Last Updated on October 20, 2025 by mcelik

Myelodysplastic syndrome is a complex condition. It affects the bone marrow’s ability to produce healthy blood cells.
At Liv Hospital, we know how important accurate information and compassionate care are. This is for patients facing this challenging blood disorder.
We will explore seven key facts about myelodysplastic syndrome. We will look at its impact on life expectancy. This will help patients and families understand this difficult diagnosis better.
Key Takeaways
- Understanding myelodysplastic syndrome is key for patients and healthcare providers.
- Myelodysplastic syndrome affects the bone marrow’s ability to produce healthy blood cells.
- Life expectancy varies based on several factors, including the specific type of myelodysplastic syndrome.
- Accurate diagnosis and treatment are essential for managing the condition.
- Compassionate care and support are vital for patients and families affected by myelodysplastic syndrome.
What is Myelodysplastic Syndrome?

Myelodysplastic syndrome (MDS) is a complex condition that affects the bone marrow’s ability to produce healthy blood cells. It is characterized by the bone marrow’s failure to produce enough healthy blood cells. This leads to various health complications.
Definition and Basic Characteristics
MDS is a group of disorders caused by poorly formed or dysfunctional blood cells. It often leads to bone marrow failure. The basic characteristics include:
- Dysplasia in one or more cell lines (erythrocytes, leukocytes, or platelets)
- Ineffective hematopoiesis resulting in cytopenias
- Risk of progression to acute myeloid leukemia (AML)
Myelodysplastic syndrome is often associated with genetic mutations. These mutations affect the bone marrow’s ability to produce healthy cells. According to recent studies, understanding these genetic underpinnings is key to developing effective treatments.
Prevalence and Risk Factors
MDS is considered a rare disease. It has an estimated annual incidence of about 4-5 cases per 100,000 people in the United States. The prevalence increases with age, with most cases diagnosed in individuals over 70 years old.
| Age Group | Incidence Rate (per 100,000) |
|---|---|
| <50 years | 0.5-1.0 |
| 50-69 years | 2-4 |
| 70+ years | 15-20 |
Risk factors for developing MDS include exposure to certain chemicals, radiation, and previous chemotherapy. Genetic predisposition also plays a significant role in the development of MDS.
We recognize that understanding MDS requires a thorough approach. This includes its definition, prevalence, and associated risk factors. By acknowledging these aspects, we can better appreciate the complexities of this condition. We also see the need for personalized treatment plans.
The MDS Condition: Pathophysiology and Bone Marrow Failure

Understanding Myelodysplastic Syndrome (MDS) is key to knowing how it affects the body. MDS makes it hard for the bone marrow to create healthy blood cells. This leads to many problems.
Normal Blood Cell Production vs. MDS
In a healthy person, the bone marrow makes blood cells in a controlled way. It turns stem cells into red, white blood cells, and platelets. But MDS messes with this, making dysplastic cells that don’t work well and don’t last long.
The main differences are:
- MDS has abnormal cells not seen in healthy people.
- There’s a big drop in healthy blood cells, causing cytopenias.
- The bone marrow can’t fully mature blood cells, leading to ineffective hematopoiesis.
Types of Blood Cells Affected
MDS can harm different blood cells, causing various symptoms. It often leads to:
- Anemia from not enough red blood cells, causing tiredness and weakness.
- Infections because of a lack of white blood cells, which fight off germs.
- Bleeding complications from low platelet counts, making it hard for blood to clot.
For more on symptoms of hematologic diseases like MDS, check this resource.
Knowing which blood cells MDS affects is vital for managing it. Healthcare providers can then create better treatment plans to help patients.
Key Fact 1: Common Symptoms and Clinical Presentation
MDS often shows symptoms related to bone marrow failure. Patients may feel tired, weak, and short of breath. These symptoms come from the disorder’s effect on blood cell production.
Primary Symptoms of Anemia, Infection, and Bleeding
Anemia is a main symptom of MDS. It leads to fatigue, weakness, and shortness of breath. This happens because there are not enough red blood cells to carry oxygen.
People with MDS also face a higher infection risk. This is because they have fewer white blood cells. White blood cells help fight off infections. Symptoms of infection include fever, chills, and a persistent cough.
