Last Updated on October 21, 2025 by mcelik
Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. This often leads to bone marrow failure. A big worry for patients is turning into a more serious disease, like acute myeloid leukemia (AML).
MDS makes it hard for the bone marrow to make healthy blood cells. This causes many health problems. It’s important for patients and their families to know what MDS is and how it affects health.
Understanding myelodysplasia means knowing its effect on life expectancy. How long a patient lives with MDS can change a lot. It depends on the type of MDS and the patient’s health.
Key Takeaways
- MDS is a group of disorders that affect blood cell production in the bone marrow.
- The condition can lead to severe health complications, including acute myeloid leukemia (AML).
- Understanding MDS is key for patients to manage their condition well.
- Life expectancy in MDS patients varies based on the subtype and overall health.
- Early diagnosis and proper treatment can greatly improve patient outcomes.
Understanding Myelodysplastic Syndrome (MDS)
Myelodysplastic Syndrome (MDS) is a blood disorder where the bone marrow can’t make enough healthy blood cells. This leads to problems like anemia, infections, and bleeding issues.
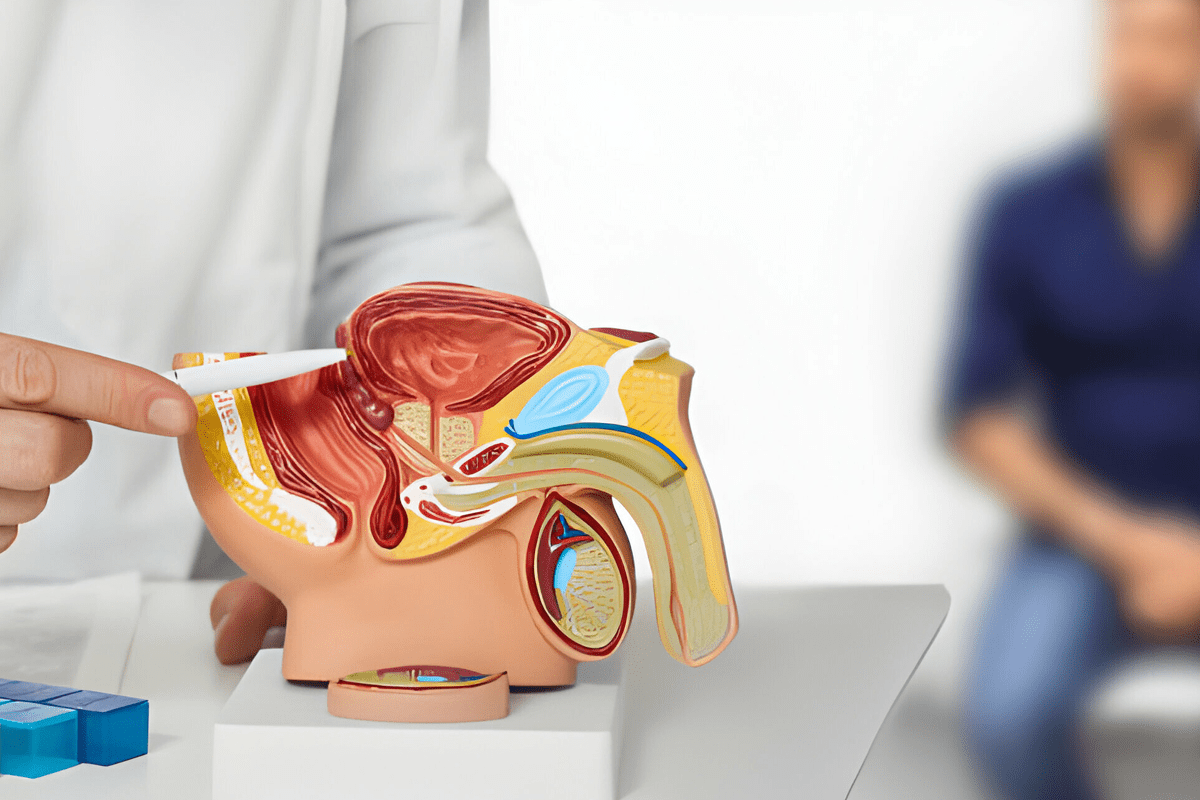
Definition and Basic Pathophysiology
MDS mainly affects older people, messing with the bone marrow’s blood cell production. It’s caused by a mix of genetic and environmental factors.
