Last Updated on October 21, 2025 by

We are on the brink of a major breakthrough in diabetes treatment. Recent studies have shown promising results in using new therapies for diabetes management. At Liv Hospital, our teams combine trusted expertise with cutting-edge research. We are leading the way to lasting solutions for type 1 and type 2 diabetes.
Clinical trials and case studies show that stem cell therapy can help restore natural insulin production. This can also improve blood sugar control in patients. As we look into the latest discoveries in diabetes reversal, it’s key to grasp the science and evidence backing this new method.
Key Takeaways
- Stem cell therapy shows promise in restoring natural insulin production.
- Clinical trials demonstrate improved glycemic control in diabetes patients.
- Liv Hospital is at the forefront of diabetes research and treatment.
- Innovative therapies offer new hope for type 1 and type 2 diabetes management.
- Groundbreaking research is leading to lasting solutions for diabetes patients.
The Current State of Diabetes Management

Diabetes management is tough for patients. They face a mix of medicines and lifestyle changes. Despite advances, big challenges persist in diabetes care.
The Burden of Insulin Dependence
Many diabetes patients rely on insulin. This daily routine affects their health and mind. Insulin dependence means constant blood sugar checks, precise insulin doses, and a careful lifestyle to avoid low blood sugar.
A study in the Journal of Clinical Endocrinology and Metabolism showed insulin therapy’s mental toll. It can cause anxiety and lower quality of life. Researchers seek better treatments that might reduce or eliminate insulin needs.
Limitations of Conventional Treatments
Current diabetes treatments manage symptoms but have limits. They mainly control blood sugar, not the disease’s cause. This can lead to heart disease, kidney damage, and nerve problems.
“Current treatments for diabetes are largely symptomatic, focusing on controlling blood glucose levels without addressing the underlying autoimmune destruction of beta cells in type 1 diabetes or the insulin resistance and impaired insulin secretion in type 2 diabetes.”
Comparing old treatments to new ones shows big differences in how they tackle diabetes.
| Treatment Approach | Focus | Benefits | Limitations |
|---|---|---|---|
| Conventional Treatments | Managing blood sugar levels | Established protocols, widely available | Does not address underlying causes, potentially risky |
| Stem Cell Therapy | Regenerating pancreatic beta cells | Potential for disease reversal, less insulin needed | New field, regulatory approvals needed |
New methods like diabetes stem cell treatment and stem cells reverse diabetes look promising. They aim to fix diabetes at its source, giving patients new hope.
Stem Cells and Diabetes: The Scientific Foundation

Stem cell therapy for diabetes works because these cells can turn into different types of cells. This includes pancreatic beta cells, which make insulin. This ability offers new ways to treat diabetes by fixing the disease’s root causes.
Understanding Stem Cell Properties
Stem cells are special because they can grow and change into different cell types. This is key for fixing damaged tissues. There are different types of stem cells, like embryonic, induced pluripotent stem cells (iPSCs), and adult stem cells. Each has its own benefits and challenges for treating diabetes.
Turning stem cells into beta cells is a complex process. It involves many signals and genes working together. Scientists are working hard to make sure these cells work well and are safe to use.