Bleeding problems are another symptom of MDS. This is because of a low platelet count. Symptoms include easy bruising, nosebleeds, and bleeding gums.
When to Seek Medical Attention
If you’re experiencing symptoms of MDS, you should see a doctor right away. Look out for persistent fatigue, frequent infections, or unexplained bleeding. These are signs you need to see a healthcare professional.
Getting a diagnosis and treatment early can make a big difference. It can improve your quality of life. Always watch your health and don’t hesitate to see your doctor if you notice any concerning symptoms.
Key Fact 2: Diagnostic Approaches for MDS
Diagnosing MDS requires detailed blood tests to spot abnormal cell production. It’s a complex task that includes clinical checks, lab tests, and sometimes bone marrow exams.
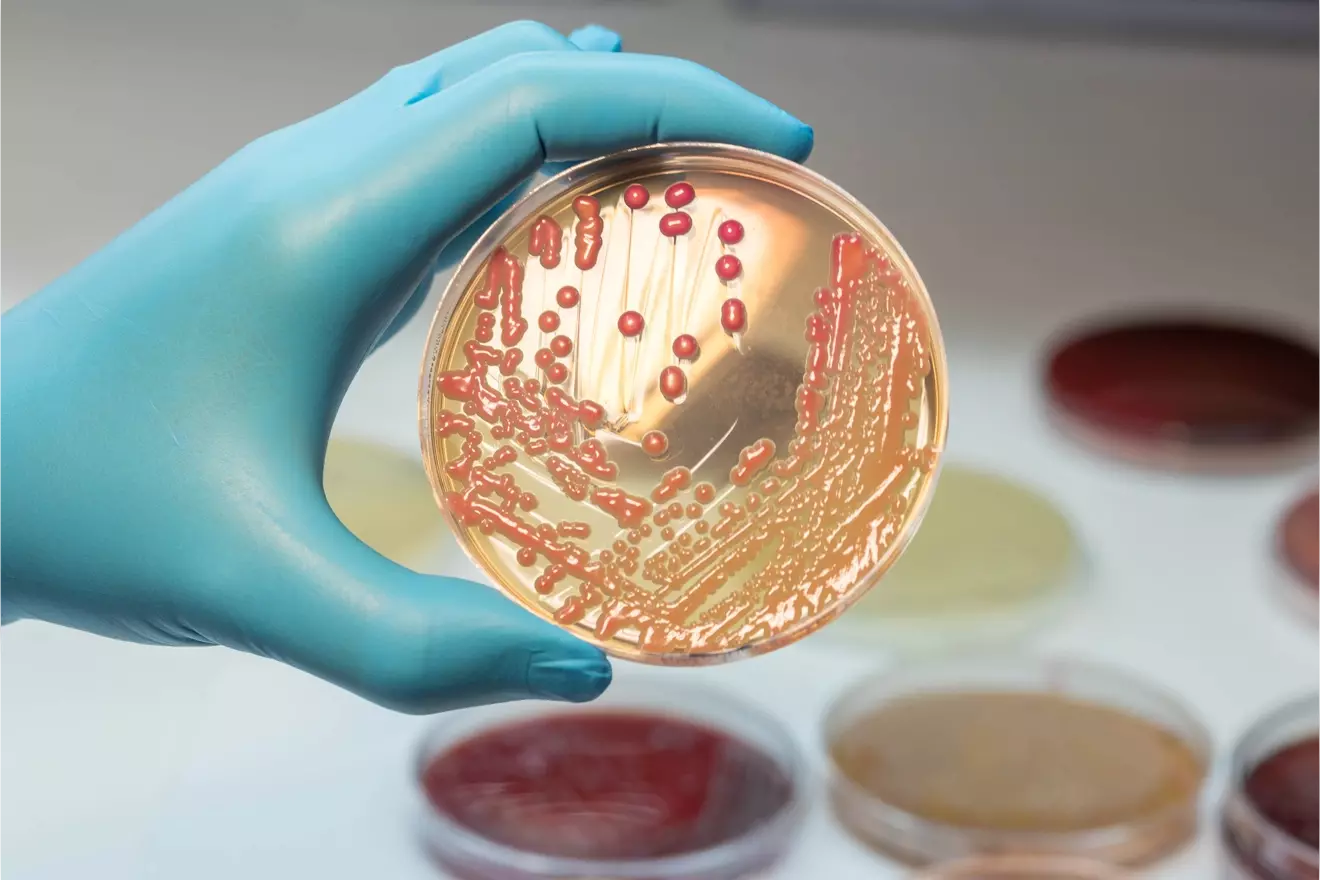
Blood Tests and MDS Cell Identification
Blood tests are key in spotting MDS. They help find abnormal blood cells, a key sign of the disease. Complete Blood Count (CBC) is often the first test, showing if blood cell counts are off.
