The world of hematopoietic stem cells (HSCs) is at the core of modern regenerative medicine. These rare, multipotent cells are found mainly in the bone marrow. They are vital for creating all blood cells through a complex process called hematopoiesis.
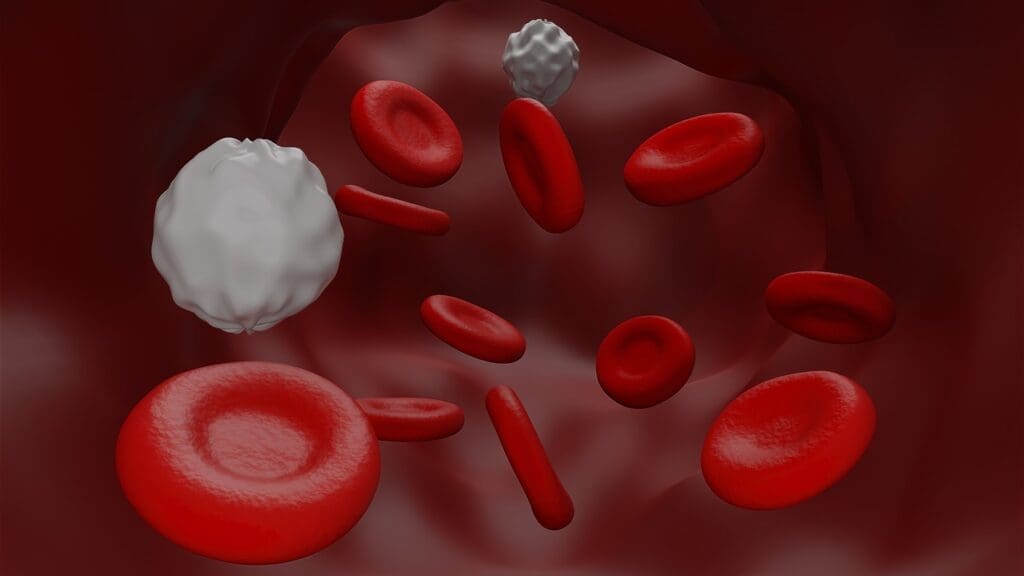
HSCs have a special gift. They can renew themselves and turn into different blood cell types. This includes red blood cells, white blood cells, and platelets. Their role is key to keeping our blood healthy, ensuring oxygen transport, immune defense, and coagulation.
Key Takeaways
- HSCs are rare, multipotent cells mainly in the bone marrow.
- They are essential for making all blood cell types through hematopoiesis.
- Their ability to self-renew and differentiate is vital for a healthy blood cell count.
- HSCs are key for oxygen transport, immune defense, and coagulation.
- Understanding HSCs is vital for treating hematologic diseases.
What Are Hematopoietic Stem Cells (HSCs)?
The human body needs Hematopoietic Stem Cells (HSCs) to make all blood cells. They are key to our survival. HSCs can renew themselves and turn into any blood cell type, a process called hematopoiesis.
Definition and Rarity of Multipotent Hematopoietic Stem Cells
HSCs can make every blood cell type, including red and white blood cells, and platelets. They are very rare, making up a small part of bone marrow cells. Yet, they are very powerful, helping keep our blood cell levels up throughout our lives.
Historical Discovery and Research Milestones
Research on HSCs started in the mid-20th century. Key moments include finding out HSCs’ role in making blood cells and their use in regenerative medicine. Our knowledge of HSCs has grown, showing their complex biology and how they work.
This understanding has led to better HSC transplantation and therapy. We keep studying HSCs to improve treatments for blood disorders and understand the hematopoietic system better.
Key Fact #1: Hematopoietic Stem Cells HSCs Are the Source of All Blood Cells
Hematopoietic Stem Cells (HSCs) are the base of our blood system. They create all blood cell types throughout our lives. HSCs make red blood cells, white blood cells, and platelets. These cells are key for carrying oxygen, fighting infections, and clotting blood.
The Process of Hematopoiesis
Hematopoiesis is how HSCs turn into different blood cells. It involves growth factors, cytokines, and transcription factors. These help multipotent hematopoietic stem cells become specific blood cell types.
