Last Updated on October 28, 2025 by
CAR T stands for Chimeric Antigen Receptor T-cell. It’s a new way to fight cancer using your own immune cells. At Liv Hospital, we aim to provide top-notch healthcare and support for international patients.
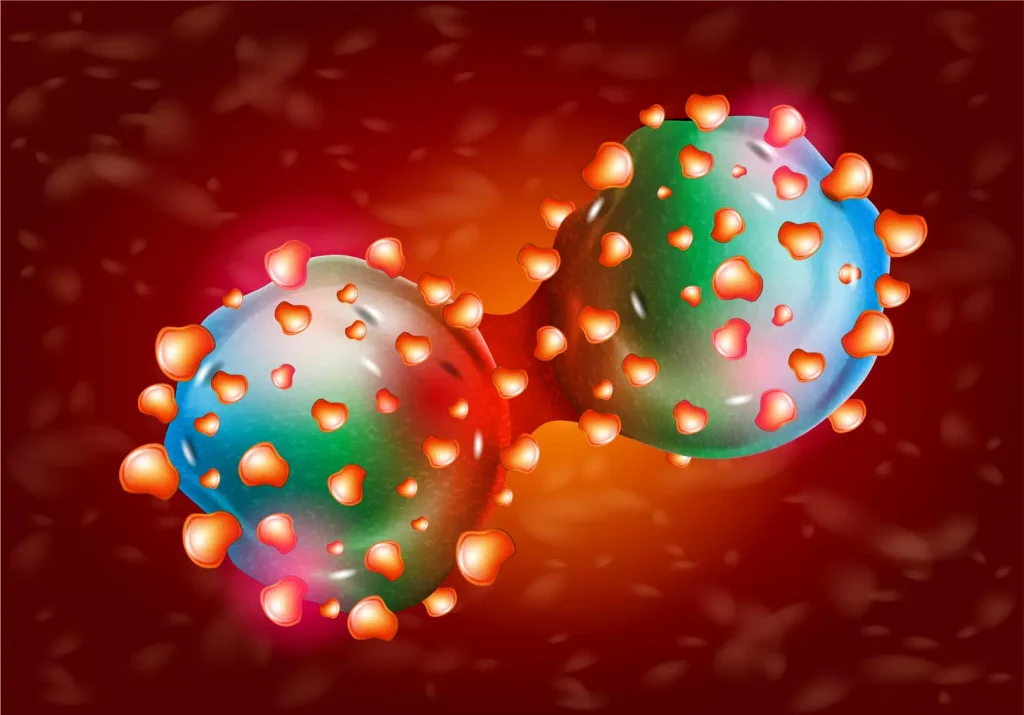
CAR T-cell therapy uses T cells to find and destroy cancer cells. This method has shown great hope in treating some blood cancers. By learning about CAR T-cell therapy, we see its big role in changing cancer treatment.
Key Takeaways
- CAR T stands for Chimeric Antigen Receptor T-cell, a type of engineered immune cell therapy.
- CAR T-cell therapy involves modifying T cells to recognize and attack cancer cells.
- This innovative treatment has shown promise in treating certain types of blood cancers.
- Liv Hospital is committed to delivering world-class healthcare with extensive international patient support.
- CAR T-cell therapy is a groundbreaking approach in cancer treatment.
The Revolutionary World of Cellular Immunotherapy

Cellular immunotherapy is changing how we treat cancer. It offers new ways to help patients and doctors. This approach is making a big difference in fighting cancer.
Cancer Treatment Evolution: From Conventional to Cellular
Old ways to fight cancer include surgery, chemo, and radiation. These methods can help but have big side effects. CAR T-cell therapy is a new way that targets cancer better.
This therapy uses the body’s immune system to fight cancer. It’s a more precise and possibly curative option for some cancers.