In MDS, the bone marrow has abnormal cells that don’t mature right. This results in a lack of healthy red and white blood cells and platelets. It can even turn into Acute Myeloid Leukemia (AML).
Prevalence and Demographics
MDS is not very common, but it gets more common with age. Studies show most cases are in people over 60.
| Age Group | Incidence Rate |
| Less than 60 | Low |
| 60-70 | Moderate |
| Greater than 70 | High |
Knowing who gets MDS and how often is key to catching it early. It’s important for improving the lives of those affected.
Types and Classification of MDS
It’s important to know the different types and classifications of MDS. This helps figure out the prognosis and treatment options. Myelodysplastic Syndromes (MDS) are disorders where the body can’t make blood cells well. This leads to low counts of different blood cells.
The way we classify MDS has changed over time. Now, we use systems based on how cells look, their genetic makeup, and how the disease acts.
WHO Classification System
The World Health Organization (WHO) system is a key way to sort MDS. It looks at how many blood cell types are affected, if there are ring sideroblasts, and the number of blasts in the blood and bone marrow. This system helps tell MDS apart from other blood cancers like Acute Myeloid Leukemia (AML). It also gives clues about how likely the disease is to progress.
The WHO system has been updated to include new information about genes and chromosomes. These updates make diagnosing MDS more accurate and help predict how the disease will behave.

IPSS and IPSS-R Risk Stratification
The International Prognostic Scoring System (IPSS) and its updated version (IPSS-R) are also key for figuring out MDS risk. The IPSS looks at the number of bone marrow blasts, the type of chromosomes, and how many blood cell types are low. The IPSS-R adds more details about chromosomes and changes how it counts blasts.
Both systems are important for predicting how MDS will progress. Patients at high-risk are more likely to turn into AML. They might need stronger treatments, like a bone marrow transplant.
Knowing the mds stages and risk levels is key for doctors to plan the best treatment for each patient. This approach can lead to better outcomes for people with MDS.
Myelodysplasia Disease Life Expectancy: Key Factors
MDS life expectancy depends on many factors. These include the disease itself and the patient’s health. Knowing these factors helps both patients and doctors make better choices about treatment.
Impact of MDS Subtype on Survival
The type of MDS a patient has greatly affects their survival chances. The World Health Organization (WHO) classifies MDS into different types. Patients with lower-risk MDS tend to live longer than those with higher-risk types.
A study in the Journal of Clinical Oncology found that lower-risk MDS patients can live several years to over a decade. This depends on their health and how well they respond to treatment. On the other hand, higher-risk MDS patients face a faster disease progression. They may live shorter lives unless they get aggressive treatments like stem cell transplants.
Role of Age and Comorbidities
Age and other health issues also affect MDS patients’ life expectancy. Many MDS patients are older and have other health problems. These conditions can make treatment harder and shorten life expectancy.
“The interplay between MDS and comorbidities is complex, and managing these conditions is critical for improving patient outcomes.”
Hematologist
It’s important to look at a patient’s overall health when planning treatment. This includes their age and any other health problems. This approach helps find the best treatment balance. It aims to improve both the quality of life and survival for MDS patients.
Is MDS Considered a Terminal Illness?
Deciding if MDS is a terminal illness is complex. It depends on many factors. Myelodysplastic Syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells, leading to bone marrow failure.
Defining Terminal Conditions in Hematology
In hematology, a terminal condition means no cure or significant improvement with current treatments. For MDS, this can be tricky. It’s because the disease’s severity and how well patients respond to treatment vary a lot.
MDS is considered a serious condition because it can turn into more severe diseases like Acute Myeloid Leukemia (AML). The chance of turning into AML is a key factor in determining how well a patient will do. It’s something doctors watch closely.
Variability in MDS Outcomes
How well MDS patients do can vary a lot. Some with lower-risk MDS can live for many years. But, those with higher-risk disease might have a shorter life expectancy.
