For those with serious blood disorders, knowing the difference between bone marrow transplant and stem cell transplant can be very important. At Liv Hospital, we focus on patient care and evidence-based treatments. We aim to help you understand the key differences and facts you need to know.
Both procedures aim to replace damaged marrow with healthy stem cells. This helps restore blood and immune cell production. A stem cell transplant is a key treatment for cancers like leukemia, lymphoma, and multiple myeloma.
We will look at five key facts that show the differences and similarities between these procedures. This will give you a full understanding of what to expect.
Key Takeaways
- Understanding the source and method of collecting donor cells is key.
- Both bone marrow and stem cell transplants aim to restore blood and immune function.
- Stem cell transplants are used to treat certain types of cancers.
- The procedures involve replacing damaged marrow with healthy stem cells.
- Liv Hospital provides complete care for international patients.
The Science Behind Blood-Forming Stem Cells
Hematopoietic stem cells are at the core of transplantation medicine. They can turn into different blood cells. This makes them key for making red blood cells, white blood cells, and platelets. These cells are vital for patients getting transplants to restore their blood and immune systems.
What Are Hematopoietic Stem Cells?
Hematopoietic stem cells can become all types of blood cells. They can keep themselves going and grow into cells that become red blood cells, white blood cells, and platelets. This is important for keeping the body’s blood and immune systems working right.
Key characteristics of hematopoietic stem cells include:
- Self-renewal: The ability to maintain their numbers.
- Differentiation: The capacity to develop into various blood cell types.
How These Cells Restore Blood and Immune Function
When a patient gets a stem cell or bone marrow transplant, the goal is to replace their damaged or diseased blood and immune system with healthy cells. Hematopoietic stem cells are key in this process. They help repopulate the patient’s bone marrow and get it working again.
The process involves several steps:
- The patient’s existing bone marrow is suppressed or destroyed.
- Hematopoietic stem cells are infused into the patient.
- These stem cells migrate to the bone marrow, where they begin to produce new blood cells.
| Cell Type | Function |
|---|---|
| Red Blood Cells | Carry oxygen throughout the body |
| White Blood Cells | Play a key role in the immune response |
| Platelets | Essential for blood clotting |
Evolution of Transplantation Medicine
The field of transplantation medicine has made big strides over the years. We’ve learned more about hematopoietic stem cells and their role in transplants. Pioneer, said, “The development of bone marrow transplantation as a treatment for various diseases has been a long and challenging journey, but one that has yielded significant rewards.”
“The development of bone marrow transplantation as a treatment for various diseases has been a long and challenging journey, but one that has yielded significant rewards.”
As research keeps moving forward, we’re seeing new uses for hematopoietic stem cells. This includes new ways to treat blood-related disorders and improve transplant results.
Understanding the Difference Between Bone Marrow Transplant and Stem Cell Transplant
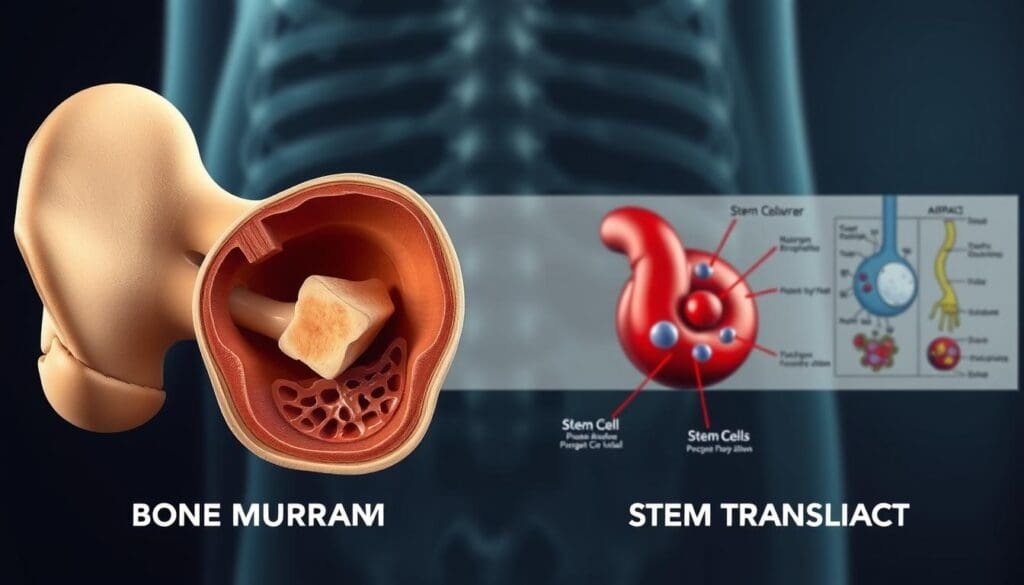
The main difference between bone marrow and stem cell transplants is where the stem cells come from. Both methods use stem cells to replace damaged cells. But, they get these cells in different ways.