The Emergence of T Cell-Based Therapies
CAR T-cell immunotherapy is a new hope in cancer treatment. It takes T cells from the blood, changes them to find cancer, and puts them back in the body.
| Therapy Type | Description | Key Benefits |
|---|---|---|
| CAR T-cell Therapy | Genetically modified T cells to recognize cancer cells | Targeted treatment, possible long-term remission |
| Conventional Chemotherapy | Chemical treatment to kill fast-growing cells | Works for many, well-known methods |
| Cellular Immunotherapy | Uses the immune system to fight cancer | May have fewer side effects, more effective |
The table shows how CAR T-cell therapy is different from old treatments. It points out the good things about new immunotherapy.
As we learn more about cellular immunotherapy, we’re entering a new era in cancer treatment. These new therapies are making care more personal and effective. They bring hope to patients and their families all over the world.
What Does CAR T Stand For: Decoding the Terminology
CAR T-cell therapy is a new and exciting treatment. To get its full impact, we need to understand its terms. It uses a patient’s immune cells, made to fight cancer better. Let’s explore what CAR T really means.
Chimeric Antigen Receptor: The Synthetic Cancer-Fighting Tool
A Chimeric Antigen Receptor (CAR) is a man-made receptor. It’s made to find and stick to cancer cells’ proteins. It’s called “chimeric” because it’s made from different parts.
This receptor is very specific. It targets cancer cells but not healthy ones. This helps avoid the usual side effects of cancer treatments.
T Cells: The Immune System’s Warriors
T cells are a key part of our immune system. They can tell self from non-self cells. This makes them great at fighting infections and diseases, like cancer.
In CAR T-cell therapy, T cells are taken from the patient. They’re then changed to have the CAR and put back in the patient. These T cells can now find and kill cancer cells better.
The Full Meaning Behind the CAR T Acronym
The CAR T acronym means Chimeric Antigen Receptor T-cell. It’s a therapy that makes T cells better at finding and killing cancer cells.
To wrap up, let’s look at what CAR T-cell therapy is all about:
| Component | Description |
|---|---|
| C | Chimeric |
| A | Antigen |
| R | Receptor |
| T | T-cell |
Understanding CAR T helps us see how it’s changing cancer treatment. It’s a big step forward in fighting cancer.
The History and Evolution of CAR T-Cell Therapy
CAR T-cell therapy is a game-changer in cancer treatment. It has roots in decades of research and innovation. This therapy offers new hope to patients with tough-to-treat cancers.
Pioneering Research and Early Developments
The idea of CAR T-cell therapy started in the late 20th century. Scientists first explored T-cell biology and their role in fighting diseases. They found that T-cells could be made to target cancer cells better.
Significant progress was made in CAR T-cell therapy. At first, it was hard to modify T-cells to fight cancer. But, new genetic engineering tools helped create chimeric antigen receptors (CARs).
Breakthrough Discoveries Leading to Clinical Applications
The big leap was creating CARs that let T-cells find and attack cancer cells. This led to the first CAR T-cell therapy trials in the early 2000s.
One major success was treating blood cancers like acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). These wins showed CAR T-cell therapy’s promise as a treatment.
FDA Approvals and Commercial CAR T Products
The FDA approved the first CAR T-cell therapy in 2017. This was a big step forward. Now, several CAR T products are available, like tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta).
These approvals have made CAR T-cell therapy more available to patients. Below is a table with details on FDA-approved CAR T products.
| CAR T Product | Approved Indication | FDA Approval Year |
|---|---|---|
| Tisagenlecleucel (Kymriah) | Relapsed or refractory B-cell precursor ALL, DLBCL | 2017 |
| Axicabtagene ciloleucel (Yescarta) | Relapsed or refractory DLBCL, follicular lymphoma | 2017 |
| Brexucabtagene autoleucel (Tecartus) | Relapsed or refractory mantle cell lymphoma | 2020 |
| Lisocabtagene maraleucel (Breyanzi) | Relapsed or refractory DLBCL, follicular lymphoma | 2021 |
The journey of CAR T-cell therapy shows the power of teamwork and innovation. As research keeps going, we’ll see more uses of CAR T-cell therapy for different cancers.