The International Prognostic Scoring System (IPSS) and its revised version (IPSS-R) help predict patient outcomes. They look at things like cytogenetic abnormalities, blast percentage, and the number of cytopenias.
- Lower-risk MDS patients often get supportive care and may have a stable disease course.
- Higher-risk patients might get more aggressive treatments, like stem cell transplantation.
It’s important to understand a patient’s MDS well. This helps figure out their prognosis and what treatment to choose.
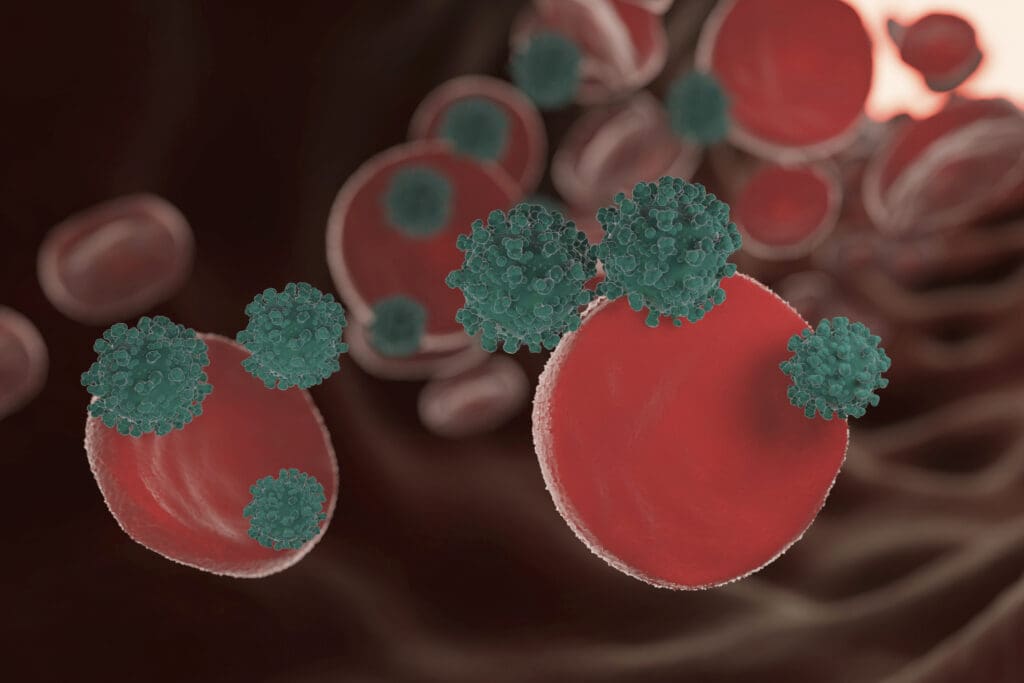
The Relationship Between MDS and Acute Myeloid Leukemia
MDS and AML are closely linked, with MDS often turning into AML. This change is a big worry for both patients and doctors. It affects how we treat the disease and how well patients do.
Progression from MDS to AML
The shift from MDS to AML happens when cancer cells get more aggressive. This is due to genetic changes that help these cells survive longer. Eventually, MDS can turn into AML, a more serious leukemia.
Key factors influencing this progression include:
- Genetic instability
- Epigenetic alterations
- Clonal evolution
Knowing these factors helps us spot who’s at risk. It also guides us in finding better treatments.
Risk Factors for Transformation
There are several things that make MDS more likely to turn into AML. These include:
- Cytogenetic abnormalities, like complex karyotypes or specific deletions
- High-risk MDS subtypes based on the IPSS-R classification
- Certain molecular mutations, like in the TP53 or RUNX1 genes
Spotting these risk factors helps doctors keep a closer eye on patients. It might even help stop the disease from getting worse.
The connection between MDS and AML shows we need more research. By understanding how the disease progresses, we can find better ways to manage MDS. This could help prevent it from turning into AML.
MDS Stages and Disease Progression
MDS progression varies among patients. It’s key to know the different stages. Myelodysplastic Syndrome (MDS) is a group of disorders with ineffective blood cell production. It can lead to complications like acute myeloid leukemia (AML).