Collection Source: Marrow vs. Peripheral Blood
Bone marrow transplants take stem cells directly from the bone marrow, usually from the hips. Stem cell transplants, or peripheral blood stem cell transplants, get stem cells from the blood. These cells are moved from the bone marrow to the blood.
Key differences in collection sources include:
- Bone marrow is extracted through a surgical procedure.
- Peripheral blood stem cells are collected through apheresis, a process that filters the blood to isolate stem cells.
Harvesting Procedures Compared
The ways to get bone marrow and peripheral blood stem cells are different. Bone marrow harvesting is a surgery done under anesthesia. It uses a needle to take marrow from the bone.
Peripheral blood stem cell collection uses medicine to move stem cells into the blood. Then, apheresis is used to get these cells.
The advantages of each method are:
- Bone marrow harvesting allows for a more direct collection of stem cells.
- Peripheral blood stem cell collection is less invasive and often preferred due to its faster recovery time.
Why Terminology Often Causes Confusion
The terms for bone marrow and stem cell transplants can be confusing. Both involve transplanting stem cells. But, they differ in where and how these cells are collected.
Clarifying the terminology:
- Both bone marrow and peripheral blood stem cell transplants are types of stem cell transplants.
- The term “stem cell transplant” is often used broadly to include both bone marrow and peripheral blood stem cell transplants.
Key Fact #1: Collection Methods and Patient Experience
Collecting bone marrow and stem cells for transplant has two main ways. Each method affects the patient’s experience and the transplant’s success. These differences are key to a good transplant outcome.
Bone Marrow Harvest: Surgical Procedure
Bone marrow harvest is a surgery to take marrow from the hip bone. This surgery is done in an operating room and can take hours. The marrow is then processed to get the stem cells needed for transplant.
Peripheral Blood Stem Cell Collection: Apheresis
Peripheral blood stem cell collection uses apheresis. This method takes stem cells from the blood. It’s less invasive than bone marrow harvest and doesn’t need surgery. Donors get medicine to help release stem cells before the apheresis.
“Apheresis has revolutionized the way we collect stem cells, making the process safer and less invasive for donors.”
Impact on Donor Recovery Time
Donor recovery times vary between methods. Bone marrow harvest, being a surgery, takes longer to recover from, often weeks. Peripheral blood stem cell collection through apheresis lets donors recover faster, usually in days.
| Collection Method | Recovery Time | Invasiveness |
|---|---|---|
| Bone Marrow Harvest | Several weeks | Surgical |
| Peripheral Blood Stem Cell Collection | A few days | Less invasive |
Knowing these differences helps donors and healthcare providers choose the best method. It depends on individual needs and situations.
Key Fact #2: Types of Transplants and Their Applications
Stem cell transplants are mainly divided into two types: autologous and allogeneic. Each has its own use. Knowing the difference is key for both patients and doctors to choose the right treatment.
Autologous Transplants: Using Your Own Cells
Autologous transplants use your own stem cells. First, stem cells are taken from you, often from bone marrow or blood. Then, they are stored until needed.
Next, you get treatment to clear out sick cells. After that, your stored stem cells are put back to fill your bone marrow.
Benefits of Autologous Transplants:
- No risk of graft-versus-host disease (GVHD)
- Faster engraftment and recovery
- Lower risk of complications related to donor cell compatibility
Allogeneic Transplants: Using Donor Cells
Allogeneic transplants use cells from a donor. The donor can be a relative or someone else. The match is checked through HLA typing.
This transplant is good for genetic disorders or some blood cancers.
