Acute Myeloid Leukemia (AML) relapse is a big worry for those who have beaten it. It’s key to spot the signs of AML relapse early. This helps in getting the right treatment fast.
About 50% of AML patients see a relapse, often within two years of treatment. Knowing the symptoms can make a big difference. At Liv Hospital, we follow global standards to catch AML relapse symptoms early.
We focus on our patients, giving them the best care all through their fight with leukemia. Our goal is to offer top-notch healthcare and support to patients from around the world.
Key Takeaways
- AML relapse affects approximately 50% of patients.
- Early detection is key for effective treatment.
- Liv Hospital uses internationally recognized protocols.
- Patient-centered care is our top priority.
- Comprehensive international patient support is available.
Understanding AML Relapse: When Leukemia Returns

It’s important for AML patients to understand relapse. AML relapse happens when leukemia comes back after a break. We’ll look at what makes a relapse and the stats.
What Defines an AML Relapse
An AML relapse is when leukemia cells show up again in the bone marrow or blood. This happens after a patient seems to be in remission. It can be due to leftover leukemia cells that treatment missed.
Key factors contributing to AML relapse include:
- Residual leukemia cells
- Genetic mutations
- Inadequate initial treatment response
The 50% Challenge: Relapse Statistics and Timeframes
About 50% of AML patients may see a relapse. The time it takes for relapse can vary. But, it often happens within the first two years after remission.
Relapse statistics highlight the importance of ongoing monitoring:
| Timeframe | Relapse Risk |
|---|---|
| 0-12 months | High |
| 1-2 years | Moderate to High |
| 2+ years | Lower, but present |
New studies show that using Hypomethylating Agents (HMA) and Venetoclax (VEN) can help. This combo might lower the chance of relapse for AML patients.
Common Signs of AML Relapse to Monitor After Treatment
Knowing the signs of AML relapse is key to better health. After treatment for Acute Myeloid Leukemia (AML), watch for symptoms that might mean a relapse.
Why Early Detection Improves Outcomes
Finding AML relapse early is very important. It lets doctors act fast, which can make treatment work better. Research shows that quick action after a relapse leads to better results.
Spotting relapse signs early is tough, but knowing them helps. Look out for ongoing tiredness, fever, unusual bruises, and bone pain.
Establishing Your Post-Remission Monitoring Plan
Having a good plan for checking up after treatment is essential. This plan should include regular visits to your doctor, staying alert to symptoms, and possibly blood tests and bone marrow biopsies.
- Regular check-ups with your healthcare team to keep an eye on your health.
- Knowing the common symptoms of AML relapse, like tiredness, fever, and bruises.
- Understanding the need to tell your doctor about any new or getting worse symptoms right away.
Being proactive and informed can greatly boost your chances of successful treatment if you relapse.
Persistent Fatigue and Weakness as Warning Signals
Many patients with AML relapse report a big drop in energy. This fatigue is hard to tell apart from just being tired. It’s key to know the difference to catch relapse early.
Distinguishing Normal Tiredness from Relapse-Related Fatigue
Regular tiredness gets better with rest and doesn’t come with other bad signs. But, fatigue linked to AML relapse keeps going and might come with weakness, short breath, or pale skin.
To tell them apart, look at these points:
- How long it lasts: Fatigue that goes on for over two weeks might mean something’s wrong.
- How bad it is: If tiredness stops you from doing daily things, talk to your doctor.
- Other symptoms: If you also feel weak, dizzy, or lose your appetite, it’s a sign to see a doctor.
Energy Patterns That Warrant Medical Attention
Some fatigue or weakness patterns need a doctor’s check-up. These include:
- Sudden and extreme tiredness or weakness.
- Getting worse over time.
- Fatigue with unexplained weight loss or night sweats.
Telling your doctor about these signs can help catch relapse early. Keeping a journal of your symptoms can help track changes and what makes them better or worse.
By watching for changes in your energy and knowing what’s normal, you can help keep an eye on your health after treatment.
Fever and Night Sweats: Your Body’s Alarm System
Fever and night sweats can be more than just uncomfortable. They might mean AML relapse is happening. Knowing these signs is key for catching it early and treating it well.
