Last Updated on November 6, 2025 by
Myelodysplastic Syndrome (MDS) is a group of disorders that affect blood cell production. It can lead to serious health issues, including myelodysplastic syndrome cancer. A surprising fact is that MDS affects many people worldwide, with different outcomes based on the subtype and health.
It’s important to know if MDS can get better on its own. The disease’s progression varies, with some experiencing slow growth and others facing aggressive forms. Treatment options, such as myelodysplastic syndrome treatments, are key in managing the condition and improving life quality.
Key Takeaways
- Myelodysplastic Syndrome is a group of disorders affecting blood cell production.
- The prognosis for MDS varies significantly among individuals.
- Understanding the subtype of MDS is critical for determining the best treatment.
- Myelodysplastic syndrome treatments can help manage the condition.
- Some patients may experience a slow progression of the disease.
What Is Myelodysplastic Syndrome (MDS)?
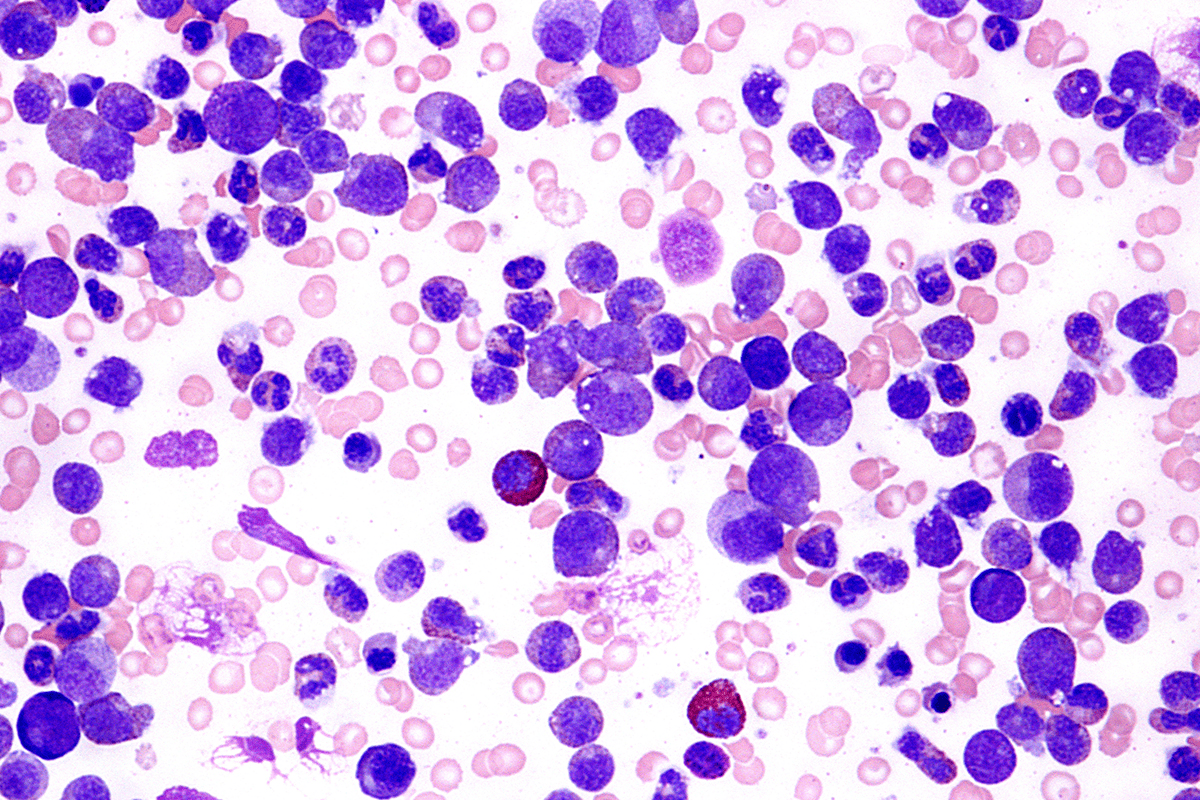
Myelodysplastic syndrome (MDS) is a group of disorders that affect the bone marrow. It makes it hard for the bone marrow to produce healthy blood cells. This leads to health problems. Knowing about MDS helps understand its effects and treatment options.
