Last Updated on October 28, 2025 by

We are leading the way in medical innovation, looking into the huge promise of human embryonic cells in regenerative medicine. These cells come from the inner cell mass of a blastocyst, a stage reached 4-7 days after fertilization. They can turn into any cell type in the human body, forming the three embryonic layers.
In our journey into embryonic stem cell research, we see how important these cells are. Their ability to become any cell type is key for understanding how we develop and for new treatments. The places where we find these cells, like IVF embryos, are key for our research.
Key Takeaways
- Embryonic stem cells are pluripotent cells found in the inner cell mass of a blastocyst.
- These cells can differentiate into all cell types in the human body.
- Their ability to form the three embryonic layers makes them significant in medical research.
- Sources of embryonic stem cells include IVF-derived embryos.
- Understanding embryonic stem cells is key for moving forward in regenerative medicine.
Understanding Embryonic Stem Cells
Embryonic stem cells are key in stem cell research. They can self-renew and differentiate, making them vital for studying human development and medical therapies. We will look into their definition, traits, and where they are found in the human body.
Definition and Characteristics
These cells can self-renew and turn into different cell types. This makes them very useful for research and medical uses. They can become any cell type, helping scientists study disease development and possibly replace damaged cells.
They are known for their pluripotency, meaning they can become every type of body cell. This is a major focus in research, as it could lead to regenerative medicine and tissue engineering.
Where Are Embryonic Stem Cells Found
Embryonic stem cells are in the inner cell mass of the blastocyst. This happens about 5-6 days after fertilization. The blastocyst has two main cell groups: the trophoblast and the inner cell mass. The inner cell mass is where embryonic stem cells come from, and they are then grown for research.
Knowing where and how to get embryonic stem cells from the blastocyst is key for research progress. The process involves careful steps to keep their ability to self-renew and become any cell type.
The Biology of Embryonic Development
Embryonic development starts with fertilization. It’s a complex process with many stages. These stages lead to the formation of a blastocyst, which is key for getting embryonic stem cells.
From Fertilization to Blastocyst Formation
Fertilization is when a sperm meets an egg, creating a zygote. This zygote goes through several divisions without growing much. It turns into a morula, then a blastocyst.
The blastocyst has two main parts: the outer trophoblast layer and the inner cell mass (ICM). The ICM is where embryonic stem cells come from.
Embryonic Stem Cells Differentiate to Form the Three Embryonic Layers
Embryonic stem cells from the ICM can turn into three main germ layers. These are ectoderm, mesoderm, and endoderm. They are the building blocks of all body tissues.
The ectoderm makes the nervous system and skin. The mesoderm forms muscles and blood vessels. The endoderm creates the digestive tract lining and other organs.
| Germ Layer | Tissues and Organs Derived |
|---|---|
| Ectoderm | Nervous system, skin, hair, nails |
| Mesoderm | Muscles, bones, blood vessels, connective tissues |
| Endoderm | Digestive tract lining, liver, pancreas, lungs |
Knowing how embryonic stem cells turn into germ layers is important. It shows their huge promise in regenerative medicine and tissue engineering.