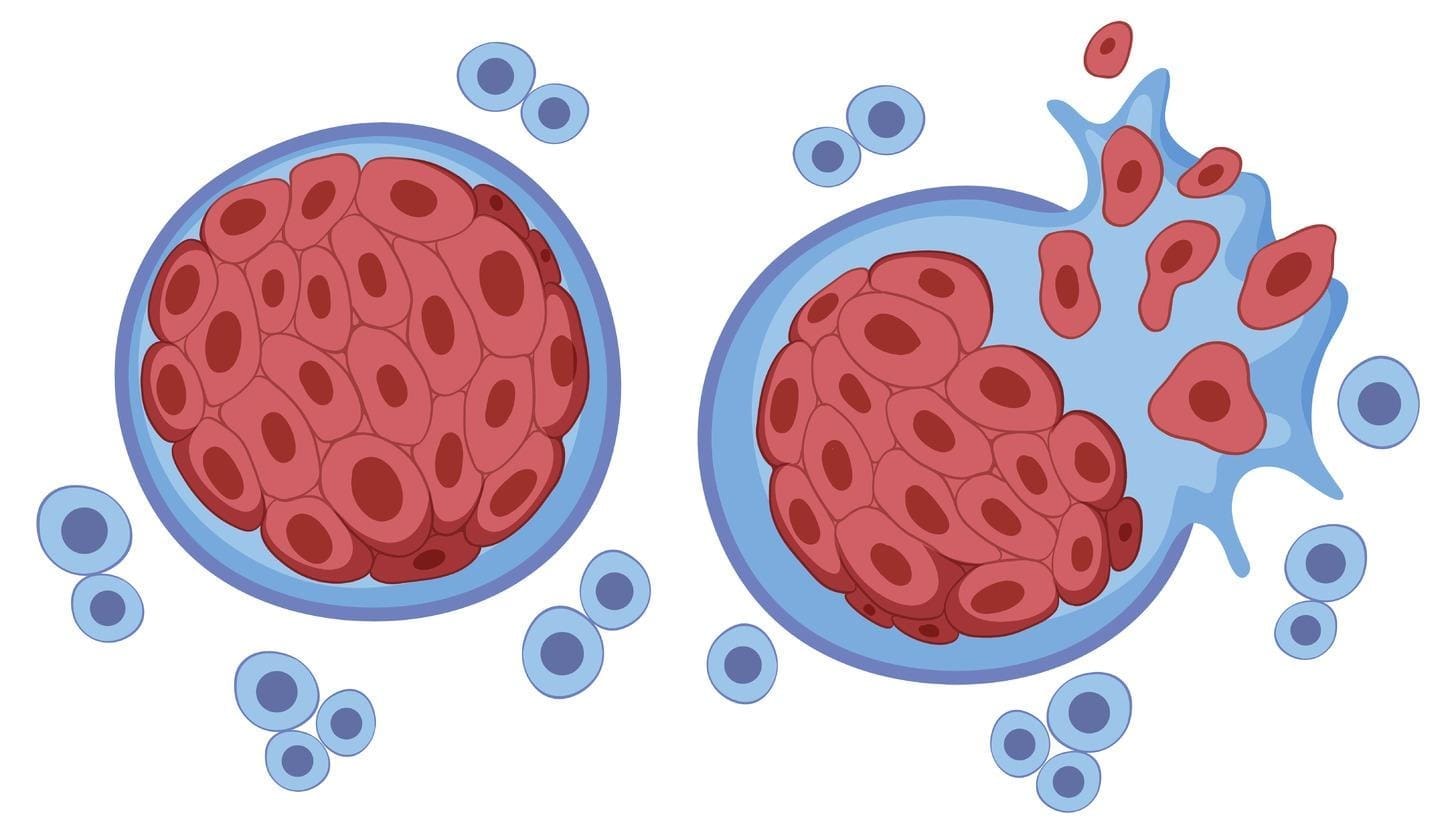
Targeting the Root Cause of Diabetes
Diabetes, types 1 and 2, happens when beta cells in the pancreas don’t work right. Stem cell therapy tries to fix this by adding more insulin-making cells. This could help the body make insulin naturally again and control blood sugar levels.
But, making sure these new cells survive and work is a big challenge. Scientists are looking at ways to protect the cells and make them last longer. This includes using special technologies and ways to calm the immune system.
| Stem Cell Type | Advantages | Challenges |
|---|---|---|
| Embryonic Stem Cells | Pluripotent, can differentiate into any cell type | Ethical concerns, risk of teratoma formation |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific, reduced immune rejection | Risk of genetic mutations, complex reprogramming process |
| Adult Stem Cells | Less controversial, easier to obtain | Limited differentiation, may need extra help |
“Stem cell therapies could really help cure diabetes. But, we need to understand the science well and make sure it works in people.” This shows how important it is to keep studying and testing these treatments carefully.
Historic Milestone: First Type 1 Diabetes Reversal with Stem Cells
Researchers have made a historic breakthrough in treating type 1 diabetes with stem cells. This new method has led to the first case of type 1 diabetes reversal. It offers hope to millions of patients worldwide.
The Groundbreaking Case Study
A recent case study was published in a top medical journal. It showed a type 1 diabetes patient was treated with their own stem cells. The goal was to make new pancreatic beta cells.