The Science Behind How CAR T-Cell Therapy Works
CAR T-cell therapy uses the immune system to fight cancer. It starts by taking T cells from a patient’s blood. This is the first step in a complex process.
The CAR T-Cell Manufacturing Process
The making of CAR T cells is detailed and involves several steps. First, T cells are taken from the patient’s blood or bone marrow. These T cells then go to a lab where they are changed to find and attack cancer cells.
- T cells are isolated and purified.
- The isolated T cells are genetically engineered to express the CAR.
- The modified T cells are expanded in number.
- The final CAR T-cell product is formulated and prepared for infusion.
The Mechanism of Action
CAR T-cell therapy works by making T cells find and kill cancer cells. The CAR on the T cells binds to a specific antigen on the surface of cancer cells, starting a chain of events. This leads to the T cells getting ready to fight.
- The CAR T cells recognize cancer cells through the CAR.
- Upon recognition, the CAR T cells become activated.
- Activated CAR T cells proliferate and expand.
- The expanded CAR T cells then target and kill the cancer cells.
Understanding CAR T-cell therapy is key to seeing its value in cancer treatment. It changes a patient’s T cells to attack cancer. This is a big step forward in fighting cancer.
Structure and Design of Chimeric Antigen Receptors
CAR T-cell therapy’s success relies on the design of chimeric antigen receptors. These receptors are made to find specific cancer cell markers. We’ll look into CAR design, from its parts to the different types and their targets.
Anatomy of a CAR: From Extracellular to Intracellular Domains
A chimeric antigen receptor is a mix of parts from different sources. It lets T cells spot cancer cells. It has an extracellular domain that grabs onto the target antigen, a transmembrane domain that keeps it in the T-cell membrane, and an intracellular domain that sends signals inside the T cell when it finds the antigen.
The part outside the cell, the extracellular domain, uses a single-chain variable fragment (scFv) from antibodies. This lets CAR T cells find and attack cancer cells with the right antigen.
Generations of CAR Design: First Through Fourth
CAR design has grown from the first to the fourth generation. Each generation has new features to make CAR T cells work better and safer. The first-generation CARs had just one signaling part, CD3ζ, which helped T cells but didn’t make them last long.
Second-generation CARs added another part, like CD28 or 4-1BB, to help T cells grow and live longer. Third-generation CARs have two of these parts, making T cells even better. Fourth-generation CARs, or TRUCKs, can release substances that help fight cancer more.
Target Antigens in CAR T-Cell Therapy
Picking the right target antigen is key for CAR T-cell therapy to work. The antigen should only be on cancer cells to avoid harming healthy cells. Common targets are CD19 for B-cell cancers and BCMA for multiple myeloma.
A study on NCBI shows that the antigen’s specificity is important. It helps reduce harm to healthy cells.
| Target Antigen | Cancer Type | CAR Design Features |
|---|---|---|
| CD19 | B-cell lymphomas and leukemias | Second-generation CARs with CD28 or 4-1BB co-stimulatory domains |
| BCMA | Multiple myeloma | Third-generation CARs with multiple co-stimulatory domains |
Current Applications and Approved Indications
CAR T-cell therapy is a new way to fight cancer. It mainly helps with B-cell cancers. This treatment offers hope to those who have tried other options.
Treating B-Cell Malignancies
CAR T-cell therapy is approved for some B-cell cancers. It works by changing a patient’s T cells to attack cancer. Then, these changed cells are put back into the patient.
Many clinical trials have shown it works well. For example, studies show it can cure many patients with certain B-cell cancers.
Ongoing Clinical Trials for Other Cancer Types
Researchers are also looking at CAR T-cell therapy for other cancers. They are testing it in solid tumors and other blood cancers.
