Last Updated on October 28, 2025 by
At Liv Hospital, we know that acute myeloid leukemia (AML) recurrence and relapse are big challenges. They affect how long patients live and their quality of life.
About 60-70% of adults get better after their first treatment. But, staying in remission is harder, more so for older adults. Doctors decide on a special treatment called allogeneic hematopoietic cell transplantation (allo-HCT) based on risks and benefits. They look at the chance of leukemia relapse and the risk of death from the treatment.
We know AML is a tough disease to handle. Recurrence worries both patients and doctors a lot. Many things can cause AML to come back, like genes, molecules, and how the disease acts.
Key Takeaways
- AML recurrence affects survival rates and quality of life.
- 60-70% of adults achieve remission after initial chemotherapy.
- Sustained remission is less common, more so in older adults.
- The risk/benefit ratio guides the decision for allo-HCT in AML patients.
- Genetic, molecular, and clinical factors influence AML recurrence.
Understanding Acute Myeloid Leukemia and Remission
It’s important for patients and doctors to understand Acute Myeloid Leukemia (AML) and what remission means. AML is a serious disease where bad cells grow fast in the bone marrow. This stops the bone marrow from making healthy blood cells.
What Defines AML Remission
Remission in AML means no leukemia cells are found in the bone marrow or blood. Getting to this point is a big win in AML treatment. Studies show that reaching complete remission can help AML patients live longer BMC Cancer.
Complete remission means the bone marrow looks normal and blood counts are almost back to normal. This is the best outcome for AML treatment.
Types of Remission in AML
There are different kinds of remission in AML, each with its own details. Complete Remission (CR) is the top goal, where no leukemia cells are found in the bone marrow or blood, and blood counts are normal.
Partial Remission (PR) shows a big drop in leukemia cells but not all are gone. While PR is good, it’s not as good as CR.
- Complete Remission with Incomplete Blood Count Recovery (CRi): This is a type of CR where blood counts don’t fully get back to normal.
- Morphologic Remission: This means no leukemia cells are seen in the bone marrow.
- Molecular Remission: This shows no leukemia markers are found.
Knowing about these remission types is key to managing AML well. It helps in making the right treatment choices and follow-up plans.
Remission Statistics in Acute Myeloid Leukemia
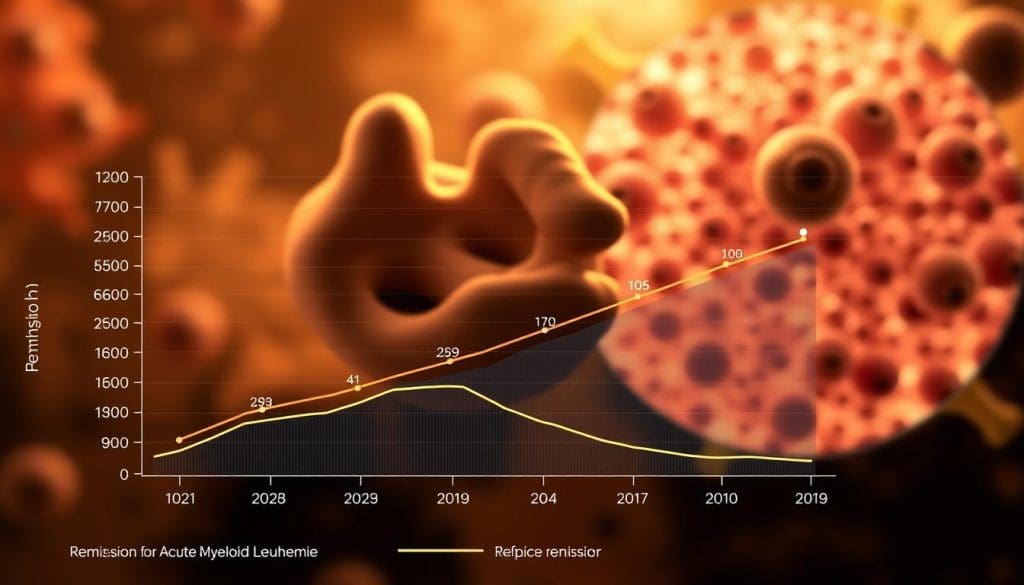
Acute Myeloid Leukemia remission rates are key to understanding the disease’s treatment success. These numbers help patients and doctors choose the best treatment plans.
Initial Remission Rates After Treatment
About 60-70% of adults get better after first chemotherapy for Acute Myeloid Leukemia. This shows how well modern treatments work to start remission. But, keeping that remission is just as important.
Getting to remission is a big win, but how long it lasts varies. Health, genetics, and leukemia type all affect it.