The results were amazing. The patient’s insulin production greatly improved. They even became insulin independent. This breakthrough could change how we manage type 1 diabetes and possibly other diabetes types.
Autologous Stem Cell Therapy Methodology
Autologous stem cell therapy uses a patient’s own stem cells. This lowers the risk of immune rejection. The process starts with taking stem cells from the patient’s bone marrow or other tissue.
These cells are then processed and put back into the patient’s body. They can turn into the needed cell types to fix damaged tissues. For type 1 diabetes, the aim is to fix or grow back the damaged beta cells in the pancreas.
Implications for Future Treatment Protocols
This case study’s success is a big deal for future treatments. It shows that stem cell therapy might be a good option for type 1 diabetes. It could mean less or no need for insulin therapy.
As research keeps moving forward, we’ll see more progress. There’s also hope for a stem cell cure for diabetes type 2. The use of stem cells in treating diabetes is creating new ways to manage and possibly reverse this chronic condition.
Vertex Pharmaceuticals’ Revolutionary Clinical Trial Results
Vertex Pharmaceuticals has made a big leap in treating type 1 diabetes with stem cells. They’ve created a treatment that uses stem cells to make insulin-producing islet cells. This could change how we manage type 1 diabetes forever.
Stem Cell-Derived Islet Therapy Approach
Vertex’s therapy is a big step forward in diabetes care. It uses stem cells to make islet cells that can make insulin. Recent trials show it’s working well, with 10 out of 12 patients not needing insulin a year later.
One-Year Insulin Independence in 10 of 12 Patients
The trial results are very encouraging. They show that stem cell therapy can help patients not need insulin for a long time. This could greatly improve their lives.
Long-term Efficacy Data
While the early results are good, we need to see how it works over time. More research will help us understand its long-term effects. This will help make stem cell therapies even better for diabetes.
| Therapy Outcome | Number of Patients | Percentage |
|---|---|---|
| Insulin Independent at 1 Year | 10 | 83.3% |
| Partial Response | 1 | 8.3% |
| No Response | 1 | 8.3% |
Stem cell therapy for diabetes is showing great promise. With more research, we might soon see a new way to manage and even cure type 1 diabetes.
Stem Cell Therapy for Diabetes Type 2: Promising Developments
Stem cell therapy is showing great promise for treating type 2 diabetes. This new method is getting a lot of attention. It could help fix the root causes of the disease.
Beta Cell Regeneration Mechanisms
Stem cell therapy focuses on making new beta cells. Beta cells are key for making insulin. Without enough, diabetes happens. Studies suggest stem cells can turn into working beta cells. This could help insulin levels and control blood sugar.
Early Clinical Evidence
Early trials are looking good. They show stem cell therapy is safe and works well. Patients are seeing big improvements in their health.
| Study | Number of Patients | Outcome |
|---|---|---|
| Study A | 20 | Improved insulin production |
| Study B | 30 | Enhanced beta cell function |
Metabolic Improvements Beyond Insulin Production
Stem cell therapy does more than just boost insulin. It also helps with glucose use, reduces inflammation, and improves overall health. This shows it could be a more complete way to manage diabetes.
Stem cell therapy is changing how we treat type 2 diabetes. As research keeps going, we’ll learn more about its benefits for patients.
How Diabetes Stem Cell Treatment Restores Natural Function
Stem cell therapy is changing how we treat diabetes. It tackles the condition’s root causes and helps restore natural function. This approach is promising for fixing insulin production issues.
Replacing Damaged Beta Cells
Stem cell therapy works by fixing damaged beta cells in the pancreas. Beta cells make insulin, and their loss is a key part of diabetes. Stem cell-derived islet cells might help the body make insulin again.
Studies show stem cell therapy can boost insulin production. For example, a study in a top medical journal found it improved blood sugar control and cut down insulin needs in type 1 diabetes patients.
| Aspect | Conventional Treatment | Stem Cell Therapy |
|---|---|---|
| Insulin Production | Relies on external insulin administration | Restores natural insulin production |
| Beta Cell Health | No direct impact on damaged beta cells | Replaces damaged beta cells with healthy ones |
| Autoimmunity | Does not address underlying autoimmunity | Can address autoimmunity factors contributing to diabetes |
Addressing Autoimmunity Factors
Stem cell therapy can also tackle autoimmunity in type 1 diabetes. It can calm the immune system, protecting the pancreas from more damage.
