorder | Key Features | Management Strategies |
|---|---|---|
| Fanconi Anemia | Bone marrow failure, congenital anomalies, cancer risk | Hematopoietic stem cell transplantation, supportive care |
| Diamond-Blackfan Anemia | Red blood cell production failure, physical anomalies | Corticosteroids, blood transfusions |
| Shwachman-Diamond Syndrome | Pancreatic insufficiency, bone marrow failure risk | Pancreatic enzyme replacement, hematologic support |
| Dyskeratosis Congenita | Skin hyperpigmentation, nail dystrophy, oral leukoplakia | Monitoring, hematopoietic stem cell transplantation |
Diagnosis and Treatment Approaches for Bone Marrow Disorders
Bone marrow disorders are tricky to diagnose. They need advanced tests. Accurate diagnosis is key for effective treatment. We’ll look at how to diagnose and treat these disorders.
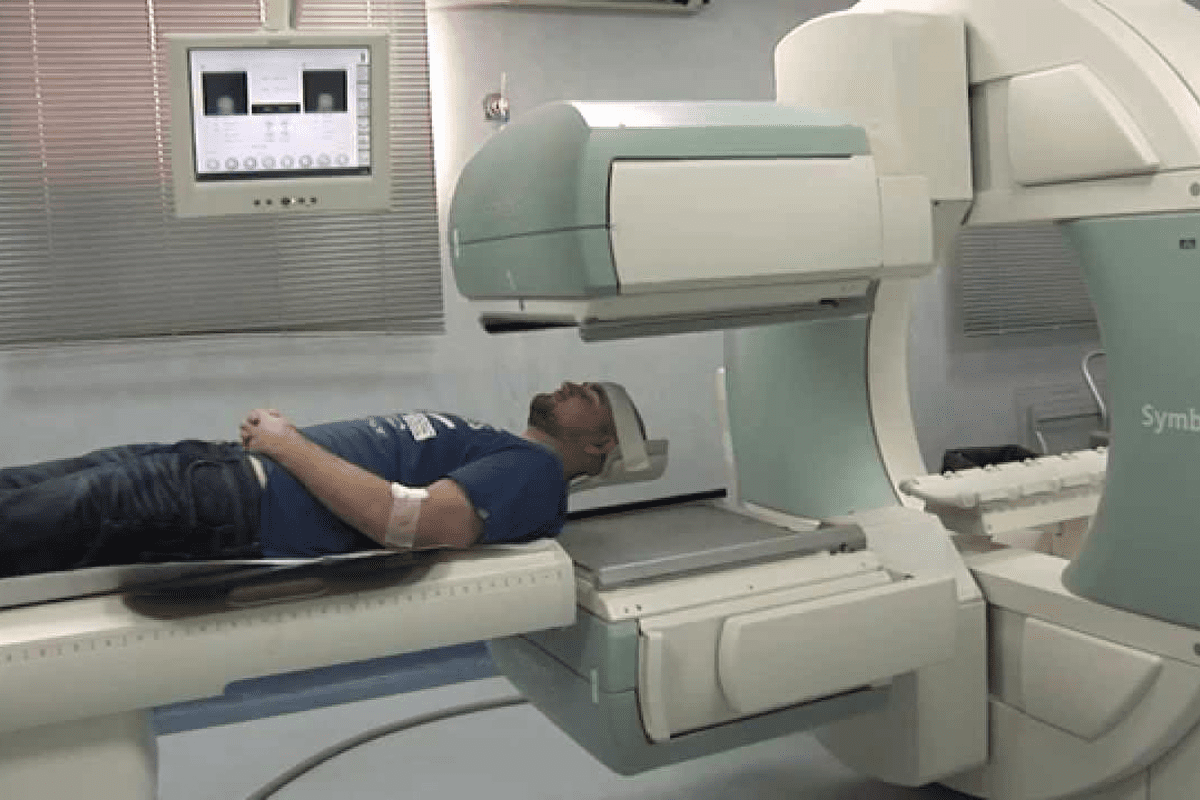
Bone Marrow Aspiration and Biopsy
Bone marrow aspiration and biopsy are key for diagnosing disorders. Bone marrow aspiration takes a sample of the liquid marrow. Bone marrow biopsy takes a piece of bone and marrow. These help check blood cell production and find problems.
Doctors say these tests are vital for diagnosing many disorders. They are done under local anesthesia. They give important insights into the condition.