Benefits and Considerations of Allogeneic Transplants:
- Potential graft-versus-tumor effect, beneficial in fighting cancer
- Requires careful HLA matching to minimize GVHD risk
- Immune system reconstitution may take longer
To show the differences and uses of these transplants, let’s look at a table:
| Characteristics | Autologous Transplants | Allogeneic Transplants |
|---|---|---|
| Source of Stem Cells | Patient’s own cells | Donor cells (related or unrelated) |
| GVHD Risk | No risk | Present, depends on HLA match |
| Graft-versus-Tumor Effect | Not applicable | Beneficial in certain cancers |
| Engraftment Speed | Faster | Variable, may be slower |
| Typical Use Cases | Multiple myeloma, certain lymphomas | Leukemia, bone marrow failure syndromes |
In conclusion, choosing between autologous and allogeneic transplants depends on many factors. These include the patient’s condition, age, and health. Understanding these differences helps patients make better choices about their treatment.
Key Fact #3: Conditions Treated with Each Procedure
Bone marrow and stem cell transplants are key treatments for many blood and immune system diseases. They have greatly improved the care of serious illnesses, giving hope to people all over the world.
Blood Cancers (Leukemia, Lymphoma, Multiple Myeloma)
Blood cancers like leukemia, lymphoma, and multiple myeloma are often treated with these transplants. Leukemia makes too many bad white blood cells. Lymphoma harms the lymphatic system. Multiple myeloma affects plasma cells in the bone marrow.
Choosing between bone marrow and stem cell transplant depends on the cancer type, its stage, and the patient’s health.
Bone Marrow Failure Syndromes
Conditions like aplastic anemia, where the bone marrow can’t make enough blood cells, are treated with stem cell transplantation. This replaces the damaged bone marrow with healthy stem cells.
Immune Deficiency Disorders
Immune disorders like severe combined immunodeficiency (SCID) can be treated with these transplants. They help the immune system work better, helping patients fight off infections.
Procedure Selection Based on Disease Type
The choice between bone marrow and stem cell transplant depends on the disease. For example, leukemia and lymphoma might use either, based on the disease and patient’s health. Some immune deficiencies need a specific transplant type.
Here’s a table showing the diseases treated and the transplant choice:
| Disease/Condition | Typical Transplant Procedure | Key Considerations |
|---|---|---|
| Leukemia | Bone Marrow or Stem Cell | Disease stage, patient health |
| Lymphoma | Bone Marrow or Stem Cell | Type of lymphoma, disease stage |
| Multiple Myeloma | Stem Cell | Patient response to initial treatment |
| Aplastic Anemia | Stem Cell | Donor availability, patient health |
| SCID (Severe Combined Immunodeficiency) | Bone Marrow or Stem Cell | Donor match, patient condition |
It’s important for patients and doctors to know about these treatments. This helps make the best choices for care.
Key Fact #4: Comparing Recovery and Outcomes
When we look at bone marrow and stem cell transplants, we see big differences. These differences help us choose the best treatment. We’ll talk about how each transplant affects recovery, like how long it takes for new cells to grow, how the immune system comes back, and how well patients do in the long run.
Engraftment Timeline Differences
The time it takes for new cells to start working is different for each transplant. Stem cell transplants usually work faster, in about 2-3 weeks. Bone marrow transplants take a bit longer, around 3-4 weeks.
This difference comes from where the stem cells come from and how they’re prepared. Knowing this helps doctors plan better care for patients after the transplant.
Immune System Reconstitution
Getting the immune system back to normal is key after a transplant. How fast and well this happens affects how well a patient can fight off infections and heal.
Stem cell transplants often lead to a quicker recovery of the immune system because they have more mature immune cells. But, both types need careful watching to avoid problems.
Long-term Survival Rates
How long patients live after a transplant is very important. Both bone marrow and stem cell transplants have shown great success in treating diseases. But, how long patients live can depend on many things, like the disease being treated, the patient’s health, and how well the donor’s cells match.
| Transplant Type | 5-Year Survival Rate | 10-Year Survival Rate |
|---|---|---|
| Bone Marrow Transplant | 55-65% | 40-50% |
| Stem Cell Transplant | 60-70% | 45-55% |
Quality of Life Considerations
How well a patient feels after a transplant is very important. Both types of transplants can affect a patient’s life during recovery and even later.