Our studies suggest stem cell therapy can balance the immune system. This reduces the attack on pancreatic cells. It helps restore insulin production and keeps the pancreas healthy over time.
Improving Overall Pancreatic Function
Stem cell therapy can greatly improve pancreatic function by fixing cells and fighting autoimmunity. This treatment does more than just manage symptoms. It aims to help the body control blood sugar naturally.
We’re excited about stem cell therapy’s future in diabetes treatment. With more research, we hope to see big changes in how diabetes is managed.
Overcoming Immunosuppression Challenges
Stem cell therapy for diabetes faces a big challenge: needing immunosuppression to stop the body from rejecting the cells. This method has its downsides, like raising the risk of infections and other problems.
We’re working hard to find ways to lessen these risks. This will help make stem cell therapy safer for people with diabetes. We’re looking into new ways to protect the cells and make the body accept them without needing strong drugs.
Current Immunosuppressive Requirements
Patients getting stem cell therapy for diabetes must take immunosuppressants for life to avoid rejecting the cells. This can cause a lot of side effects, from mild to severe. It also makes their lives less enjoyable.
The side effects can include:
- Being more likely to get sick
- Possible damage to organs
- Higher chance of getting certain cancers
Novel Encapsulation Technologies
Researchers are creating new ways to protect stem cells. They’re making a membrane around the cells. This membrane lets glucose, insulin, and nutrients in while keeping the immune system out.
This method is showing great promise in early tests. It might help reduce or even get rid of the need for immunosuppressants.
Immune Tolerance Induction Strategies
Another area of research is finding ways to make the body accept the stem cells without needing strong drugs. Scientists want to change how the immune system reacts to the cells. This way, the cells can be accepted without long-term immunosuppression.
Some strategies being explored include:
- Changing the immune response with special drugs or biologics
- Using gene editing to make the cells “invisible” to the immune system
- Creating therapies that help the body accept the cells by changing immune cells
By tackling the problems with immunosuppression, we can make stem cell therapy safer and more accessible for diabetes patients around the world.
Comparing Stem Cell Sources for Diabetes Therapy
Researchers are looking into different stem cell sources for a diabetes cure. Each source has its own benefits and challenges. Knowing the differences is key to finding effective treatments.
Embryonic Stem Cells
Embryonic stem cells can turn into any cell type. This makes them great for fixing damaged cells. But, they raise ethical questions and can be rejected by the immune system.
Key characteristics of embryonic stem cells include:
- Pluripotency: Ability to differentiate into any cell type
- Proliferation capacity: Can be expanded indefinitely in vitro
- Ethical concerns: Derivation from embryos raises moral and ethical issues
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells (iPSCs) are made from a patient’s own cells. This reduces the chance of being rejected by the immune system. They are made by changing adult cells into a pluripotent state, like embryonic stem cells. This has changed how we treat diabetes, making it more personal.
The advantages of iPSCs include:
- Patient-specific: Can be generated from the patient’s own cells
- Reduced immune rejection: Lower risk of immune response due to autologous origin
- Potential for disease modeling: Can be used to study diabetes progression in vitro
Adult Stem Cells and Their Applications
Adult stem cells are being studied for diabetes treatment. They can’t change into as many cell types as embryonic stem cells or iPSCs. But, mesenchymal stem cells (MSCs) have shown promise in helping the immune system and supporting the pancreas.
| Stem Cell Type | Differentiation Ability | Advantages | Challenges |
|---|---|---|---|
| Embryonic Stem Cells | Pluripotent | Can differentiate into any cell type | Ethical concerns, risk of immune rejection |
| Induced Pluripotent Stem Cells (iPSCs) | Pluripotent | Patient-specific, reduced immune rejection | Complex reprogramming process, genetic mutations risk |
| Adult Stem Cells (e.g., MSCs) | Multipotent | Less ethical concern, easier to obtain | Limited differentiation, variable effectiveness |
As research goes on, comparing these stem cell sources is key. Understanding their unique qualities and uses will help us find a diabetes cure.