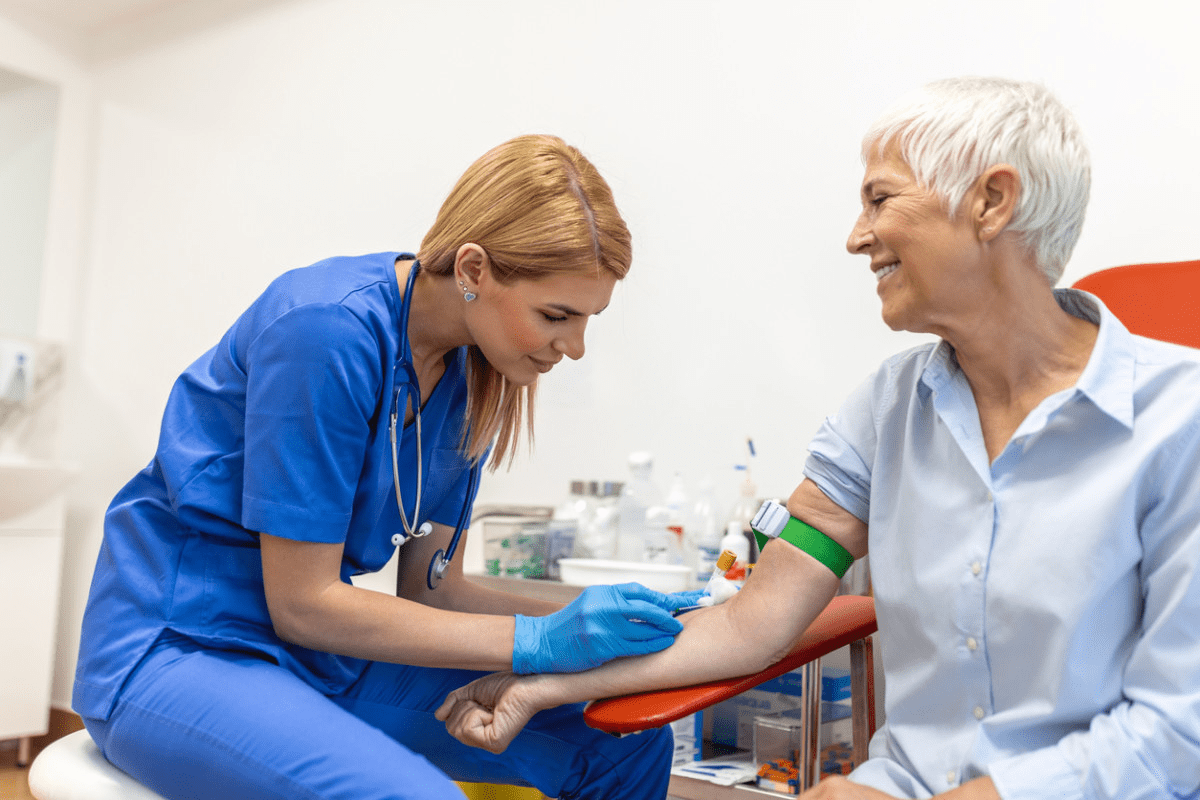
Blood Tests and Imaging Studies
Blood tests are also important for diagnosis. They check blood cell levels. Imaging like X-rays and MRI help see how far the disorder has spread.
- Blood tests check blood cell counts and find issues.
- Imaging studies show how much bone marrow is affected.
Conventional Treatments vs. Emerging Therapies
Treatment for bone marrow disorders depends on the condition. Conventional treatments include chemotherapy and supportive care. Emerging therapies like gene therapy are also being explored.
“The treatment for bone marrow disorders is changing. New therapies offer hope for better outcomes.” This shows the need for ongoing research and trials.
Bone Marrow Transplantation: When Is It Necessary?
Bone marrow transplantation is a cure for some disorders. It replaces bad marrow with healthy stem cells. This can be from the patient or a donor.
Deciding on bone marrow transplantation depends on several factors. These include the disorder type, its severity, the patient’s health, and donor availability. We’ll explore this treatment option further.
Conclusion: Advances in Understanding and Treating Bone Marrow Disorders
The field of bone marrow disorders has seen big strides, bringing hope to many. At Liv Hospital, we’re dedicated to top-notch healthcare and support for international patients. Our goal is to give each patient the best care for their condition. Ongoing bone marrow research and new tech are making diagnosis and treatment better.
We lead in using the newest treatments for bone marrow disorders. This includes new therapies and care plans tailored for each patient. Our focus on the latest research helps us offer effective treatments for complex cases. We aim to better the lives of those with these conditions.
Our commitment to full care is clear in our treatment plans, made for each patient’s needs. We see the future of treating bone marrow diseases in more research and teamwork. This drives us to explore new possibilities in patient care.