Things that can affect how well a patient feels include graft-versus-host disease, if the disease comes back, and the emotional impact of the transplant. Supportive care and rehabilitation programs help patients get stronger and improve their life after the transplant.
Understanding the differences in recovery and outcomes helps patients and doctors make better choices about treatment.
Key Fact #5: Risks and Complications Specific to Each Procedure
It’s important to know the risks of bone marrow and stem cell transplants. Both can save lives but have their own dangers. These risks need careful attention from both patients and doctors.
Bone Marrow Transplant Risks
Bone marrow transplants have risks like graft-versus-host disease (GVHD). This is when the donor’s immune cells attack the recipient’s body. Other dangers include infections, damage to organs, and the transplant not working.
“The risk of GVHD is a big worry in allogeneic bone marrow transplants,” say experts.
Stem Cell Transplant Complications
Stem cell transplants, like those using peripheral blood stem cells, have their own problems. These include infection risks when the immune system is weak. There’s also a chance of GVHD in allogeneic transplants and disease coming back.
Handling these issues well is key to a successful transplant.
Graft-versus-Host Disease Management
Graft-versus-host disease is a big problem with allogeneic transplants. It can happen with both bone marrow and stem cell transplants. Doctors use medicines to stop GVHD, watch for signs, and help with symptoms.
“Good GVHD management is vital for better results in allogeneic transplant patients,” a study found.
Infection Prevention Strategies
Stopping infections is very important after a transplant. Doctors use prophylactic antibiotics, antiviral meds, and keep patients isolated. They also teach patients to spot infections early and get help fast if they see signs.
Knowing the risks of bone marrow and stem cell transplants helps doctors give better care. This improves patients’ lives and outcomes.
Patient Selection and Preparation Process
The process of choosing patients for bone marrow or stem cell transplants is detailed. It looks at the patient’s medical history and current health. This step is key to see if the patient is a good fit for the transplant.
Pre-Transplant Evaluation
Before the transplant, patients go through a thorough check-up. This check-up looks at their health and the risks of the transplant. It includes a review of their medical history and current health, along with various tests.
Key components of the pre-transplant evaluation include:
- Medical history review
- Physical examination
- Laboratory tests (blood work, etc.)
- Imaging studies (X-rays, CT scans, etc.)
- Cardiac and pulmonary function tests
Conditioning Regimens: Myeloablative vs. Reduced-Intensity
Before the transplant, patients go through conditioning regimens. These regimens prepare the body for the transplant. There are two main types: myeloablative and reduced-intensity conditioning.
| Conditioning Regimen | Description | Patient Profile |
|---|---|---|
| Myeloablative | High-dose chemotherapy and/or radiation to completely eradicate the bone marrow | Younger patients with fewer comorbidities |
| Reduced-Intensity | Lower-dose chemotherapy and/or radiation to suppress the immune system | Older patients or those with comorbidities |
The choice of conditioning regimen depends on the patient’s age, health, and the disease being treated.
Psychological Preparation
Psychological preparation is a big part of the transplant process. Patients and their families often feel stressed and anxious. Our team offers support, including counseling and education, to help them cope.
“The emotional journey of a transplant patient is just as important as their physical preparation,” says one of our transplant specialists. We ensure that patients receive the necessary support to navigate this complex process.
Innovations Advancing Transplantation Medicine
We’re seeing big changes in transplant medicine, thanks to new ideas. Innovations in transplantation medicine are making treatments better and more available. This means more people can get the help they need.
Haploidentical Transplants
Haploidentical transplants use donors who are half-matched to the patient. This has opened up more options for patients. Thanks to better treatments, these transplants are working better than before.
The good things about haploidentical transplants are:
- More donors for patients without a full match
- Quicker transplants for those with fast-moving diseases
- Could fight leukemia better
Cord Blood as an Alternative Source
Cord blood is being used as a new source for stem cells. It’s quick to get, doesn’t need as tight a match, and has less risk of disease. We’re also looking at mixing cord blood with other sources to make transplants even better.
Learn more about other stem cell sources at our page on alternative to stem cell transplant: autologous vs. allogeneic.