Looking at blood cell shapes is part of identifying MDS cells. This search for blast cells shows if the blood is not normal. Blast cells are young cells that shouldn’t be in the blood in large numbers.
Myelodysplastic Syndrome Blood Film Characteristics
A blood film analysis is also vital for MDS diagnosis. It looks at blood under a microscope for cell shape and size issues. Signs of MDS include hypogranular neutrophils and pseudo-Pelger-Huët anomaly.
The blood film shows how blood cells are changing, which is key for MDS. Doctors use this info to understand the disease’s severity and type. This helps in planning the right treatment.
Key Fact 3: Classification and Risk Stratification Systems
Understanding the classification and risk stratification systems for Myelodysplastic Syndrome (MDS) is key. It helps determine prognosis and guide treatment. These systems categorize patients based on their condition’s severity, leading to personalized treatment plans.
WHO Classification of Myelodysplastic Syndromes
The World Health Organization (WHO) classification system for MDS is widely used. It categorizes the disease based on morphological and genetic features. This system distinguishes MDS from other myeloid neoplasms and identifies specific subtypes with different prognostic implications.
Key features of the WHO classification include:
- Percentage of blasts in the bone marrow and peripheral blood
- Presence of specific cytogenetic abnormalities
- Degree of dysplasia in different myeloid lineages
- says, “The
“Accurate diagnosis and classification are critical in MDS, as they directly impact treatment choices and patient outcomes.
IPSS and IPSS-R Risk Categories
The International Prognostic Scoring System (IPSS) and its revised version (IPSS-R) are used to stratify MDS patients. They predict the risk of progression to acute myeloid leukemia (AML) and overall survival. These systems consider cytogenetic abnormalities, blast percentage, and number of cytopenias.
| Risk Category | IPSS Score | IPSS-R Score | Prognosis |
|---|---|---|---|
| Low | 0 | ≤ 3 | Favorable |
| Intermediate | 0.5-1 | 3-4.5 | Moderate |
| High | ≥ 1.5 | ≥ 4.5 | Poor |
The IPSS-R system offers a more detailed stratification. It includes additional variables like depth of cytopenias and more detailed cytogenetic information. This allows for a more precise estimation of prognosis and tailoring treatment strategies to individual patient needs.
By using these systems, we can better understand MDS’s heterogeneity. This helps us make informed decisions about patient care.
Key Fact 4: MDS Progression to Acute Myeloid Leukemia
It’s important to understand how Myelodysplastic Syndrome (MDS) can turn into Acute Myeloid Leukemia (AML). This change is complex and depends on several factors. These include the type of MDS, genetic changes, and the patient’s health.
Understanding the 40% Progression Risk
Research shows that up to 40% of MDS cases can turn into AML. This change affects how the disease is treated and the patient’s outlook. The risk of this change varies with different MDS subtypes. Some types are more likely to turn into AML.
Warning Signs and Monitoring Protocols
It’s key to spot the signs of MDS turning into AML early. Signs include a quick rise in blast cells, worsening blood counts, and new genetic changes. Regular blood tests and bone marrow checks help catch these signs early.
Good monitoring involves clinical checks, lab tests, and genetic studies. By watching patients closely, we can find those at high risk of AML. This helps us tailor care to meet their needs, improving their life quality.
Key Fact 5: Myelodysplasia Life Expectancy by Risk Category
Knowing how long you might live with myelodysplastic syndrome (MDS) is key. It helps both patients and doctors make better choices about treatment. The life span of MDS patients changes a lot based on their risk level.
Life expectancy for MDS patients can be quite different. It can range from 8-10 years for those at very low risk to just 9-15 months for those at very high risk. Doctors use the International Prognostic Scoring System (IPSS) and its updated version (IPSS-R) to sort patients. They look at things like bone marrow blast percentage, genetics, and how many blood cell counts are low.