Definition and Basic Characteristics
MDS is when the bone marrow can’t make enough blood cells. This means not enough red, white blood cells, and platelets. These cells are key for oxygen, fighting off infections, and blood clotting. The severity and how fast it gets worse can vary a lot.
How MDS Affects Blood Cell Production
In healthy people, the bone marrow makes blood cells that work well. But with MDS, the bone marrow makes bad or dysplastic cells. These cells don’t last long or work right, so treatments are needed to help.
Relationship to Leukemia
MDS can turn into mds cancer, like acute myeloid leukemia (AML). How likely this is depends on the type of MDS and other things. Knowing this helps pick the right treatment for mds disease and what to expect.
The link between MDS and leukemia shows why early and good myelodysplastic syndrome treatment is key. It can help stop or slow down worse conditions like AML.
Types and Classification of MDS
Myelodysplastic Syndrome (MDS) is divided into types based on different systems. These systems help predict how the disease will progress. Knowing these classifications is key to finding the right myelodysplastic syndrome treatmentshttps://bloodcancerunited.org/blood-cancer/myelodysplastic-syndromes-mds.
WHO Classification System
The World Health Organization (WHO) system is a main way to sort MDS. It looks at blast cells in the bone marrow, genetic changes, and cell line dysplasia. This system is important for picking the right treatment.
IPSS and IPSS-R Risk Stratification
The International Prognostic Scoring System (IPSS) and its update (IPSS-R) are key for MDS risk. They use blast cells, karyotype, and cytopenias to set risk levels. The IPSS-R is more detailed, giving a better idea of what to expect.
Low-Risk vs. High-Risk MDS
MDS patients are split into low-risk and high-risk groups. Low-risk MDS patients face a lower chance of turning into AML. They might get supportive care and less intense treatments. On the other hand, high-risk MDS patients are at a higher risk of AML. They often need stronger treatments, like mds treatment options.
It’s important for doctors to understand MDS classification and risk. This helps them tailor treatments for each patient. The choice of mds blood cancer treatment depends on many factors, like the patient’s health and MDS type.
For those with mds pre leukemia prognosis, watching the disease closely is key. Regular checks and quick action can help stop the disease from getting worse. The classification systems guide doctors in managing MDS, making sure patients get the best care for their specific situation.
Understanding MDS Cancer: Causes and Risk Factors
It’s important to know the causes and risk factors of MDS for early detection and management. MDS, or myelodysplastic syndrome, is a group of disorders. They are caused by poorly formed or dysfunctional blood cells, leading to bone marrow failure.
Primary vs. Secondary MDS
MDS can be divided into primary (de novo) and secondary MDS. Primary MDS happens without a known cause or previous exposure to harmful substances. On the other hand, secondary MDS is linked to previous exposure to chemotherapy, radiation, or certain environmental toxins. Secondary MDS often has a poorer prognosis.
Age and Genetic Factors
Age is a big risk factor for MDS, with most cases diagnosed in people over 70. Genetic mutations also play a key role, with certain inherited conditions increasing the risk. Acquired genetic mutations over time can also contribute to the disease.
Environmental Exposures
Exposure to certain environmental toxins, like benzene and pesticides, increases the risk of MDS. Occupational exposure to these substances is very hazardous. This highlights the need for protective measures in high-risk workplaces.
Previous Cancer Treatments
Previous cancer treatments, including chemotherapy and radiation therapy, can raise the risk of secondary MDS. The risk depends on the type and intensity of the treatment, as well as individual patient factors.
Signs, Symptoms, and Diagnosis of MDS
Spotting the signs of MDS is the first step towards getting a diagnosis. This involves several tests and procedures. Myelodysplastic Syndrome (MDS) shows nonspecific symptoms, making it hard to diagnose.

Common Symptoms
People with MDS may feel tired, weak, and have trouble breathing. These issues often stem from anemia, where the body lacks red blood cells.
- Fatigue and weakness due to anemia
- Shortness of breath
- Pale skin
- Increased risk of infections
- Easy bruising or bleeding
At times, MDS doesn’t show symptoms early on. It’s found during blood tests for other reasons.