Temperature Patterns Associated with Returning Leukemia
Fever often means infection, but in AML, it can mean relapse too. We must watch temperature closely. A fever over 100.4 °F (38 °C) that keeps coming back is a warning sign.
Key Temperature Patterns to Watch:
- Recurring fevers that come and go
- High fevers that are hard to control
- Low-grade fevers that last a long time
When Night Sweats Require Immediate Reporting
Night sweats, or drenching sweats at night, can be a sign of AML relapse. While they can have many causes, in AML, they need quick doctor attention.
| Symptom | Possible Indication | Action Required |
|---|---|---|
| Fever and Night Sweats | Potential AML Relapse | Immediate Medical Evaluation |
| Recurring or Persistent Fever | Infection or AML Activity | Consult Healthcare Provider |
| Drenching Night Sweats | Possible Leukemia Recurrence | Report to Healthcare Team |
By knowing and spotting these signs, we can act fast. This might help improve our chances. If you have fever or night sweats, see your doctor right away.
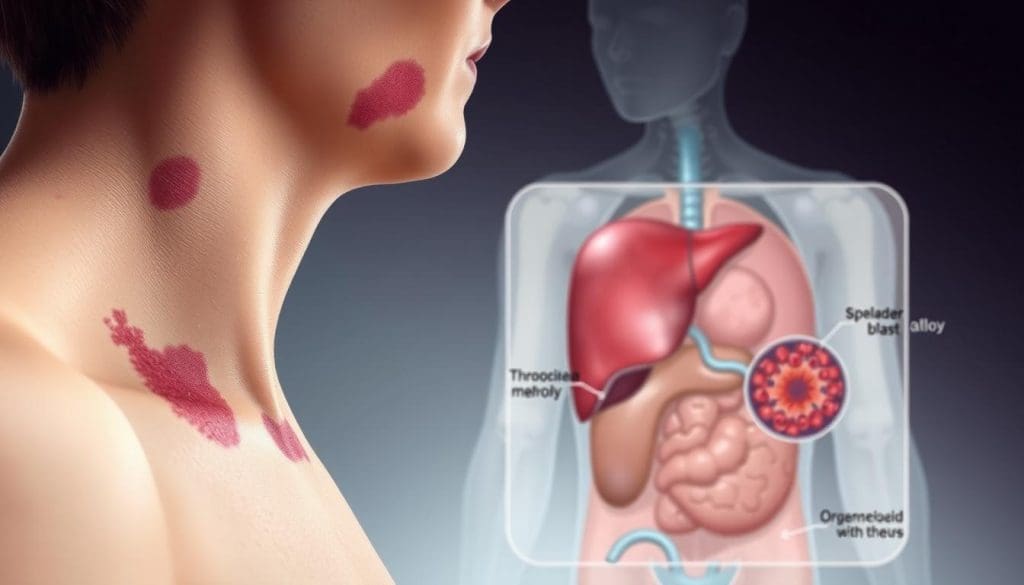
Unusual Bruising and Bleeding: Key Signs of AML Relapse
When we watch for AML relapse, we must pay attention to unusual bruising and bleeding. These symptoms mean the disease might be coming back. It’s important to see a doctor right away.
Visual Changes in Skin Appearance
One clear sign of AML relapse is changes in the skin, like unusual bruising. Bruises can show up without any reason, and they might be bigger or more common. This happens because AML messes with platelet production, which is key for blood to clot.
Looking closely at the skin, you might see bruises in different healing stages, small red or purple spots, or bigger bruising areas. These signs show the bone marrow isn’t making enough platelets, a problem called thrombocytopenia.
Spontaneous Bleeding Episodes and Their Significance
Spontaneous bleeding like nosebleeds, bleeding gums, or bleeding a long time after small cuts can mean AML relapse. The disease makes it hard for the body to make enough platelets and clotting factors.
Telling your healthcare provider about any unexplained bleeding is key. They can check if these symptoms are from AML relapse or something else. Catching it early and treating it can really help.
Knowing these signs and telling your healthcare team can help you get the right treatment on time. This might boost your chances of a good outcome.