How HSCs Maintain Blood Cell Production Throughout Life
HSCs keep making blood cells all our lives. They do this by balancing self-renewal and differentiation. Some HSCs become specific blood cells, while others stay stem cells. This keeps the blood cell supply steady.
Regulating HSCs is complex. It’s vital for our health. Understanding how HSCs work is key to knowing their role in health and disease.
Key Fact #2: The Unique Self-Renewal Ability of HSCs
Hematopoietic Stem Cells (HSCs) have a special ability to renew themselves. This is key for their survival and function. They can keep their numbers up and make blood cells all our lives.
Mechanisms of Self-Renewal
The self-renewal of HSCs is complex. It involves many molecular mechanisms. A network of signaling pathways and transcription factors keeps the balance right.
Key regulators include specific transcription factors and cytokines that promote or inhibit self-renewal.
Balance Between Self-Renewal and Differentiation
Keeping the balance between self-renewal and differentiation is vital. Self-renewal keeps the HSC pool steady. Differentiation lets them make different blood cell types.
This delicate balance is achieved through the coordinated action of multiple regulatory elements.
Factors Influencing Self-Renewal Decisions
Many factors affect HSCs’ self-renewal choices. These include:
- Intrinsic factors, such as transcription factors and cell cycle regulators
- Extrinsic factors, including cytokines and signals from the bone marrow niche
- Environmental cues, such as stress and injury signals
Understanding these factors is key to seeing how HSCs keep their numbers up.
Key Fact #3: Differentiation Pathways of Hematopoietic Cell Lineages
Hematopoietic Stem Cells (HSCs) can turn into different blood cell types. Each type has its own job to keep us healthy. This process is key to making the many blood cells our bodies need.
Red Blood Cells: Oxygen Transport
Red blood cells carry oxygen from our lungs to our body’s tissues. They have a protein called hemoglobin that holds onto oxygen. Making red blood cells involves many growth factors and transcription factors working together.
White Blood Cells: Immune Defense
White blood cells help fight off infections and invaders. There are many types, like neutrophils, lymphocytes, and monocytes. Each type has its own role in keeping us safe. The making of white blood cells is controlled by cytokines and transcription factors.
Platelets: Blood Coagulation
Platelets are small cells that help our blood clot. When we get a cut, platelets form a plug to stop the bleeding. Thrombopoietin, a cytokine, helps turn HSCs into megakaryocytes, which then become platelets.
| Blood Cell Type | Function | Key Regulators |
|---|---|---|
| Red Blood Cells | Oxygen Transport | Hemoglobin, Erythropoietin |
| White Blood Cells | Immune Defense | Cytokines, Transcription Factors |
| Platelets | Blood Coagulation | Thrombopoietin, Megakaryocytes |
In summary, HSCs turn into different blood cells, each with its own job. Knowing how this works helps us understand the complex world of blood cell creation. It’s key to understanding health and disease.
Key Fact #4: Hematopoietic Progenitor Cells as Intermediate Cells
Hematopoietic progenitors act as a middle ground between HSCs and fully formed blood cells. They come from HSCs and help create more specialized cells. This is key in the process of hematopoiesis.
Differences Between HSCs and Hematopoietic Progenitors
HSCs can keep themselves going, but hematopoietic progenitors focus more on growing into different types of cells. This difference is important for understanding how the hematopoietic stem cell lineage grows and changes.
Types and Functions of Progenitor Cells
There are two main types of hematopoietic progenitors: Common Myeloid Progenitors (CMPs) and Common Lymphoid Progenitors (CLPs). Each type has its own job and helps create different kinds of blood cells.
Common Myeloid Progenitors (CMPs)
CMPs turn into myeloid cells like monocytes, macrophages, neutrophils, and red blood cells. These cells are important for fighting off infections and carrying oxygen.
Common Lymphoid Progenitors (CLPs)
CLPs become lymphoid cells, including T cells, B cells, and natural killer cells. These cells are vital for our immune system’s ability to adapt to new threats.
Grasping the role of hematopoietic progenitors is key to understanding hematopoiesis. It also helps in developing treatments for blood-related diseases.
Key Fact #5: Myeloid and Lymphoid Lineages in Hematopoiesis
Myeloid and lymphoid lineages start from HSCs. They are key to our immune system and health. Knowing about them helps us see how HSCs protect us and carry oxygen.