How Are Embryonic Stem Cells Obtained
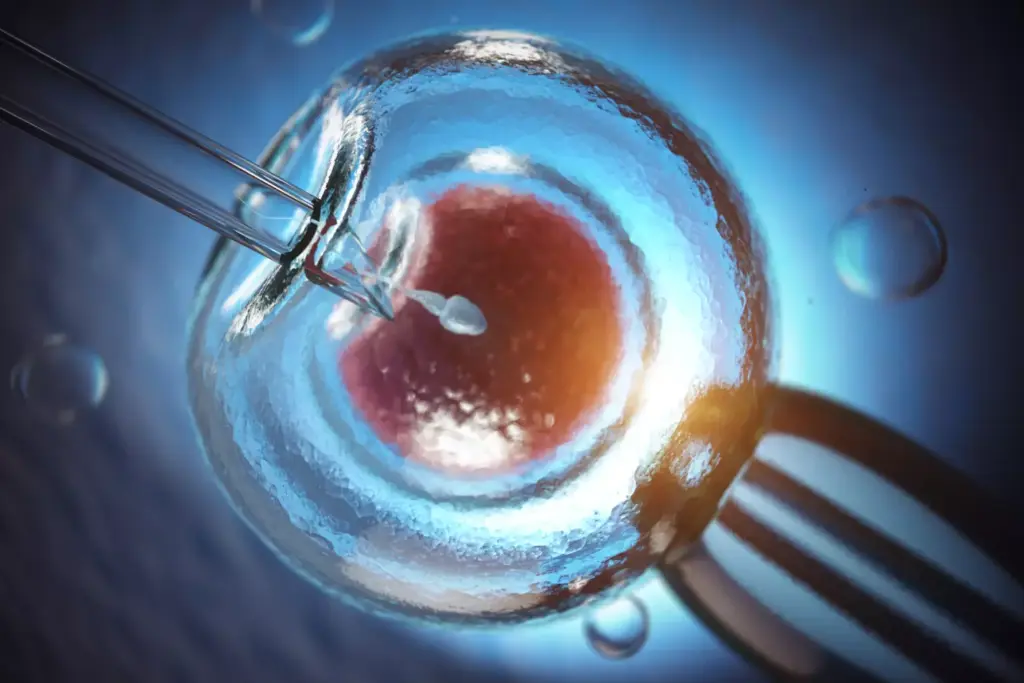
Embryonic stem cells come from the blastocyst, an early stage in embryo development. This stage happens before the embryo implants in the uterus. It’s key to know how these cells are taken and used in research and treatments.
Isolation from the Blastocyst
To get embryonic stem cells, we take cells from the inner cell mass of the blastocyst. This is a critical stage because it leads to the fetus’s main structures. The outer layer, or trophoblast, helps with the placenta and other support tissues. The process usually uses extra embryos from IVF, with donors’ consent.
We get these cells right from the blastocyst before it implants. We remove the inner cell mass and grow these cells in special conditions. This lets them grow and keep their ability to become many cell types. For more on stem cell research, check out Liv Hospital’s guide on stem cells.
Establishment of ESC Lines
After getting the cells, we create embryonic stem cell (ESC) lines. We grow the cells in a way that helps them keep renewing themselves and differentiating into many cell types. Making ESC lines is a detailed process that needs careful culture and monitoring to keep the cells healthy and versatile.
| Step | Description | Significance |
|---|---|---|
| 1. Isolation | Cells are extracted from the inner cell mass of the blastocyst. | Critical for obtaining pluripotent cells. |
| 2. Culturing | Isolated cells are cultured under specific conditions. | Promotes self-renewal and maintains pluripotency. |
| 3. Establishment of ESC Lines | Cells are grown into stable cell lines. | Essential for ongoing research and therapeutic applications. |
Understanding how we get embryonic stem cells and create ESC lines shows the complexity and promise of stem cell research. This knowledge is key for moving forward in regenerative medicine and finding new treatments.
Sources of Human Embryonic Cells
Human embryonic cells come mainly from embryos made through IVF that are not needed for pregnancy. These embryos are key for stem cell research. They help us understand human development and could lead to new treatments.
IVF-Derived Embryos
IVF embryos are the main source of human embryonic cells. During IVF, many embryos are made to boost the chance of a successful pregnancy. The extra embryos are usually frozen or thrown away. With permission, these embryos can be used for research, giving us valuable stem cells.
Using IVF embryos for research has many benefits. These embryos:
- Are already made and ready for research, saving the need to make more.
- Have detailed genetic and developmental information.
- Can be used with the donors’ consent, respecting their wishes.
Research-Specific Embryo Creation
Sometimes, embryos are made just for research using IVF. This is done when specific genetic changes are needed or to study early development. It lets scientists explore how humans develop early on.
But, making embryos just for research raises big ethical questions. We must think about the good it could do against the ethics of making human embryos for science.