- Multiple myeloma
- Solid tumors such as glioblastoma and ovarian cancer
- Other types of leukemia and lymphoma
These trials aim to use CAR T-cell therapy for more cancers. This could help more patients find new treatments.
CAR T-Cell Therapy vs. Traditional Cancer Treatments
CAR T-cell therapy is different from usual cancer treatments. It uses the body’s immune system to fight cancer. This is unlike chemotherapy and radiation.
“CAR T-cell therapy has the chance to give long-lasting results for some cancers. This is a big plus compared to some other treatments.”
One big plus of CAR T-cell therapy is it targets cancer cells well. This can help avoid harming healthy cells. But, it also has its own challenges and side effects, like CRS and neurotoxicity.
As research goes on, CAR T-cell therapy will likely get better. This could lead to more uses and better results for patients.
The Patient Journey: From Eligibility to Treatment
The path to CAR T-cell therapy has many important steps. First, patients find out if they can get the treatment. Knowing what to expect makes the journey easier.
Determining Patient Eligibility for CAR T-Cell Therapy
To see if a patient can get CAR T-cell therapy, doctors do a detailed check. They look at the patient’s health, cancer type and stage, and past treatments.
Key factors in determining eligibility include:
- Diagnosis of specific B-cell malignancies
- Previous treatment history, including failure of other therapies
- Patient’s overall health and performance status
- Adequate organ function
Preparing for Treatment: What Patients Should Expect
After being found eligible, patients start getting ready for treatment. This includes several steps.
Apheresis, where T-cells are taken from the blood, is a key first step. Patients also have to go through tests to check their health and get ready for the therapy.
| Preparation Step | Description | Timeline |
|---|---|---|
| Apheresis | Collection of T-cells from the patient’s blood | 1-2 days |
| Health Assessments | Various tests to evaluate overall health | Variable, typically 1-4 weeks |
| Chemotherapy | Lymphodepleting chemotherapy to prepare the body | 3-5 days before CAR T infusion |
The Treatment Timeline and Process
The time it takes for CAR T-cell therapy can differ. But, it usually goes through a few main stages:
- Chemotherapy to deplete lymphocytes
- Infusion of CAR T-cells
- Monitoring for response and possible side effects
The CAR T-cell infusion itself is quick, usually under an hour. But, patients are watched closely for any quick reactions.
Challenges, Side Effects, and Management Strategies
CAR T-cell therapy is growing, but we must understand its side effects and how to manage them. This treatment has shown great promise against some cancers. Yet, we must face and solve the challenges it brings.
Cytokine Release Syndrome: A Common Complication
Cytokine release syndrome (CRS) is a major side effect of CAR T-cell therapy. It happens when the T cells release a lot of cytokines into the blood. This can cause symptoms from mild to severe.
CRS symptoms include fever, nausea, headache, and fatigue. In severe cases, it can lead to low blood pressure and organ problems. Because CRS can be different for everyone, it’s important to watch patients closely and act fast if needed.
Neurotoxicity and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS)
Neurotoxicity, like ICANS, is another big side effect. ICANS can cause confusion, disorientation, and in serious cases, seizures or brain swelling. Scientists are studying why ICANS happens, but think it’s linked to cytokine release and how it affects the brain.
Other Possible Side Effects
Patients getting CAR T-cell therapy might also face other side effects. These include:
- B cell aplasia leading to low immune function
- Infections because of weakened immune system
- Hemophagocytic lymphohistiocytosis (HLH)
- Tumor lysis syndrome
Each side effect needs careful management and monitoring.
Management and Mitigation of Adverse Events
Managing CAR T-cell therapy side effects needs a team effort. Strategies include:
| Side Effect | Management Strategy |
|---|---|
| Cytokine Release Syndrome (CRS) | Use of tocilizumab, an anti-IL-6 receptor antibody; corticosteroids in severe cases |
| Neurotoxicity/ICANS | Corticosteroids; supportive care; in some cases, tocilizumab |
| B Cell Aplasia/Hypogammaglobulinemia | IVIG replacement therapy |
Spotting and treating these side effects early is key to better patient outcomes.