The Myeloid Pathway: Cells and Functions
The myeloid pathway creates blood cells like monocytes and neutrophils. These cells are important for:
- Immune defense
- Oxygen transport
- Handling inflammation
The Lymphoid Pathway: Cells and Functions
The lymphoid pathway makes lymphocytes, like T cells and B cells. These cells are vital for:
- Adaptive immune responses
- Cell-mediated immunity
- Producing antibodies
This lineage helps our body fight off infections.
Lineage Commitment Factors
What makes HSCs choose myeloid or lymphoid lineage? It’s due to:
- Cytokines and growth factors
- Transcription factors
- Signaling pathways
These elements control which genes are turned on or off in HSCs.
In summary, myeloid and lymphoid lineages are vital to our blood system. Problems with them can cause blood disorders. Studying how they decide their path is key to finding treatments.
Key Fact #6: Cytokines Regulate Hematopoietic Stem Cell Lineage Commitment
Cytokines play a big role in guiding HSCs to choose their path. They are like messengers between cells, helping them decide what to do next. In the world of blood cells, cytokines help HSCs pick their line of work.
Essential Cytokines in HSC Regulation
Some cytokines are key for HSCs. They include:
- Stem Cell Factor (SCF): important for HSC survival and growth.
- Thrombopoietin (TPO): helps keep HSCs healthy and supports blood platelet formation.
- Interleukins (ILs): different ILs help with different HSC tasks and choices.
Signaling Pathways in Lineage Determination
Cytokines work through special paths to send messages. For example, the JAK/STAT pathway is a main way many cytokines talk to HSCs. Knowing these paths helps us understand how HSCs are controlled.
Clinical Applications of Cytokine Therapy
Cytokine therapy is used in many ways, like helping blood cells recover after bone marrow transplants. Doctors use specific cytokines to help HSCs grow and change, making patients do better.
| Cytokine | Function |
|---|---|
| SCF | HSC survival and self-renewal |
| TPO | HSC maintenance and megakaryocyte development |
| ILs | Regulation of HSC function and lineage commitment |
“Cytokines are key in controlling blood cell creation, opening doors for treatments in blood diseases.”
Key Fact #7: Bone Marrow Niches Are Critical for HSC Maintenance
The bone marrow niche is vital for hematopoietic stem cells (HSCs) to work right. We’ll see how this special place helps keep HSCs healthy.
Components of the HSC Microenvironment
The HSC microenvironment, or niche, has different cells like osteoblasts and endothelial cells. These cells make substances that help HSCs grow and change. This is shown in studies on HSC regulation.
Endosteal vs. Vascular Niches
The bone marrow has two main niches: the endosteal and vascular. The endosteal niche is near the bone and is quieter. The vascular niche, linked to blood vessels, is busier. Each niche has its own role in managing HSCs.
Niche Factors Supporting HSC Function
Niche factors like cytokines and growth factors help HSCs. For example, stem cell factor (SCF) and thrombopoietin (TPO) are important for HSC survival and growth. Knowing about these factors helps in making treatments for HSCs.
HSC Transplantation: A Life-Saving Procedure
Hematopoietic Stem Cell (HSC) transplantation is a key treatment for serious blood disorders. It uses HSCs from different sources to fix the patient’s blood-making system.
Sources of Hematopoietic Stem Cells for Transplantation
HSCs for transplant come from various places, including:
- Bone Marrow: Bone marrow has long been the main source for HSCs.
- Peripheral Blood: Mobilized blood stem cells are now common due to their easy collection and quick start.
- Umbilical Cord Blood: Cord blood is valuable, mainly for those without a matched donor.
Conditions Treated with HSC Transplantation
HSC transplantation helps many blood diseases, including:
- Leukemia: It treats both acute and chronic leukemia.
- Lymphoma: It’s used for lymphoma that doesn’t respond to usual treatments.
- Aplastic Anemia: A condition where the bone marrow can’t make blood cells.
- Multiple Myeloma: It’s for advanced cases of this plasma cell cancer.