Age-Related Differences in Remission Achievement
Age affects how well remission lasts. Older adults often have a harder time keeping remission than younger ones. This is because of health issues, different leukemia types, and how well they handle strong chemotherapy.
Older patients might not handle aggressive chemotherapy well. So, their treatment for AML relapse must be adjusted to fit their health.
Knowing these age differences helps create better treatment plans. This improves outcomes for people of all ages.
Typical Duration of AML Remission
The time it takes for AML remission varies based on treatment success and genetic changes. Knowing these factors helps in finding ways to stop AML from coming back and manage symptoms.
Short-Term vs. Long-Term Remission Patterns
AML remission can be short-term or long-term. Short-term lasts less than a year, while long-term can last more than three years. Studies show that how long remission lasts varies among patients.
A study in BMC Cancer found that minimal residual disease (MRD) status is key in determining remission length.
Factors Affecting Remission Duration
Several things can affect how long AML remission lasts, including:
- Genetic Mutations: Some genetic changes can influence remission length. For example, mutations in FLT3 or NPM1 genes can affect prognosis.
- Response to Initial Therapy: How well the first treatment works is a big factor. Patients who get complete remission after the first treatment usually do better.
- Minimal Residual Disease (MRD) Status: MRD status is very important in predicting relapse risk. Patients with no detectable MRD usually have longer remissions.
Understanding these factors is key to preventing AML recurrence and managing recurring AML symptoms. By identifying high-risk patients, doctors can improve care and monitoring, leading to better outcomes.
Why Acute Myeloid Leukemia Recurrence Happens
Acute Myeloid Leukemia (AML) can come back due to many reasons. Knowing these reasons is key to stopping or managing it.
Biological Mechanisms Behind Relapse
AML often comes back because some cancer cells survive treatment. These cells can hide for a long time before starting to grow again.
Genetic changes, epigenetic changes, and the bone marrow’s effect on cancer cells also play a part in AML relapse.
Residual Disease and Leukemic Stem Cells
Leukemic stem cells (LSCs) are a big problem in AML relapse. These cells can keep the cancer alive by growing more.
LSCs are hard to kill because they can keep the cancer going, even after treatment.
| Characteristics | Leukemic Stem Cells (LSCs) | Non-LSCs |
|---|---|---|
| Self-Renewal Capability | Present | Absent |
| Therapy Resistance | High | Variable |
| Role in Relapse | Critical | Less Significant |
Treatment Resistance Development
AML can also come back because the cancer cells become resistant to treatment. This resistance can happen through genetic changes or other ways.
It’s important to understand how cancer cells become resistant. This helps us find new ways to treat AML and improve patient care.
By studying why AML comes back, we can learn how to help patients better. This includes looking at the role of cancer cells and how treatment resistance happens.
Risk Factors for AML Relapse
It’s key to know what makes AML relapse happen. AML coming back is a big problem in treating acute myeloid leukemia. Knowing what causes it helps us fight the disease better.
Genetic and Cytogenetic Risk Factors
Genetic and cytogenetic issues are big in deciding AML relapse risk. Some genetic changes raise the risk of coming back. For example, FLT3 and NPM1 mutations have different risks.
Cytogenetic tests look at leukemia cell chromosomes. They tell us about relapse risk. People with bad cytogenetic signs are more likely to relapse.
Treatment Response and Minimal Residual Disease
How well you respond to first treatment and MRD levels are key. If you’re in complete remission but MRD is there, you’re at higher risk. MRD tests help find who needs extra or different treatments.
Good treatment plans depend on your risk and how you react to treatment. If you don’t respond well or have high MRD, you might get stronger treatments or join clinical trials.
Patient-Specific Risk Factors
Things like age, health, and other health issues also affect AML relapse risk. Older people or those with health problems might face higher risks. This is because they might not handle strong treatments well or have weaker immune systems.
- Age and overall health status
- Presence of comorbidities
- Genetic and cytogenetic risk profiles
- Response to initial treatment
Knowing these risk factors helps doctors make treatment plans just for you. This might lower the chance of AML coming back and improve your health.
Monitoring and Early Detection of Acute Myeloid Leukemia Recurrence
Watching for AML recurrence is key in post-remission care. It helps catch any signs early. After remission, a follow-up plan is needed to spot relapse quickly.
Follow-up Protocols After Remission
After AML remission, regular check-ups are vital. These include:
- Regular blood count checks to monitor for abnormal cell counts.
- Bone marrow biopsies at scheduled intervals to assess for any signs of leukemia.
- Imaging studies as necessary to check for any signs of disease recurrence.
These visits help doctors keep a close eye on the patient. They can adjust the care plan as needed.