Diagnostic Tests and Procedures
To diagnose MDS, doctors use blood tests, bone marrow biopsies, and more. These steps help figure out if you have MDS and how severe it is.
| Diagnostic Test | Purpose |
| Complete Blood Count (CBC) | Measures the levels of different blood cells |
| Bone Marrow Biopsy | Examines the bone marrow for abnormal cells |
| Cytogenetic Analysis | Identifies genetic abnormalities in bone marrow cells |
Distinguishing MDS from Other Blood Disorders
It’s tricky to tell MDS apart from other blood issues like anemia or leukemia. A detailed check-up, including blood tests and bone marrow exams, is needed for a correct diagnosis.
Diagnosing MDS involves looking at symptoms, blood test results, and bone marrow biopsies. Getting the right diagnosis is key to finding the right treatment.
The Natural Progression of MDS
Myelodysplastic Syndrome (MDS) can change in unpredictable ways. This makes it key to have a treatment plan that fits each person. Knowing how MDS progresses is vital for managing it well.
Typical Disease Course
The way MDS progresses varies a lot from person to person. Some may stay stable for years, while others see the disease get worse fast. The survival rate for MDS patients depends on many things, like the type of MDS and the patient’s health.
A study in the Journal of Clinical Oncology showed that MDS patients’ survival times ranged from 1.4 to 5.4 years. The myelodysplastic syndrome prognosis is better for those with lower-risk MDS.
| Risk Category | Median Survival Time (Years) |
| Low Risk | 5.4 |
| Intermediate-1 Risk | 2.7 |
| Intermediate-2 Risk | 1.8 |
| High Risk | 1.4 |
Factors Affecting Disease Progression
Many things can affect how MDS progresses. These include the patient’s age, certain genetic mutations, and how well the first treatment works. As MDS gets worse, the bone marrow makes fewer healthy blood cells.
“The progression of MDS is influenced by a complex interplay of genetic and environmental factors.” – Hematologist
It’s important to keep checking on the disease and adjust treatments as needed.
Transformation to Acute Myeloid Leukemia
One big risk with MDS is turning into acute myeloid leukemia (AML). This happens when the bone marrow cells grow out of control.
People with higher-risk MDS are more likely to turn into AML. This shows why it’s so important to watch the disease closely and act fast.
Understanding how MDS progresses and what affects it helps both patients and doctors make better treatment choices.
Can MDS Resolve Without Treatment?
To understand if MDS can go away on its own, we need to look at cases of spontaneous remission. Myelodysplastic Syndrome (MDS) makes it hard for the bone marrow to create healthy blood cells. Sometimes, MDS can get better without treatment.
Documented Cases of Spontaneous Remission
There are cases where MDS patients got better without treatment. These cases are important because they show what might help MDS patients. Spontaneous remission in MDS is rare, but studying these cases can help us understand the disease better.

Statistical Likelihood of Spontaneous Resolution
It’s hard to say how often MDS can get better on its own because it varies a lot. But, research shows that spontaneous remission happens in a small number of MDS patients. Different studies have found different rates, but it’s not common.
Factors Associated with Spontaneous Improvement
Some things can help MDS patients get better on their own. These include certain genes, immune system factors, and maybe even the environment. Knowing these can help find patients who might get better without treatment and help create new treatments.
In summary, while MDS getting better without treatment is rare, it has happened and is being studied. More research on what helps MDS patients get better could lead to better treatments for MDS.
MDS Survival Rates and Prognosis Factors
MDS survival rates depend on many factors. It’s key to know these for good disease management. The prognosis for Myelodysplastic Syndrome (MDS) patients varies a lot.
Survival Statistics by Risk Category
MDS is split into risk groups. This is based on scoring systems like the International Prognostic Scoring System (IPSS) and its update, IPSS-R. These systems forecast survival chances and the risk of turning into acute myeloid leukemia (AML).
| Risk Category | Median Survival (Years) | Risk of AML Progression |
| Low Risk | 8.8 | Low |
| Intermediate-1 | 5.3 | Moderate |
| Intermediate-2 | 2.7 | High |
| High Risk | 1.6 | Very High |
The table shows survival years and AML risk for different MDS risks. Knowing these stats is vital for treatment choices.