Low-Risk vs. High-Risk MDS
Classifying MDS into low-risk and high-risk categories is important. Low-risk MDS has a better prognosis, with slower disease progression. On the other hand, high-risk MDS has a worse prognosis and a higher chance of turning into AML.
“The International Prognostic Scoring System (IPSS) and its revised version (IPSS-R) are widely used,” says a hematologist. “They consider factors like cytogenetic abnormalities, blast percentage, and cytopenias.”
Monitoring Disease Evolution
Regular monitoring of MDS is key to track disease progression and adjust treatment plans. This includes blood counts, bone marrow biopsies, and cytogenetic analysis. Early detection of disease progression leads to better outcomes.
- Regular follow-up appointments with a hematologist
- Periodic blood tests and bone marrow examinations
- Cytogenetic and molecular testing to monitor genetic changes
Understanding MDS stages and monitoring disease progression are vital. Recognizing low-risk and high-risk MDS helps tailor treatments. This ensures each patient gets the right care.
Common Symptoms of Myelodysplastic Syndrome in Adults
The symptoms of MDS in adults can vary a lot. This depends on the disease’s specifics and the person’s health. Knowing these symptoms is key for early detection and managing the condition well.
Initial Presentation and Early Symptoms
In the early stages, MDS can be tricky to diagnose. This is because its symptoms are similar to those of other conditions. Common early signs include:
- Fatigue and weakness due to anemia
- Shortness of breath
- Pale skin
- Increased risk of infections
- Easy bruising or bleeding
These symptoms happen because MDS messes with the bone marrow’s ability to make healthy blood cells. Anemia, or low red blood cell count, is a common early sign. It leads to feeling tired and weak.
Advanced Disease Manifestations
As MDS gets worse, symptoms can get more serious. These may include:
- Severe infections due to low white blood cell counts
- Frequent or severe bleeding due to low platelet counts
- Increased fatigue and weakness
- Weight loss
In advanced stages, MDS can turn into Acute Myeloid Leukemia (AML), a more aggressive blood cancer. It’s important to manage symptoms to improve quality of life.
| Symptom | Early Stage | Advanced Stage |
| Fatigue | Mild to moderate | Severe |
| Infections | Occasional | Frequent and severe |
| Bleeding | Easy bruising | Frequent or severe bleeding |
A hematologist, says, “Understanding how MDS symptoms progress is vital for good care and better patient outcomes.”
“The variability in MDS symptoms highlights the need for personalized treatment plans. These plans should meet the unique needs of each patient.”
Diagnostic Approaches for MDS
Diagnosing Myelodysplastic Syndrome (MDS) requires a mix of clinical checks and lab tests. Getting the diagnosis right is key to picking the right treatment and knowing what to expect.
Blood Tests and Bone Marrow Evaluation
The first step is blood tests to check the levels of red, white blood cells, and platelets. A Complete Blood Count (CBC) is a must. It shows if there are any oddities in blood cell counts, which might point to MDS.
Then, a bone marrow biopsy and aspiration are done. These tests look at the bone marrow’s cells and find any oddities. They help figure out how bad the dysplasia is and the number of blasts, which are key for MDS diagnosis and its type.
Cytogenetic and Molecular Testing
Cytogenetic analysis looks at bone marrow cells’ chromosomes for genetic issues. This is important for figuring out the risk and what to expect. Common problems include deletions of chromosomes 5 and 7, and trisomy 8.
Molecular testing, like Next-Generation Sequencing (NGS), finds specific gene mutations linked to MDS. Mutations in TP53, RUNX1, and ASXL1 genes are seen in MDS and can affect the disease’s outlook.
By using blood tests, bone marrow checks, cytogenetic analysis, and molecular testing, doctors can accurately diagnose MDS. They can also figure out its subtype and risk level. This detailed approach is vital for creating a treatment plan that fits the patient’s needs.
Treatment Options for Different MDS Risk Categories
The treatment for Myelodysplastic Syndrome (MDS) varies based on the disease’s risk level. Knowing the risk category is key to finding the best treatment. This helps improve patient outcomes.