Molecular Monitoring Techniques
Advanced tests are key in catching AML recurrence early. These include:
- Polymerase Chain Reaction (PCR) to detect specific genetic mutations associated with AML.
- Next-Generation Sequencing (NGS) to identify minimal residual disease.
These tests help doctors spot molecular changes that might mean relapse. They can catch it before symptoms show.
Early Signs and Symptoms of Relapse
Knowing the early signs of AML relapse is important. These include:
- Unexplained fatigue or weakness.
- Frequent infections or fever.
- Easy bruising or bleeding.
- Pain in the bones or joints.
Spotting these signs early can lead to quicker medical help. This can improve treatment outcomes.
The table below outlines key points for monitoring and early detection of AML recurrence:
| Monitoring Aspect | Description | Frequency |
|---|---|---|
| Blood Count Checks | Monitoring for abnormal cell counts | Regular intervals |
| Bone Marrow Biopsies | Assessing for signs of leukemia | Scheduled intervals |
| Molecular Monitoring | Detecting minimal residual disease | As recommended by healthcare provider |
Timeframes for AML Relapse After Remission
Acute Myeloid Leukemia (AML) can come back at different times after treatment. It’s important for doctors to know these times to help patients. The time a patient stays in remission is key, as relapse can happen soon, in the middle, or later.
Early Relapse (Within First Year)
Relapse in the first year is often harder to treat. It can happen because of leftover cancer cells or because the treatment doesn’t work well.
It’s very important to catch early relapse early. Regular check-ups and tests help find it quickly.
Intermediate Relapse (1-3 Years)
Relapse between 1-3 years is called intermediate. The risk of it happening is high, so doctors keep a close eye on patients.
What happens during this time can depend on the patient’s genes and how they first responded to treatment. Knowing this helps doctors plan the best follow-up care.
Late Relapse (Beyond 3 Years)
Late relapse, happening more than three years after treatment, is less common but serious. Patients in this group might have different reasons for their relapse.
For these patients, it’s important to look at their treatment history and health again. This helps decide the best way to handle the relapse.
To understand AML relapse better, let’s look at some data:
| Relapse Timeframe | Characteristics | Prognosis |
|---|---|---|
| Early Relapse (<1 year) | Often associated with minimal residual disease and treatment resistance | Generally poorer |
| Intermediate Relapse (1-3 years) | Influenced by genetic profile and initial treatment response | Variable |
| Late Relapse (>3 years) | Less common; may have different underlying factors | Can be more favorable with appropriate treatment |
Knowing when AML relapse can happen is key to better treatment plans. By understanding what affects relapse risk, doctors can work to prevent it and manage it better.
Treatment Approaches for Relapsed AML
When AML comes back, doctors need to rethink how to treat it. Fighting relapsed AML is tough. It requires a detailed plan to tackle the disease’s many challenges.
Salvage Chemotherapy Options
Salvage chemotherapy is key in treating relapsed AML. The right chemotherapy depends on several things. These include the patient’s past treatments, how long they were in remission, and their current health.
- Re-induction regimens: These are strong chemotherapy plans to get a second remission.
- High-dose cytarabine: This is often used in salvage therapy, mainly for those with a long first remission.
- Fludarabine-based regimens: New combos like FLT3 inhibitors with chemotherapy are being tested.
Stem Cell Transplantation for Relapsed Disease
Allogeneic stem cell transplantation might cure some patients with relapsed AML who get a second remission. Whether to do the transplant depends on the patient’s age, health, and if they have a good donor.
Novel Therapies and Clinical Trials
The field of AML treatment is changing fast. New treatments for relapsed disease are being looked into. These include:
- Targeted therapies: Drugs that focus on specific genetic flaws, like FLT3 inhibitors and IDH1/2 inhibitors.
- Immunotherapies: New ways like CAR-T cell therapy and bispecific antibodies are being studied.
- Clinical trials: Joining clinical trials lets patients try new treatments not yet available to everyone.
Knowing the outlook for AML recurrence and spotting recurring AML symptoms is key. By mixing old and new treatments, doctors can create plans that meet each patient’s needs.
Conclusion
Acute myeloid leukemia (AML) recurrence is a big challenge. It’s caused by many factors like genetics, molecular changes, and clinical aspects. Knowing these is key to finding better treatments and helping patients.
We’ve looked at AML recurrence from different angles. This includes how long patients stay in remission and what makes them more likely to relapse. Some patients stay in remission for a long time, while others relapse quickly.
Genetic and molecular risks, how well a patient responds to treatment, and the presence of cancer cells after treatment are important. Research into new treatments is vital. It helps us tackle AML recurrence and improve patient care.