Transplantation Process and Challenges
The HSC transplant process includes many steps, from finding a donor to aftercare. Despite its benefits, it faces big challenges, such as:
- Graft-versus-Host Disease (GVHD): A complication where donor cells attack the recipient’s body.
- Infection Risk: Patients are at high risk of infections when their immune system is weak.
- Organ Toxicity: The treatments can harm different organs.
We’re working to improve HSC transplant methods. This aims to better patient results and make this life-saving treatment more available.
Current Research and Future Directions in Hematopoietic Stem Cell Biology
Hematopoietic stem cell research is on the verge of a major breakthrough. This is thanks to advances in gene editing, gene therapy, and regenerative medicine. These developments are changing how we understand HSC biology, leading to new ways to treat diseases.
Emerging Technologies in HSC Research
New technologies like single-cell RNA sequencing and advanced imaging are giving us deep insights into HSCs. They help us see how different HSCs work together and how they fit into their environment.
Gene Therapy and HSC Modification
Gene therapy is being tested to change HSCs for healing. By fixing genes in HSCs, we might cure genetic diseases affecting blood cells. Early studies look promising, and we’re moving these ideas into real treatments.
Potential Applications in Regenerative Medicine
HSC research could lead to big changes in regenerative medicine. HSCs might help fix damaged tissues and bring back healthy blood-making in patients with blood disorders. We’re also looking at combining HSCs with other cells to improve healing.
As we learn more about HSC biology, we’re getting closer to new treatments for blood diseases. The future of HSC research is bright, with the chance to greatly improve patient care and save lives.
Conclusion: The Critical Importance of HSCs in Human Health
Hematopoietic stem cells (HSCs) play a key role in keeping our blood healthy. They are the only source of all blood cells. Their ability to self-renew helps keep blood cell production going all our lives.
When HSCs don’t work right, it can cause many blood-related diseases. This shows how important they are for our health. We need to keep studying HSCs to learn more about their role in health and sickness.
Thanks to HSC research, we have treatments like HSC transplantation that save lives. More studies on these cells will help us understand how blood is made. This knowledge is vital for finding new ways to treat diseases.
As we learn more about HSCs, we might find new ways to help people stay healthy. The role of HSCs in making blood cells highlights the need for more research in this area.
What are hematopoietic stem cells (HSCs)?
Hematopoietic stem cells (HSCs) are found in the bone marrow. They are key in making all blood cell types.
What is the role of HSCs in blood cell formation?
HSCs are the source of all blood cells. They turn into different blood cell types. These cells are vital for carrying oxygen, fighting infections, and clotting blood.
What is hematopoiesis?
Hematopoiesis is the process of HSCs turning into different blood cell types. It ensures we always have enough blood cells.
How do HSCs maintain their population?
HSCs keep their numbers up by self-renewing and differentiating. Self-renewal helps them replenish, while differentiation creates new blood cells.
What are hematopoietic progenitor cells?
Hematopoietic progenitor cells are cells that come from HSCs. They turn into specific blood cell types, like myeloid and lymphoid cells.
What is the significance of bone marrow niches in HSC maintenance?
Bone marrow niches support HSCs. They help with self-renewal, differentiation, and survival. This is vital for HSC function.
What is HSC transplantation?
HSC transplantation is a treatment for blood disorders. It involves giving HSCs from a donor or the patient to replace damaged blood cells.
What are the sources of HSCs for transplantation?
HSCs can come from bone marrow, blood, or umbilical cord blood. Each source has its own benefits and drawbacks.
What are the current research directions in HSC biology?
Research in HSC biology is exploring new technologies and gene therapy. It aims to improve our understanding and find new treatments.
What is the role of cytokines in regulating HSC lineage commitment?
Cytokines are important in guiding HSCs to become specific blood cells. They help balance self-renewal and differentiation.
What is the significance of HSCs in human health?
HSCs are essential for a healthy blood cell count. Their problems can lead to blood disorders, making them vital for health.
References
- National Center for Biotechnology Information (NCBI) / Books: https://www.ncbi.nlm.nih.gov/books/NBK544245/
- Abcam: https://www.abcam.com/en-us/knowledge-center/stem-cells/hematopoietic-stem-cells
- American Society of Hematology (ASH): https://www.hematology.org/education/patients/blood-basics