Low-Risk MDS Management
For those with low-risk MDS, the main goal is to manage symptoms and enhance quality of life. Treatment options include:
- Supportive Care: This involves blood transfusions to help with anemia and platelet transfusions to prevent bleeding.
- Growth Factors: Medications like erythropoietin and G-CSF help produce more blood cells.
- Immunosuppressive Therapy: Some patients benefit from drugs like ATG and cyclosporine.
- Lenalidomide: This drug is very effective for patients with low-risk MDS and a specific chromosomal deletion.
Regular monitoring is key to adjust treatment plans as needed. It helps identify any progression to a higher risk category quickly.
High-Risk MDS Treatment Approaches
Patients with high-risk MDS need aggressive treatments to change the disease’s course. Treatment options include:
- Hypomethylating Agents: Drugs like azacitidine and decitabine can improve survival by reducing abnormal cell production.
- Intensive Chemotherapy: This is similar to AML treatment and may be considered for some high-risk MDS patients.
- Hematopoietic Stem Cell Transplantation: This is the only potentially curative treatment, but it’s a complex procedure with significant risks.
For patients with progressive MDS, treatment plans must adapt to the disease’s changes. This may involve more intensive therapies or clinical trials for new treatments.
The choice of treatment for MDS depends on several factors. These include the patient’s health, the disease’s characteristics, and personal preferences. A healthcare team specializing in MDS can guide on the best treatment strategy.
Stem Cell Transplantation for MDS
Stem cell transplantation is a treatment that can cure myelodysplastic syndrome (MDS). It replaces the patient’s sick bone marrow with healthy stem cells. These can come from the patient themselves or a donor.
Choosing to have a stem cell transplant depends on many things. These include the patient’s health, the type of MDS, and the disease’s risk level.
Candidacy and Timing Considerations
Not every MDS patient can get a stem cell transplant. Being a candidate depends on age, health, and if a donor is available. When to do the transplant is also key. It must balance the risk of the disease getting worse with the chance of the transplant working.
For those with high-risk MDS, transplanting sooner is often better. This is because these patients might get the most benefit from the transplant’s curative effects.
Outcomes and Survival Rates
The success of stem cell transplantation for MDS varies. It depends on the patient’s health before the transplant, the donor match, and the treatment used.
Thanks to better transplant methods and care, survival rates have gone up. Many MDS patients who get a transplant can live long-term and even be cured.
But, the transplant comes with risks. Problems like graft-versus-host disease (GVHD) can harm the patient’s life quality and survival chances.
What Is the Most Common Cause of Death in MDS?
Myelodysplastic Syndrome (MDS) makes it hard for the body to make blood cells. This can lead to serious problems that can be deadly. Knowing what causes death in MDS patients is key to helping them live better lives.
Complications of Cytopenias
One big reason MDS patients die is because of problems caused by not having enough blood cells. These problems include:
- Anemia makes people very tired and can’t get enough oxygen
- Neutropenia makes it hard to fight off infections
- Thrombocytopenia can cause serious bleeding
These issues can really hurt a patient’s quality of life and make them more likely to face serious dangers.
Leukemic Transformation and Other Factors
Another big reason MDS patients die is when their disease turns into Acute Myeloid Leukemia (AML). How likely this is can depend on the type of MDS and other factors.
Important things that can affect the chance of turning into AML include:
- Genetic changes in the cells
- How bad the lack of blood cells is
- Having certain genetic mutations
Knowing about these factors is important for treating MDS well. It can help prevent or slow down the change to AML.
Living with MDS: Quality of Life and Support Resources
Living with myelodysplastic syndrome (MDS) is tough. It affects both your body and mind. You face many challenges, like symptoms, treatments, and changes in your lifestyle.
Managing Physical and Emotional Challenges
MDS brings physical symptoms like fatigue, infections, and bleeding. These can really lower your quality of life. To deal with these, you need a mix of medical care, lifestyle changes, and emotional support.
Physical Challenges: Fatigue, weakness, and shortness of breath are common. Blood transfusions and medicines can help.