We’re working hard to understand AML better and find better treatments. Our goal is to provide top-notch healthcare and support to patients with AML recurrence. We aim to improve their care and outcomes.
FAQ
What is acute myeloid leukemia (AML) remission, and how is it defined?
AML remission means there are no leukemia cells in the bone marrow and blood. Complete remission (CR) means the bone marrow and blood counts return to normal.
What are the types of remission in AML, and how do they differ?
AML remission comes in two types: complete remission (CR) and partial remission (PR). CR means the bone marrow and blood counts are normal. PR means there’s a big drop in leukemia cells but not all are gone.
What are the initial remission rates after treatment for AML, and how do they vary by age?
About 60-70% of adults get remission after treatment. But, older adults have lower chances of keeping remission.
What factors affect the duration of AML remission?
Several things can affect how long AML remission lasts. These include genetic mutations, how well the first treatment works, and the presence of minimal residual disease (MRD).
Why does AML recurrence happen, and what are the underlying biological mechanisms?
AML recurrence happens because of leftover disease and cancer stem cells. Treatment resistance also makes it hard to manage AML.
What are the risk factors for AML relapse, and how can they be identified?
Certain genetic and cytogenetic factors, how well the first treatment works, and MRD status predict relapse. Age and health conditions also play a role.
How can AML recurrence be monitored and detected early?
Regular check-ups and molecular tests help find relapse early. This allows for quick action.
What are the typical timeframes for AML relapse after remission?
AML relapse can happen early (in the first year), intermediate (1-3 years), or late (more than 3 years) after remission.
What treatment approaches are available for relapsed AML?
Treatments for relapsed AML include salvage chemotherapy, stem cell transplantation, and new therapies. Clinical trials also offer new treatments.
How can managing AML recurrence improve patient outcomes?
Knowing what causes AML recurrence and finding effective treatments can help patients live better lives.
What is the prognosis for AML recurrence, and how can it be managed?
The outlook for AML recurrence depends on genetic factors and how well the treatment works. Effective treatments like salvage chemotherapy and stem cell transplantation can help.
Can AML recurrence be prevented, and what strategies can be employed?
While we can’t prevent AML recurrence completely, early detection and molecular monitoring can help. New therapies and clinical trials also offer hope.
References
- American Cancer Society (Cancer.org): AML Response Rates
- Haematologica (European Hematology Association): Genomic Classification of AML
- Cancer Research UK: Acute Myeloid Leukaemia (AML) Survival
- PubMed Central (NCBI): Predictive Factors for Outcome in Elderly Patients with AML
- Nature: Risk Factors and Predictors for AML
FAQ
What is acute myeloid leukemia (AML) remission, and how is it defined?
AML remission means there are no leukemia cells in the bone marrow and blood. Complete remission (CR) means the bone marrow and blood counts return to normal.
What are the types of remission in AML, and how do they differ?
AML remission comes in two types: complete remission (CR) and partial remission (PR). CR means the bone marrow and blood counts are normal. PR means there’s a big drop in leukemia cells but not all are gone.
What are the initial remission rates after treatment for AML, and how do they vary by age?
About 60-70% of adults get remission after treatment. But, older adults have lower chances of keeping remission.
What factors affect the duration of AML remission?
Several things can affect how long AML remission lasts. These include genetic mutations, how well the first treatment works, and the presence of minimal residual disease (MRD).
Why does AML recurrence happen, and what are the underlying biological mechanisms?
AML recurrence happens because of leftover disease and cancer stem cells. Treatment resistance also makes it hard to manage AML.
What are the risk factors for AML relapse, and how can they be identified?
Certain genetic and cytogenetic factors, how well the first treatment works, and MRD status predict relapse. Age and health conditions also play a role.
How can AML recurrence be monitored and detected early?
Regular check-ups and molecular tests help find relapse early. This allows for quick action.
What are the typical timeframes for AML relapse after remission?
AML relapse can happen early (in the first year), intermediate (1-3 years), or late (more than 3 years) after remission.
What treatment approaches are available for relapsed AML?
Treatments for relapsed AML include salvage chemotherapy, stem cell transplantation, and new therapies. Clinical trials also offer new treatments.
How can managing AML recurrence improve patient outcomes?
Knowing what causes AML recurrence and finding effective treatments can help patients live better lives.
What is the prognosis for AML recurrence, and how can it be managed?
The outlook for AML recurrence depends on genetic factors and how well the treatment works. Effective treatments like salvage chemotherapy and stem cell transplantation can help.
Can AML recurrence be prevented, and what strategies can be employed?
While we can’t prevent AML recurrence completely, early detection and molecular monitoring can help. New therapies and clinical trials also offer hope.