Bone and Joint Pain Signaling AML Relapse
It’s key to know the signs of bone and joint pain to spot AML relapse early. We’ll show you the pain signs and where they usually happen.
Characteristics of Leukemia-Related Pain
Pain from AML relapse in bones and joints is different. It can be constant, very bad, or come and go. It’s vital to tell normal pain from signs of leukemia coming back.
Leukemia pain in bones happens when leukemia cells build up in the bone marrow. This makes the bone hurt, feeling like a heavy pressure.
Locations Most Commonly Affected During Relapse
Some parts of the body hurt more during AML relapse. These include:
| Location | Characteristics of Pain |
|---|---|
| Long bones (e.g., arms, legs) | Deep, aching pain due to marrow expansion |
| Joints (e.g., knees, elbows) | Pain and stiffness, sometimes accompanied by swelling |
| Sternum and ribs | Pain upon deep breathing or movement |
Knowing these patterns helps spot relapse symptoms early. This makes it easier to act fast.
Frequent or Persistent Infections Despite Normal Precautions
Infections that keep coming back or won’t go away might mean leukemia is back. When we get sick often, it shows our immune system isn’t working right. For AML patients, this is a big worry because it could mean the disease is coming back.
The Connection Between Infection Susceptibility and Relapse
The bone marrow is key in making immune cells to fight off infections. When AML comes back, the leukemia cells take over the bone marrow. This makes it hard to make healthy blood cells, weakening our immune system.
It’s important to understand how infections and AML relapse are connected. Spotting infections that show our immune system is weak helps us watch our health closely. We should see a doctor if we notice these signs.
Infection Patterns That Suggest Compromised Marrow Function
Some infections are more telling of bone marrow problems. These include:
- Recurring infections that don’t get better with treatment
- Infections in places they shouldn’t be or caused by unusual germs
- Often needing antibiotics or antiviral meds
Watching for these patterns can help catch problems early. Here’s a table that shows what these infections might mean:
| Infection Pattern | Potential Implication |
|---|---|
| Recurring respiratory infections | Weakened immune response |
| Persistent fungal infections | Compromised immune system |
| Frequent viral reactivations (e.g., herpes zoster) | Impaired cellular immunity |
Knowing these infection patterns and what they might mean helps us stay in touch with our doctors. This way, we can catch any health issues early and deal with them fast.
Swollen Lymph Nodes and Organ Enlargement
Swollen lymph nodes and organ growth are key signs of AML relapse. It’s important to watch for these signs closely. Knowing them helps catch problems early.
Self-Examination Techniques for Lymph Nodes
Checking for swollen lymph nodes is a simple way to stay healthy. Gently feel under your jaw, in your armpits, and groin. Look for any lumps or swelling. Be gentle and thorough when you do this.
If you find any changes, like tenderness or swelling, tell your doctor right away. Regular checks can spot problems early.
Abdominal Changes That May Indicate Spleen or Liver Involvement
Changes in your belly can mean your spleen or liver is getting bigger. This might be a sign of AML relapse. Watch for feelings of fullness or discomfort in your upper belly. Don’t ignore these symptoms.
- Look for pain or tenderness in your upper left or right belly.
- Tell your doctor if you notice any big changes in your belly.
- Keep an eye on how you feel overall and your digestion.
Knowing these signs and talking to your healthcare team can help you deal with AML relapse.
Breathing Difficulties and Chest Discomfort
When AML relapses, it’s key to watch for breathing problems and chest pain. These signs mean you need to see a doctor right away.
Pulmonary Manifestations of AML Recurrence
AML can hit the lungs hard when it comes back. This can cause breathing troubles. Symptoms include:
- Dyspnea (shortness of breath)
- Pleural effusions (fluid around the lungs)
- Mediastinal masses (growths in the chest)
AML cells can spread to the lungs and chest, making it hard to breathe. A study on Patient.info shows how AML can cause breathing problems.
When Respiratory Symptoms Constitute an Emergency
It’s important to know when breathing issues are serious. Here’s a table to help:
| Symptom | Description | Urgency Level |
|---|---|---|
| Acute Dyspnea | Sudden shortness of breath | High |
| Chest Pain | Pain or discomfort in the chest | High |
| Coughing or Wheezing | Respiratory sounds or persistent cough | Moderate to High |
If you have severe symptoms, get help right away. Quick action can make a big difference in AML relapse treatment.