Prognostic Indicators
Several indicators predict MDS patient outcomes. These include:
- Cytogenetic abnormalities
- Bone marrow blast percentage
- Number of cytopenias
- Patient’s age and overall health
These help sort patients by risk and guide treatment plans.
Quality of Life Considerations
Survival and prognosis are important, but quality of life matters too. Managing symptoms, transfusion needs, and the disease’s mental impact are key to a patient’s well-being.
Effective MDS management involves understanding survival, prognosis, and quality of life. This approach allows for tailored care that meets each patient’s needs.
Standard Treatment Approaches for MDS
Treatment for Myelodysplastic Syndrome (MDS) involves many steps. These steps are based on the patient’s risk level and health. The main goal is to manage symptoms, improve life quality, and slow disease progress.
Choosing the right treatment depends on several things. These include the MDS subtype, the patient’s age, health, and other medical conditions. Knowing these helps doctors create a treatment plan that fits each patient’s needs.
Supportive Care Options
Supportive care is key in managing MDS. It aims to ease symptoms and enhance life quality. This care includes:
- Blood transfusions to fight anemia and reduce tiredness
- Medicines to boost blood cell production
- Antibiotics for infections
- Growth factors to increase blood cell counts
For those with lower-risk MDS, supportive care is often the main treatment. It focuses on symptom management and maintaining quality of life.
Medication Therapies
Some patients may need medication to treat MDS. These treatments include:
- Immunosuppressive therapy to calm the immune system’s attack on the bone marrow
- Lenalidomide for patients with a specific genetic deletion (del(5q))
- Hypomethylating agents like azacitidine and decitabine to improve blood cell production
These medicines can help manage the disease. They can also reduce the need for blood transfusions and may improve survival chances.
Stem Cell Transplantation
Stem cell transplantation is a possible cure for MDS. It replaces the patient’s diseased bone marrow with healthy stem cells from a donor.
This treatment is usually for those with higher-risk MDS or who haven’t responded to other treatments. The decision to have a stem cell transplant depends on the patient’s health and the risks of the procedure.
The treatment options for MDS are complex and always changing. Patients should talk to their healthcare provider about their situation and the latest treatment options.
Watch and Wait: When Treatment May Be Delayed
The “watch and wait” approach is often used at first for managing MDS. It’s chosen when the disease isn’t immediately threatening. This method means keeping a close eye on the patient without starting treatment right away. It helps doctors understand how the disease is moving and decide the best next steps.
Criteria for Observation Approach
Choosing the “watch and wait” method depends on several things. These include the patient’s health, the type of MDS, and if they’re showing symptoms. Usually, those with lower-risk MDS and mild symptoms might start with this approach. A hematologist or oncologist will look at the patient’s situation and decide the best plan.
Key factors considered for the “watch and wait” approach include:
- The patient’s age and overall health status
- The MDS risk category, as determined by systems like IPSS-R
- The presence and severity of symptoms such as anemia, infections, or bleeding
- Blood cell counts and other relevant laboratory findings
Monitoring During Watch and Wait
During the “watch and wait” time, it’s important to keep a close eye on the patient. This is to catch any changes that might mean treatment is needed. This usually means:
- Regular blood tests to check blood cell counts
- Periodic bone marrow biopsies to see how the disease is doing
- Watching for new symptoms or if old ones get worse
Good monitoring during the “watch and wait” phase is key. It helps start treatment when it’s needed, which can improve results.
By watching MDS patients closely during the “watch and wait” time, doctors can act fast when the disease gets worse or symptoms get more serious. This helps make treatment more effective.
Lifestyle Modifications That May Impact MDS Progression
For those with MDS, making lifestyle changes can really help. Myelodysplastic Syndrome (MDS) makes it hard for the bone marrow to make healthy blood cells. While doctors’ treatments are key, changing your lifestyle can also help manage the disease.
Nutrition and Dietary Considerations
Eating well is very important for MDS patients. Not getting enough nutrients can make the condition worse. So, it’s important to eat foods that are full of good nutrients.