FAQ
What are bone marrow disorders?
Bone marrow disorders affect the bone marrow’s ability to make healthy blood cells. This can lead to issues like anemia, infections, and bleeding problems. It can also cause cancer.
What is the function of bone marrow?
Bone marrow is the spongy tissue in bones that makes blood cells. It turns stem cells into red blood cells, white blood cells, and platelets.
What are the different types of bone marrow?
There are two types of bone marrow. Red bone marrow makes blood cells, while yellow bone marrow has fat cells. Adults mostly have yellow bone marrow.
What are the common types of bone marrow diseases?
Common bone marrow diseases include aplastic anemia, myelodysplastic syndromes, and myeloproliferative neoplasms. Leukemia, lymphoma, and multiple myeloma are also common.
What is aplastic anemia?
Aplastic anemia is when the bone marrow can’t make blood cells. It can be caused by toxins, some medicines, and viruses.
How is leukemia classified?
Leukemia is divided into acute and chronic types. Each type is further classified based on the cell type involved.
What is the difference between Hodgkin and non-Hodgkin lymphoma?
Hodgkin and non-Hodgkin lymphoma are two types of lymphoma. They have different characteristics and treatment options.
What is multiple myeloma?
Multiple myeloma is a cancer where plasma cells in the bone marrow grow too much. It can cause anemia, bone damage, and kidney problems.
What are genetic bone marrow abnormalities?
Genetic bone marrow abnormalities are caused by mutations. They affect the bone marrow’s ability to make blood cells. Examples include Fanconi anemia and Diamond-Blackfan anemia.
How are bone marrow disorders diagnosed?
Doctors use tests like bone marrow aspiration and biopsy, blood counts, and imaging studies to diagnose bone marrow disorders.
What are the treatment options for bone marrow disorders?
Treatment depends on the condition. It can include chemotherapy, immunosuppressive therapy, gene therapy, and targeted treatments.
When is bone marrow transplantation necessary?
Bone marrow transplantation is a cure for some conditions. It replaces diseased bone marrow with healthy stem cells.
What are bone marrow disorders?
Bone marrow disorders affect the bone marrow’s ability to make healthy blood cells. This can lead to issues like anemia, infections, and bleeding problems. It can also cause cancer.
What is the function of bone marrow?
Bone marrow is the spongy tissue in bones that makes blood cells. It turns stem cells into red blood cells, white blood cells, and platelets.
What are the different types of bone marrow?
There are two types of bone marrow. Red bone marrow makes blood cells, while yellow bone marrow has fat cells. Adults mostly have yellow bone marrow.
What are the common types of bone marrow diseases?
Common bone marrow diseases include aplastic anemia, myelodysplastic syndromes, and myeloproliferative neoplasms. Leukemia, lymphoma, and multiple myeloma are also common.
What is aplastic anemia?
Aplastic anemia is when the bone marrow can’t make blood cells. It can be caused by toxins, some medicines, and viruses.
How is leukemia classified?
Leukemia is divided into acute and chronic types. Each type is further classified based on the cell type involved.
What is the difference between Hodgkin and non-Hodgkin lymphoma?
Hodgkin and non-Hodgkin lymphoma are two types of lymphoma. They have different characteristics and treatment options.
What is multiple myeloma?
Multiple myeloma is a cancer where plasma cells in the bone marrow grow too much. It can cause anemia, bone damage, and kidney problems.
What are genetic bone marrow abnormalities?
Genetic bone marrow abnormalities are caused by mutations. They affect the bone marrow’s ability to make blood cells. Examples include Fanconi anemia and Diamond-Blackfan anemia.
How are bone marrow disorders diagnosed?
Doctors use tests like bone marrow aspiration and biopsy, blood counts, and imaging studies to diagnose bone marrow disorders.
What are the treatment options for bone marrow disorders?
Treatment depends on the condition. It can include chemotherapy, immunosuppressive therapy, gene therapy, and targeted treatments.
When is bone marrow transplantation necessary?
Bone marrow transplantation is a cure for some conditions. It replaces diseased bone marrow with healthy stem cells.
References
National Marrow Donor Program (NMDP)/Be The Match. Diseases Treated by Transplant. https://www.nmdp.org/patients/understanding-transplant/diseases-treated-by-transplant
NYU Langone Health. Types of Myeloproliferative Disorders. https://nyulangone.org/conditions/myeloproliferative-disorders/types
News-Medical.Net. Bone Marrow Diseases. https://www.news-medical.net/health/Bone-Marrow-Diseases.aspx