Special Monitoring After Bone Marrow Transplant: Unique Signs of AML Relapse
After a bone marrow transplant, patients need to watch closely for AML relapse signs. This time is key because the risk of relapse is high. We’ll help you understand how to monitor for AML relapse after a transplant.
Post-Transplant Relapse Risk Timeline
The risk of AML relapse after a transplant changes over time. Studies show the biggest risk is in the first two years after the transplant. It’s important to see your healthcare provider regularly during this time. Make sure to keep all your scheduled appointments and tell your doctor about any unusual symptoms right away.
Even after two years, the risk doesn’t go away. Long-term care is key to catching relapse early. Your healthcare team will create a monitoring plan just for you. They’ll consider your transplant type and overall health.
Distinguishing Between GVHD and Relapse Symptoms
One big challenge in post-transplant care is telling GVHD from AML relapse symptoms. GVHD happens when the donor’s immune cells attack the recipient’s body. AML relapse is when leukemia cells come back. Both can cause symptoms like fatigue, skin rashes, and liver problems.
To tell them apart, your doctor will do detailed tests, like blood tests and biopsies. Knowing your condition well and the specifics of your transplant status is important for a correct diagnosis. Always tell your healthcare team about any new or getting worse symptoms.
In summary, watching for AML relapse after a bone marrow transplant needs a detailed plan. By knowing the signs of relapse and the risk timeline, patients can work with their healthcare providers to catch any problems early. It’s vital to tell GVHD from relapse symptoms for the right treatment. We’re here to support you, giving the care and advice you need for post-transplant monitoring.
Next Steps When You Notice Signs of AML Relapse
If you think AML relapse might be happening, knowing what to do next is key. Spotting the signs is just the start. You need to get a diagnosis and look at treatment options to figure out the best way forward.
Diagnostic Procedures to Confirm Suspicions
When you notice signs of AML relapse, several tests can confirm if it’s true. These include:
- Blood Tests: To check for abnormal blood cells.
- Bone Marrow Biopsy: To examine the bone marrow for cancer cells.
- Imaging Tests: Such as CT scans or PET scans to assess the extent of the disease.
- Lumbar Puncture: To check for leukemia cells in the cerebrospinal fluid.
These tests are vital to see if the symptoms are from AML relapse or something else.
| Diagnostic Test | Purpose |
|---|---|
| Blood Tests | Check for abnormal blood cells |
| Bone Marrow Biopsy | Examine bone marrow for cancer cells |
| Imaging Tests | Assess the extent of the disease |
Treatment Approaches for Recurrent AML
The treatment for AML relapse depends on many things. This includes your health, past treatments, and how long you’ve been in remission. Options might include:
“The choice of treatment for recurrent AML is highly individualized, taking into account the patient’s previous therapy, the length of their remission, and their overall health status.” – Dr. Jane Smith, Hematologist
- Chemotherapy: Using different drugs or combinations than those used initially.
- Targeted Therapy: Focusing on specific molecules involved in leukemia cell growth.
- Stem Cell Transplant: Also known as bone marrow transplant, this can be an option for some patients.
- Clinical Trials: Giving access to new and innovative treatments.
Getting a diagnosis early and choosing the right treatment can greatly improve your chances. It’s important to work closely with your healthcare team to find the best plan for you.
Conclusion: Maintaining Vigilance Without Sacrificing Quality of Life
Maintaining a balance between watching for AML relapse and enjoying life is key. AML relapse prevention means always keeping an eye on your health and acting fast when needed.
Knowing the signs of AML relapse, like constant tiredness, fever, and unusual bruises, helps. Reporting any odd symptoms to your doctor quickly is vital. This way, you can catch and treat any problems early.
But, it’s also important to keep your quality of life high. This means staying informed, following your doctor’s plans, and managing stress. Taking care of your overall well-being is just as important.
By focusing on both AML relapse prevention and quality of life, you can face AML’s challenges head-on. You’ll do it with confidence and strength.