Nutritional Recommendations for MDS Patients:
| Nutrient | Food Sources | Benefits |
| Iron | Red meat, spinach, beans | Essential for healthy red blood cells |
| Vitamin B12 | Meat, fish, poultry, dairy products | Crucial for the production of red blood cells |
| Folate | Leafy greens, legumes, citrus fruits | Important for preventing anemia |
Exercise and Physical Activity
Staying active is good for MDS patients. It can help fight off fatigue, a common symptom.
- Benefits of Exercise:Improves cardiovascular health
- Enhances muscle strength
- Reduces fatigue
Stress Management
Stress can make MDS symptoms worse. Finding ways to manage stress is key to staying healthy.
Stress Management Techniques:
- Meditation and mindfulness
- Yoga
- Deep breathing exercises
By making these lifestyle changes, MDS patients can live better lives. They might even slow down the disease’s progress.

Complementary Approaches to Managing MDS Symptoms
Complementary approaches can help ease MDS symptoms and improve well-being. While main treatments are key, adding complementary therapies can boost quality of life. They offer extra benefits in managing symptoms.
Evidence-Based Complementary Therapies
Several therapies show promise in managing MDS symptoms. These include:
- Acupuncture: This traditional Chinese medicine helps manage pain and other symptoms.
- Meditation and Mindfulness: These practices reduce stress and improve well-being.
- Nutritional Supplements: Some supplements may help with symptoms or improve health. Always talk to a healthcare provider before adding supplements.
Patients should talk to their healthcare provider about these options. This helps find the best approach for their situation.
Approaches to Avoid
While many therapies are helpful, some should be avoided or used with caution:
- Unproven or Unregulated Treatments: Be cautious of treatments claiming to cure MDS without scientific evidence.
- Interactions with Conventional Treatments: Some therapies can interact with main MDS treatments. Always check with a healthcare provider before starting.
By choosing and using complementary therapies wisely, MDS patients can better manage symptoms and improve their quality of life.
When to Seek Medical Intervention for MDS
MDS patients should watch for warning signs that mean they need to see a doctor right away. Myelodysplastic Syndrome (MDS) is a complex condition. It needs careful watching and quick medical care to manage its progress and complications well.
Warning Signs That Require Immediate Attention
Certain symptoms and health changes mean you should see a doctor fast. These include:
- Increased fatigue or weakness that makes daily tasks hard.
- Unexplained fever or infections that keep coming back or are very bad.
- Easy bruising or bleeding that doesn’t stop or is unusual.
- Pale skin or other signs of anemia.
- Shortness of breath or trouble breathing.
If you notice any of these symptoms or if they get worse, you must get medical help.
Regular Monitoring Guidelines
It’s key for MDS patients to keep an eye on their health closely. This means:
- Regular blood tests to check blood cell counts.
- Going to follow-up appointments with a hematologist or oncologist as told.
- Telling your healthcare provider about any new or getting worse symptoms.
- Following the treatment plan and any changes made by your healthcare team.
By being alert and taking action, MDS patients can manage their condition better. Regular checks and quick medical help when needed are important for good MDS care.
Living with MDS: Patient Experiences and Coping Strategies
Living with Myelodysplastic Syndrome (MDS) is tough. It changes a person’s life, affecting them, their family, and caregivers.
Patient Perspectives
People with MDS face many challenges. They deal with physical symptoms and the emotional impact of their diagnosis. The emotional toll of MDS can be huge, leading to anxiety, depression, and fear about the future.
Understanding MDS and its treatments is key. Knowing about their disease helps patients make informed decisions about their care. It also helps them manage their symptoms better.
Support Resources
Support is vital for MDS patients. It includes healthcare professionals, support groups, and online communities. Access to good care is essential for managing the disease.
Here’s a table showing important support resources for MDS patients:
| Resource | Description | Benefits |
| Healthcare Professionals | Doctors, nurses, and other medical staff who specialize in MDS care. | Expert medical advice, treatment planning, and ongoing support. |
| Support Groups | Groups where patients can share their experiences and connect with others who have MDS. | Emotional support, practical advice, and a sense of community. |
| Online Communities | Online forums and social media groups dedicated to MDS patients and their families. | Access to a wider community, information sharing, and support from others who understand the challenges of MDS. |
By using these resources, MDS patients can handle their condition better. This improves their quality of life.