Gene Therapy Applications
Gene therapy is changing transplant medicine. It can fix genetic problems at the cell level. This could cure some diseases without needing a transplant. It’s a new area but very promising.
The benefits of gene therapy are:
- Can treat genetic diseases directly
- Less chance of disease from the transplant
- May not need to use strong medicines to prevent rejection
We’re excited about the future of transplant medicine. With new research, we’re getting better at helping patients. The future looks bright for those in need of transplants.
Conclusion: Making Informed Decisions About Transplantation
Understanding the differences between bone marrow and stem cell transplants is key. Patients and families need to think about many things. This includes the type of transplant, how cells are collected, and possible risks.
Bone marrow and stem cell transplants are different in many ways. They vary in where cells come from, how they are collected, and what patients go through. Knowing these differences helps people make better choices in the complex world of transplantation.
C
hoosing between bone marrow and stem cell transplant needs careful thought. It’s important to get advice from doctors. We suggest talking to healthcare professionals about your specific situation. This way, you can find the best transplant option for you.
What is the main difference between a bone marrow transplant and a stem cell transplant?
A bone marrow transplant takes stem cells directly from the bone marrow. This is usually done through surgery. On the other hand, a stem cell transplant collects stem cells from the blood after they’ve been moved from the bone marrow by medicine.
Are bone marrow and stem cell transplants used to treat the same conditions?
Yes, both are used for similar conditions. These include blood cancers like leukemia and lymphoma, and some bone marrow failures. The choice depends on the disease, the patient’s health, and donor availability.
How do the collection methods for bone marrow and stem cell transplants differ?
Bone marrow collection is a surgery to extract marrow from the hip bone. Stem cell collection uses apheresis, where blood is drawn, stem cells are separated, and then returned.
What is the difference between autologous and allogeneic transplants?
An autologous transplant uses the patient’s own stem cells. These are collected, stored, and then reinfused after treatment. An allogeneic transplant uses stem cells from a donor. The choice depends on the disease, donor availability, and treatment needs.
What are the risks associated with bone marrow and stem cell transplants?
Both carry risks like graft-versus-host disease and infections. The risk varies based on the transplant type, patient’s health, and donor-recipient match.
How has transplantation medicine evolved in recent years?
Transplantation medicine has made big strides. Advances include using haploidentical donors and better managing graft-versus-host disease. These have improved patient outcomes.
What is the role of gene therapy in bone marrow and stem cell transplants?
Gene therapy is a new field. It modifies or replaces genes in stem cells to treat diseases. It’s promising for genetic disorders and some blood cancers.
Is bone marrow transplant the same as stem cell transplant?
While both involve stem cells, they’re not the same. Bone marrow transplants use stem cells from bone marrow. Stem cell transplants use those from peripheral blood.
What is the recovery process like after a bone marrow or stem cell transplant?
The recovery includes engraftment and immune system rebuilding. Patients are closely watched for complications. The recovery time varies based on the transplant type and patient health.
How do I choose between a bone marrow transplant and a stem cell transplant?
Choosing between the two should be discussed with a healthcare provider. Consider the disease, patient health, and other factors. Both have benefits and risks that need careful consideration.
References
Cochrane – Bone marrow vs peripheral blood stem cell transplantation
https://www.cochrane.org/CD010189/stem-cells-bone-marrow-or-stem-cells-peripheral-blood-which-better-adults-blood-cancers
Cochrane – High‑dose chemo with autologous bone marrow or stem cell transplant
https://www.cochrane.org/CD003139/high-dose-chemotherapy-and-bone-marrow-or-stem-cell-transplantation-early-poor-prognosis-breast
Cochrane – Mesenchymal stromal cells in graft‑versus‑host disease
https://www.cochrane.org/CD009768/mesenchymal-stromal-cells-treat-or-prevent-graft-versus-host-disease-stem-cell-transplant-recipients
PMC / PubMed – MSC co‑infusion in allogeneic stem cell transplantation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8056684/
Cochrane – Stem cell transplant vs immunosuppressive therapy in aplastic anaemia
https://pubmed.ncbi.nlm.nih.gov/25031191/




