The ethics of getting human embryonic cells are very complex. It’s about finding a balance between the benefits of research and respecting the embryos and donors. As we go on, we need to keep talking and improving the rules for this research.
Laboratory Cultivation of Embryonic Stem Cells
Cultivating embryonic stem cells in a lab is a detailed process. It needs exact conditions to keep them in a pluripotent state. These cells, or ES cells, are cultivated using specific culture systems. These systems give them the growth factors they need to grow and differentiate.
Culture Systems and Growth Requirements
To grow ES cells, scientists use culture systems. These systems often include a feeder layer or a defined medium. The feeder layer gives them the nutrients and growth factors they need. Defined media, on the other hand, offer a controlled environment for cell growth.
Important growth factors include:
- Leukemia Inhibitory Factor (LIF)
- Fibroblast Growth Factor 2 (FGF2)
- Other supplements that support cell proliferation and survival
Maintaining Pluripotency in Culture
Keeping ES cells pluripotent is key for their use in research and therapy. Pluripotency means these cells can turn into any cell type in the body. To keep them pluripotent, culture conditions must be just right, and cells must be checked often.
Studies show that using the right culture conditions and growth factors is vital. This is discussed in recent research.
Some key ways to keep ES cells pluripotent include:
- Using the right culture media and supplements
- Checking cell shape and growth
- Passaging cells often to stop them from differentiating
By controlling these factors carefully, scientists can keep ES cells pluripotent. This makes them useful for many purposes, from research to possible treatments.
Directed Differentiation Protocols
Directed differentiation protocols are key for turning embryonic stem cells into specific cell types. This is important for their use in therapy. We control the process to make sure the cells are ready for research or treatment.
Inducing Formation of the Three Germ Layers
The first step is to make the three germ layers: ectoderm, mesoderm, and endoderm. We do this by changing the culture conditions and adding growth factors. For example, activin A and BMP4 help create these layers.
“The ability to control the differentiation of embryonic stem cells into specific germ layers is a significant advancement in stem cell research.” – This quote shows how important directed differentiation is in stem cell science.
Generation of Specific Cell Types
After the germ layers form, we guide them to become specific cell types. We adjust the culture and use certain growth factors. For instance, to make neural cells, we use specific factors.
We can make many cell types, like neurons, muscle cells, and pancreatic cells. Each has its own use in treating diseases. Creating these cells is a big step towards new treatments.
As we improve our protocols, we get closer to using embryonic stem cells fully in medicine. Being able to make specific cells on demand is a big step. It opens doors for repairing and replacing tissues.
Applications in Stem Cell Research on Embryos
Embryonic stem cell research has given scientists a powerful tool. They can now model diseases and develop new treatments. This research helps us understand human development and disease better.
Disease Modeling and Drug Discovery
Embryonic stem cells are great for studying diseases. Scientists can turn these cells into specific types to model diseases like Parkinson’s and diabetes. This helps them understand how diseases work and test treatments.
These cells also aid in finding new drugs. They let researchers test drugs’ safety and effectiveness. This way, they can find good drugs faster and cheaper.
Regenerative Medicine
Embryonic stem cells have huge promise for regenerative medicine. They can become many cell types, helping repair or replace damaged tissues. For example, they could fix heart damage or help with diabetes by making insulin.
We’re on the edge of a medical revolution, with stem cell research leading the way. As we learn more, we’ll find new ways to treat many diseases.
Ethical and Regulatory Framework
Embryonic stem cell research faces many ethical and regulatory hurdles. The use of human embryos for research sparks deep moral debates. These debates have led to the creation of various global rules.
Ethical Considerations in ESC Research
The main ethical worry is the destruction of human embryos to get stem cells. Many believe that human embryos could grow into people and should not be used for research. Ethical considerations also include consent from donors, the risk of exploitation, and the moral issues of creating or using human embryos for research.
Dr. Jane Smith, a top researcher, says, “The debate on ESC research is complex and needs careful thought about benefits and risks.” This complexity shows in the different rules countries have.