Current Research and Future Directions in MDS Treatment
New research in MDS is bringing hope to patients. Our understanding of Myelodysplastic Syndrome is getting better. This means researchers are finding new ways to help patients.
Emerging Therapies
New treatments for MDS are being tested. These include:
- Immunotherapies: These use the body’s immune system to fight cancer. They might help treat MDS.
- Targeted Therapies: These therapies focus on specific molecules in MDS. They offer a more tailored treatment.
- Gene Therapies: Scientists are looking into gene therapy. It could fix the genetic problems that cause MDS.
Clinical Trials
Clinical trials are key in finding new MDS treatments. They test new therapies to see if they work and are safe. Right now, trials are looking at many new treatments, including new medicines and transplant methods.
| Therapy Type | Description | Potential Benefits |
| Immunotherapy | Stimulates the immune system to attack cancer cells | Enhanced immune response against MDS |
| Targeted Therapy | Targets specific molecules involved in MDS progression | Personalized treatment approach with potentially fewer side effects |
| Gene Therapy | Aims to correct genetic abnormalities driving MDS | Potential for long-term remission or cure |
The future for MDS treatment looks bright. Ongoing research and trials offer hope for better care. As new therapies are developed and tested, we can expect more effective and tailored treatments.
Conclusion: Understanding the Reality of MDS Remission
Myelodysplastic Syndrome (MDS) is a complex condition. It’s important for patients and doctors to understand it well. Some patients can go into remission, but it depends on many factors.
Learning about MDS remission means knowing the different types and how they progress. Patients need to work with their doctors to find the right treatment. This could be supportive care, medicines, or stem cell transplants.
More research on MDS is needed to help patients. New treatments and clinical trials give hope. Support from doctors, family, and friends is key for those with MDS.
Patients can improve their life by learning about MDS and its treatments. This knowledge helps them make better choices. It can also help them live longer and better with MDS.
FAQ
What is Myelodysplastic Syndrome (MDS)?
Myelodysplastic Syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This affects the bone marrow’s ability to produce healthy blood cells, leading to various health issues.
Can MDS resolve on its own?
While rare, there have been cases of MDS patients getting better on their own. But, the chance of this happening depends on several factors. These include the type and risk category of MDS.
What are the common symptoms of MDS?
Common symptoms of MDS include fatigue, weakness, and pale skin. Patients may also experience shortness of breath and frequent infections. Some may bleed or bruise easily.
How is MDS diagnosed?
MDS is diagnosed through blood tests, bone marrow biopsy, and other procedures. These tests help find and measure the severity of MDS.
What are the treatment options for MDS?
Treatment options for MDS include supportive care, medication, and stem cell transplantation. The choice depends on the patient’s risk category and health.
What is the “watch and wait” approach for MDS?
The “watch and wait” approach involves monitoring the patient’s condition without immediate treatment. It’s often recommended for low-risk MDS patients.
modifications impact MDS progression?Can lifestyle
Yes, lifestyle changes like a balanced diet and regular exercise may help manage MDS symptoms. They may also impact disease progression.
What are the survival rates for MDS patients?
Survival rates for MDS patients vary based on risk category and other factors. Generally, low-risk MDS patients have a better prognosis than high-risk patients.
Are there any complementary therapies for MDS?
Some evidence-based complementary therapies, like acupuncture and meditation, may help manage MDS symptoms. It’s important to consult with a healthcare provider before starting any therapy.
When should I seek medical intervention for MDS?
Patients should seek medical attention if they experience severe fatigue, frequent infections, or bleeding. Regular monitoring is also key to managing the disease effectively.
What are the emerging therapies for MDS?
Emerging therapies for MDS include new medications and immunotherapies. Clinical trials are ongoing to evaluate their safety and efficacy.
Where can I find support resources for MDS?
Patients and caregivers can find support through organizations dedicated to MDS and blood cancer research. Online forums and support groups are also available.