Knowing your MDS prognosis and life expectancy helps you make choices about treatment. Every person’s experience with MDS is different. Your life expectancy can be affected by how well you respond to treatment and your overall health.
FAQ
What is Myelodysplastic Syndrome (MDS)?
Myelodysplastic syndrome (MDS) is a complex condition. It affects the bone marrow’s ability to produce healthy blood cells. This leads to various complications.
What are the common symptoms of MDS?
Patients with MDS often have symptoms like fatigue, infections, and bleeding episodes. These are due to a lack of healthy blood cells.
How is MDS diagnosed?
Diagnosing MDS involves several steps. Blood tests, bone marrow examination, and cytogenetic analysis are used.
What is the significance of the WHO classification and IPSS/IPSS-R risk categories in MDS?
The WHO classification and IPSS/IPSS-R risk categories are key. They help determine prognosis and guide treatment decisions.
What is the risk of MDS progressing to Acute Myeloid Leukemia (AML)?
The risk of MDS progressing to AML is a major concern. Understanding the risk factors is essential for management.
How does life expectancy vary among MDS patients?
Life expectancy in MDS patients varies. It depends on their risk category and prognostic factors.
What is myelodysplasia life expectancy?
Myelodysplasia life expectancy depends on the risk category. Lower-risk patients generally have a better prognosis than higher-risk patients.
What are the characteristics of MDS on blood film analysis?
Blood film analysis in MDS shows various abnormalities in blood cells. These help diagnose the condition.
What are the primary symptoms related to anemia, infection, and bleeding in MDS?
The main symptoms of MDS include fatigue, recurrent infections, and bleeding episodes. These are due to a lack of healthy blood cells.
What is Myelodysplastic Syndrome (MDS)?
Myelodysplastic syndrome (MDS) is a complex condition. It affects the bone marrow’s ability to produce healthy blood cells. This leads to various complications.
What are the common symptoms of MDS?
Patients with MDS often have symptoms like fatigue, infections, and bleeding episodes. These are due to a lack of healthy blood cells.
How is MDS diagnosed?
Diagnosing MDS involves several steps. Blood tests, bone marrow examination, and cytogenetic analysis are used.
What is the significance of the WHO classification and IPSS/IPSS-R risk categories in MDS?
The WHO classification and IPSS/IPSS-R risk categories are key. They help determine prognosis and guide treatment decisions.
What is the risk of MDS progressing to Acute Myeloid Leukemia (AML)?
The risk of MDS progressing to AML is a major concern. Understanding the risk factors is essential for management.
How does life expectancy vary among MDS patients?
Life expectancy in MDS patients varies. It depends on their risk category and prognostic factors.
What is myelodysplasia life expectancy?
Myelodysplasia life expectancy depends on the risk category. Lower-risk patients generally have a better prognosis than higher-risk patients.
What are the characteristics of MDS on blood film analysis?
Blood film analysis in MDS shows various abnormalities in blood cells. These help diagnose the condition.
What are the primary symptoms related to anemia, infection, and bleeding in MDS?
The main symptoms of MDS include fatigue, recurrent infections, and bleeding episodes. These are due to a lack of healthy blood cells.
References
- Eureka Health. What is the life expectancy with myelodysplastic syndrome? [Internet]. 2025 Jun 13 [cited 2025 ___]. Available from: https://www.eurekahealth.com/resources/life-expectancy-with-myelodysplastic-syndrome-en (Eureka Health)
- HealthTree. How long will I live with myelodysplastic syndrome? [Internet]. [cited 2025 ___]. Available from: https://healthtree.org/mds/community/how-long-will-i-live-with-myelodysplastic-syndrome (healthtree.org)
- Wikipedia. Myelodysplastic syndrome. [Internet]. [cited 2025 ___]. Available from: https://en.wikipedia.org/wiki/Myelodysplastic_syndrome (Wikipedia)
- Healthline. MDS prognosis: life expectancy and outlook. [Internet]. [cited 2025 ___]. Available from: https://www.healthline.com/health/mds-prognosis (Healthline)
- Medical News Today. What is the outlook and life expectancy of MDS? [Internet]. [cited 2025 ___]. Available from: https://www.medicalnewstoday.com/articles/319346 (Medical News Today)