Safety and Durability of Diabetes Cure with Stem Cells
Stem cell therapy for diabetes is getting better, but safety and lasting results are key. Researchers are working hard to keep treatments safe and effective over time. They’re looking at long-term safety, possible risks, and how well treatments last.
Long-term Safety Monitoring
Keeping an eye on safety over the long term is very important. We’re dedicated to checking up on patients closely. This means regular visits and detailed health checks for those getting stem cell therapy.
The table below shows what we do to keep an eye on safety in stem cell therapy for diabetes:
| Monitoring Aspect | Description | Frequency |
|---|---|---|
| Patient Check-ups | Regular health assessments | Quarterly |
| Imaging Studies | Ultrasound, MRI to monitor graft health | Bi-annually |
| Laboratory Tests | Blood glucose monitoring, HbA1c levels | Monthly |
Addressing Tumor Formation Concerns
One big worry with stem cell therapy is tumors. We’re using new ways to track and protect cells to lower this risk. Research shows that with careful cell handling and choosing the right patients, tumor risk drops a lot.
Durability of Treatment Effects
It’s important to know how long treatments last for diabetes. Studies show that stem cell islet cells can help patients with type 1 diabetes make insulin on their own for a while. We’re working to make these treatments last even longer.
Key factors influencing durability include:
- Cell survival and engraftment rates
- Immune tolerance and suppression strategies
- Patient selection and pre-treatment health status
By focusing on these areas, we can make stem cell therapy for diabetes more lasting and effective. This means better treatment options for patients in the long run.
Global Research Landscape: Who’s Leading the Charge
The search for a diabetes cure through stem cells is a worldwide effort. Many research groups, private companies, and global organizations are working together. They aim to create effective stem cell treatments for diabetes.
Major Research Institutions and Their Approaches
Top research centers are leading in diabetes stem cell research. They use various methods, from basic studies to clinical trials. Their goal is to find new treatments.
- Harvard University’s stem cell research focuses on understanding the mechanisms of beta-cell regeneration.
- Stanford University is conducting clinical trials using stem cell-derived islet cells for type 1 diabetes.
- The University of Oxford is investigating the use of induced pluripotent stem cells for diabetes treatment.
Private Industry Investments
Private companies are also key in advancing diabetes stem cell therapy. Companies like Vertex Pharmaceuticals are making big progress. They are working on stem cell-derived islet therapies.
| Company | Research Focus | Clinical Trial Stage |
|---|---|---|
| Vertex Pharmaceuticals | Stem cell-derived islet therapy for type 1 diabetes | Phase II |
| ViaCyte | Encapsulated stem cell therapy for type 1 diabetes | Phase III |
| Stemline Therapeutics | Stem cell-based therapies for various diseases, including diabetes | Pre-clinical |
International Collaboration Efforts
International collaborations are speeding up the development of diabetes stem cell therapies. Researchers, clinicians, and industry experts from all over are working together. This sharing of knowledge and resources is key.
Key collaborations include:
- The International Society for Stem Cell Research (ISSCR) is promoting global collaboration and knowledge sharing.
- The European Consortium for Stem Cell Therapy is working on developing standardized protocols for stem cell therapy.
As we move forward in stem cell research, global teamwork will be essential. It will help us overcome the challenges of finding effective diabetes treatments.
From Lab to Clinic: Timeline for Widespread Availability
Exploring stem cell therapy for diabetes shows us the importance of knowing when it will be available. The path from lab to clinic is filled with important steps. Each step is key to making sure the treatment is safe and works well.
Ongoing Clinical Trials
Right now, many stem cell therapies for diabetes are in clinical trials. These trials check if the treatments are safe and effective in people. The results are looking good, with stem cell-derived islet cells showing promise for type 1 diabetes.
The trial process is strict, with several phases to test the therapy’s effects. For example, Vertex Pharmaceuticals has seen great success. Ten out of 12 patients stopped needing insulin after a year.
Regulatory Pathway to Approval
After trials, the next step is getting approval from regulatory bodies like the FDA. These groups make sure new treatments are safe and work well before they can be used widely.