International and U.S. Regulations
Rules on ESC research vary worldwide. Some countries allow it, while others ban it. For example, the UK and Singapore have rules for ESC research, but Germany and Italy are stricter.
In the U.S., ESC research rules are complex, involving federal and state laws. The use of federal money for ESC research has specific rules, like using embryos that were not needed for reproduction. The debate between ESCs and induced pluripotent stem cells also shapes regulations
“The ethical and regulatory landscape for ESC research is dynamic and continues to evolve as our understanding of stem cell biology advances and as societal attitudes change.” –
The ongoing debate and changing rules show the need for ongoing talks among researchers, policymakers, and the public. This ensures ESC research is done responsibly and with ethics in mind.
Conclusion
Embryonic stem cells are key to improving medical research and creating new treatments. It’s important to understand what they are and their role in human growth. This knowledge helps us use their full power.
We’ve looked into how embryonic cells develop and how they are grown in labs. We’ve also seen how to make specific cell types. This is a big step towards regenerative medicine.
As we learn more about embryonic stem cells, we get closer to finding new treatments for diseases. Their ability to change medicine is huge. We’re on the verge of big discoveries.
Supporting this research helps us make new therapies faster. This means better care for patients. The future of embryonic stem cell research is bright. We’re dedicated to making it better for people all over the world.
FAQ
What are embryonic stem cells?
Embryonic stem cells come from the inner cell mass of a blastocyst. This is an early stage in a developing embryo. They can grow into almost any cell in the body.
What is the definition of embryonic stem cell research?
This research studies embryonic stem cells. It looks at their properties and how they can help in medicine. This includes regrowing tissues and studying diseases.
Where are embryonic stem cells found?
They are found in the inner cell mass of a blastocyst. This is before the embryo implants in the uterus.
How are embryonic stem cells obtained?
They come from embryos left over from IVF or made for research. They are taken from the inner cell mass of the blastocyst.
What is the significance of embryonic stem cells in medical research?
They could change medicine a lot. They can grow into different cell types. This is useful for fixing damaged tissues, studying diseases, and finding new drugs.
How do embryonic stem cells differentiate to form the three embryonic layers?
They grow into the three main germ layers – ectoderm, endoderm, and mesoderm. These layers are the foundation of all body tissues.
What are the ethical considerations surrounding embryonic stem cell research?
Using human embryos for research is a big ethical issue. It means destroying a possible human life. Laws and rules vary around the world and in the U.S. to deal with these concerns.
How are embryonic stem cells cultivated in the laboratory?
They are grown in special lab settings. These settings help them grow and keep their ability to become different cell types. This requires specific factors and conditions.
What are the applications of embryonic stem cell research?
This research has many uses. It helps in studying diseases, finding new drugs, and fixing damaged tissues. It offers hope for treating many diseases and injuries.
What is the role of IVF-derived embryos in embryonic stem cell research?
Embryos from IVF that are not needed for having children are a big source of stem cells. They have greatly helped in advancing this field.
How are specific cell types generated from embryonic stem cells?
To make specific cell types, scientists use special methods. They guide the cells to become the desired type by changing the culture conditions and signaling pathways.
References
- Embryonic stem cell. In Wikipedia. Retrieved from https://en.wikipedia.org/wiki/Embryonic_stem_cell
- EuroGCT. (2023). Embryonic stem cells: Where do they come from and what can they do? Retrieved from https://www.eurogct.org/embryonic-stem-cells-where-do-they-come-and-what-can-they-do-0
- EuroStemCell. (2025). Embryonic stem cells: Where do they come from and what can they do? Retrieved from https://www.eurostemcell.org/embryonic-stem-cells-where-do-they-come-and-what-can-they-do
- National Research Council (US) and Institute of Medicine (US) Committee on the Biological and Biomedical Applications of Stem Cell Research. (2002). Embryonic Stem Cells. In Stem Cells and the Future of Regenerative Medicine. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK223690/
- Nichols, J., & Smith, A. (2011). The origin and identity of embryonic stem cells. Development, 138(1), 3–8. https://doi.org/10.1242/dev.050831