Emotional Support: MDS also takes a toll on your mind. You might feel anxious, depressed, or worried about the future. Counseling, support groups, and talking to others with MDS can help.
| Support Resource | Description | Benefits |
| Patient Organizations | Groups that provide information, advocacy, and community for MDS patients. | Access to educational materials, support networks, and advocacy efforts. |
| Educational Materials | Resources such as brochures, websites, and webinars that educate patients about MDS. | Empowers patients with knowledge about their condition, treatment options, and management strategies. |
| Support Groups | Face-to-face or online groups where patients can share experiences and support one another. | Provides emotional support, reduces feelings of isolation, and offers practical advice from peers. |
Patient Organizations and Educational Materials
Many organizations help MDS patients. They offer lots of information and support. These groups provide educational materials, host support groups, and advocate for patients.
The MDS Foundation is a great example. They offer resources, advocacy, and support for research into MDS.
By using these resources, MDS patients can manage their condition better. They can improve their quality of life and find support on their journey.
Conclusion: Navigating an MDS Diagnosis
Getting a Myelodysplastic Syndrome (MDS) diagnosis can be tough. It’s because MDS is complex and can have different outcomes. Knowing if MDS is terminal and understanding its stages is key for making care choices.
MDS can get worse and turn into acute myeloid leukemia. This raises questions about life expectancy. It’s important for patients to work with their doctors to keep an eye on their health and change treatment plans as needed.
Understanding MDS, its progression, and treatment options can help patients manage their condition better. They can also improve their quality of life. Getting support from patient groups and learning more about MDS can help with the physical and emotional challenges of the disease.
FAQ
What is myelodysplastic syndrome (MDS)?
Myelodysplastic syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This often leads to bone marrow failure.
Is myelodysplastic syndrome a terminal illness?
MDS is a serious and potentially life-threatening condition. Whether it’s terminal depends on several factors. These include the subtype, age, and overall health of the patient.
What are the different types of MDS?
The World Health Organization (WHO) classifies MDS into several subtypes. These are based on blast percentage, cytogenetics, and morphology.
How does MDS progress to acute myeloid leukemia (AML)?
MDS can turn into AML, a more aggressive blood cancer. The risk of this happening varies. It depends on the MDS subtype and cytogenetic abnormalities.
What are the common symptoms of MDS in adults?
Adults with MDS often experience fatigue, weakness, and shortness of breath. They may also have infections and signs of bleeding or bruising due to low blood counts.
How is MDS diagnosed?
Diagnosing MDS involves blood tests, bone marrow evaluation, and cytogenetic and molecular testing. These tests help assess the disorder’s presence and characteristics.
What are the treatment options for MDS?
Treatment for MDS depends on the risk category. It may include supportive care, immunotherapy, chemotherapy, and stem cell transplantation. The goal is to manage symptoms and improve survival.
What is the role of stem cell transplantation in MDS treatment?
Stem cell transplantation is a potentially curative treatment for MDS. It’s most beneficial for patients with high-risk disease. But, it comes with significant risks and requires careful consideration.
What is the most common cause of death in MDS patients?
The most common causes of death in MDS patients are complications from cytopenias. These include infections and bleeding. Leukemic transformation to AML is also a major cause.
How does MDS impact quality of life?
MDS can significantly affect quality of life. Symptoms, treatment side effects, and the psychological burden of living with a chronic condition all play a role.
What support resources are available for MDS patients?
MDS patients can find various support resources. These include patient organizations, educational materials, and healthcare providers. They help manage the condition and improve quality of life.
What is myelodysplastic syndrome life expectancy?
Life expectancy in MDS varies widely. It depends on factors like the subtype, age, and overall health. Some patients have a relatively indolent course, while others face a more aggressive disease.
What is the difference between low-risk and high-risk MDS?
Low-risk MDS has a lower risk of leukemic transformation and longer survival. High-risk MDS, on the other hand, has a higher risk of AML transformation and shorter survival.
How is MDS staged?
MDS is staged using risk stratification systems like the International Prognostic Scoring System (IPSS) and the Revised IPSS (IPSS-R). These systems help predict prognosis and guide treatment decisions.