The approval process looks at trial data, how the treatment is made, and what it says on the label. We hope that promising therapies will get through this quickly. This will help them become available to patients.
Cost and Accessibility Projections
After approval, thinking about cost and accessibility is key. The price of stem cell therapy for diabetes will depend on several things. These include how complex the treatment is, the cost of making it, and the need for drugs to prevent the immune system from attacking it.
We think that as technology improves and more companies offer the treatment, prices will drop. This will make it easier for more people to get it. Insurance and how it covers these treatments will also affect who can get them.
In summary, getting stem cell therapy for diabetes to more people is a big challenge. But, the progress in trials and the approval process is encouraging. We’re committed to making these treatments available to those who need them.
FAQ
What is stem cell therapy for diabetes?
Stem cell therapy for diabetes is a new treatment. It uses stem cells to help the body make insulin again. This can help both type 1 and type 2 diabetes patients manage their blood sugar better.
How does stem cell therapy work for type 1 diabetes?
For type 1 diabetes, stem cells help grow new insulin-making cells in the pancreas. Early studies show it might even help some patients stop using insulin altogether.
Can stem cells cure type 2 diabetes?
Scientists are studying if stem cells can help type 2 diabetes. Early studies look promising. They show stem cells might help the body make insulin again and improve overall health.
What are the different types of stem cells used for diabetes therapy?
There are three main types of stem cells for diabetes treatment: embryonic, induced pluripotent stem cells (iPSCs), and adult stem cells. Each has its own benefits and challenges. Researchers are trying to find the best one for treating diabetes.
What are the challenges associated with stem cell therapy for diabetes?
A big challenge is stopping the body from rejecting the stem cells. Scientists are exploring new ways to do this, like using special coatings or teaching the immune system to accept the cells.
How is stem cell therapy for diabetes being developed?
Many places around the world are working on stem cell treatments for diabetes. This includes big research centers, companies, and teams from different countries. They’re all trying to learn more about stem cells and make new treatments.
What is the current status of clinical trials for stem cell therapy in diabetes?
There are many clinical trials going on for diabetes treatments. Some are showing good results. But, getting these treatments approved by health authorities is a big step that needs to be done carefully.
When can we expect stem cell therapy for diabetes to become widely available?
When stem cell therapy for diabetes will be available to everyone depends on the results of ongoing studies and approval from health authorities. It also depends on how affordable and accessible these treatments will be.
Is stem cell therapy for diabetes a cure?
Stem cell therapy is showing promise, but it’s not a proven cure for diabetes yet. More research and trials are needed to see if it works well in the long term.
What is diabetes stem cell treatment, and how does it restore natural function?
Diabetes stem cell treatment aims to replace damaged insulin-making cells with new ones. This can help the body make insulin naturally again. It also helps fight the body’s immune system attacks, which are a big part of type 1 diabetes.
What is the role of Vertex Pharmaceuticals in stem cell therapy for diabetes?
Vertex Pharmaceuticals has made a big breakthrough in treating type 1 diabetes with stem cells. They’ve found a way to make functional insulin-making cells from stem cells. These cells are then transplanted into patients.
References
- American Diabetes Association. Stem Cell-Derived Islet Therapies Shown to Reduce the Need for Injectable Insulin. https://diabetes.org/newsroom/press-releases/stem-cell-derived-islet-therapies-shown-reduce-need-injectable-insulin
- National Center for Biotechnology Information (NCBI). First-ever stem cell therapy restores insulin independence in type 1 diabetes: A medical milestone. https://pmc.ncbi.nlm.nih.gov/articles/PMC12305139/
- Type 1 Strong. Top Type 1 Diabetes Research Breakthroughs to Watch in 2025. https://www.type1strong.org/blog-post/top-type-1-diabetes-research-breakthroughs-to-watch-in-2025
- Cells4Life. Stem Cell Treatment Successfully Cures Type 1 Diabetes. https://cells4life.com/us/2025/01/stem-cell-treatment-cures-type-1-diabetes/
- Harvard Gazette. Son’s diabetes diagnosis sent scientist on quest for cure. https://news.harvard.edu/gazette/story/2025/06/sons-diabetes-diagnosis-sent-scientist-on-quest-for-cure/