The Future Landscape of CAR T-Cell Therapy
CAR T-cell therapy is on the verge of a new era. This is thanks to new designs and wider uses. Researchers are making big strides in this field.
Next-Generation CAR T-Cell Designs
New CAR T-cell designs are exciting. They aim to be more effective and safe. For example, fourth-generation CAR T cells, or TRUCKs, release cytokines to fight cancer better.
There are also CAR T cells with multiple specificity. They can target several cancer cell antigens at once. This could help prevent cancer cells from evading treatment.
Expanding Applications to Solid Tumors
While CAR T-cell therapy works well for some blood cancers, it’s harder for solid tumors. But, researchers are finding ways to tackle this. They’re working on targeting specific tumor antigens and improving CAR T-cell survival in solid tumors.
We’re hopeful that these efforts will bring CAR T-cell therapy to more cancers, including solid tumors.
Off-the-Shelf (Allogeneic) CAR T-Cell Products
Off-the-shelf CAR T-cell products are a big step forward. These cells come from healthy donors, not patients. This could mean faster treatment and helping more people.
Many companies are working on these products. Several are in clinical trials now.
Combination Approaches with Other Immunotherapies
Researchers are also exploring combining CAR T-cell therapy with other treatments. For instance, using CAR T cells with checkpoint inhibitors might make treatments more effective. This is because it can fight the immune system’s suppressive effects in tumors.
We think these combinations will be key in future cancer treatments. They offer new hope for patients who haven’t responded to current therapies.
Conclusion: The Transformative Impact of CAR T-Cell Therapy
CAR T-cell therapy has changed the game for some blood cancers. It brings new hope to patients and changes how we fight cancer. The car t-cell therapy impact is huge, giving a chance for a cure to those who’ve tried everything else.
This therapy works by making T cells attack cancer cells. The transformative impact comes from its ability to offer treatments that really work. These treatments are made just for each patient, leading to big improvements.
In short, CAR T-cell therapy is a big step forward in cancer treatment. As research grows and new uses are found, we’ll see even better results for patients. The car t-cell therapy conclusion will likely be more innovation and better health outcomes.
FAQ
What does CAR T stand for?
CAR T stands for Chimeric Antigen Receptor T-cell. It’s a type of treatment for blood cancers.
What is CAR T-cell therapy?
CAR T-cell therapy is a new way to fight cancer. It takes T cells from your blood, changes them, and puts them back in your body. This helps them attack cancer cells.
How does CAR T-cell therapy work?
It uses your own T cells, which are changed to find and kill cancer cells. This is done by adding a special receptor to the T cells.
What is the mechanism of action of CAR T-cell therapy?
The T cells with the special receptor find and stick to cancer cells. This makes the T cells grow and kill the cancer cells.
What are the side effects of CAR T-cell therapy?
Side effects include cytokine release syndrome (CRS), neurotoxicity, and immune effector cell-associated neurotoxicity syndrome (ICANS). Other side effects are B-cell aplasia and infections.
How is cytokine release syndrome (CRS) managed?
CRS is treated with hydration, oxygen, and sometimes tocilizumab and corticosteroids. This is for severe cases.
What is the future of CAR T-cell therapy?
The future includes new CAR T-cell designs and using it for solid tumors. There’s also work on off-the-shelf products and combining it with other treatments.
Are there any ongoing clinical trials for CAR T-cell therapy?
Yes, there are trials for CAR T-cell therapy in different cancers. This includes B-cell malignancies and solid tumors.
How is patient eligibility determined for CAR T-cell therapy?
Eligibility depends on the cancer type and stage, previous treatments, and overall health.
What is the treatment timeline and process for CAR T-cell therapy?
The process includes steps like apheresis, making CAR T cells, and infusing them. After, there’s monitoring and care.