Last Updated on November 17, 2025 by Ugurkan Demir

At LivHospital, we know how complex bone marrow disorders can be. Bone marrow is the soft tissue inside bones where blood cells are made. It has stem cells that turn into red cells, white cells, and platelets. These cells help fight infections, carry oxygen, and heal our bodies.
We will look at 10 common bone marrow conditions. These include aplastic anemia, Fanconi anemia, myelodysplastic syndromes, and myeloproliferative neoplasms. Knowing about these conditions helps us diagnose and treat them better. This improves the lives of those affected.
Key Takeaways
- Understanding bone marrow’s role in producing blood cells is vital.
- Both cancerous and non-cancerous disorders can affect bone marrow.
- Timely diagnosis is key for effective care and better quality of life.
- LivHospital offers full support and guidance for international patients.
- Our team combines medical knowledge with empathy and understanding.
Understanding Bone Marrow Blood Disease: Functions and Pathology

Bone marrow is key to making blood cells in our body. Problems with it can cause serious health issues. It’s the soft tissue inside bones like hips and thighbones, making blood cells.
The Role of Bone Marrow in Blood Cell Production
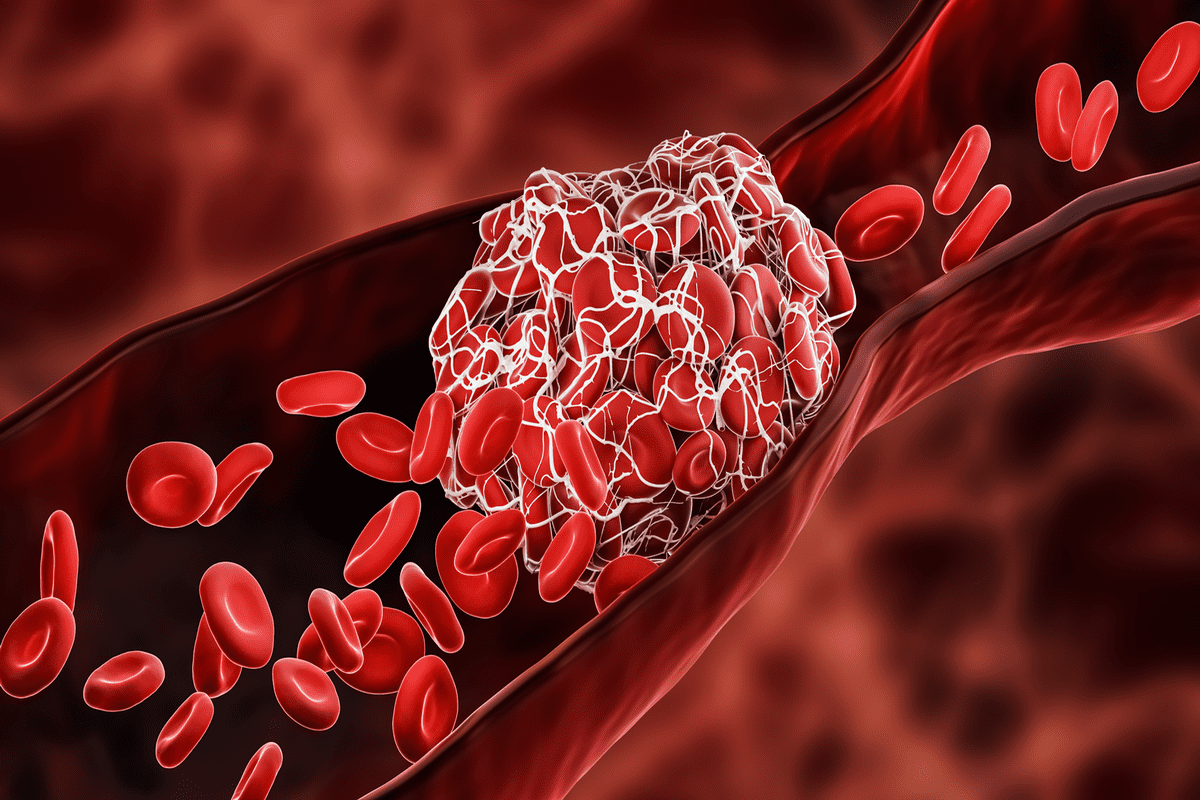
Bone marrow is vital for making red blood cells, white blood cells, and platelets. Red blood cells carry oxygen to our body. White blood cells fight infections, and platelets help blood clot.
The process of making blood cells is complex. It involves many cell types and growth factors working together.
How Disorders Affect Blood Cell Development
Disorders in bone marrow can harm blood cell production or function. For example, aplastic anemia makes the bone marrow fail to make blood cells. This leads to anemia, infections, and bleeding.
Other disorders, like myelodysplastic syndromes, make abnormal blood cells. These cells can’t function right.
Common Symptoms of Bone Marrow Dysfunction
Symptoms of bone marrow problems vary by disorder. But common signs include fatigue, frequent infections, and bleeding or bruising. Knowing these symptoms helps in early diagnosis and treatment.
Aplastic Anemia: A Critical Non-Cancerous Bone Marrow Failure
Aplastic anemia is a rare and serious condition where the bone marrow fails to make blood cells. This failure can cause severe infections, anemia, and bleeding. We will look into what causes this, its symptoms, and how it’s treated.
Mechanisms and Causes of Bone Marrow Suppression
The reasons for aplastic anemia vary, but often involve the immune system attacking the bone marrow. Environmental factors, genetic predispositions, and exposure to certain chemicals or drugs can start this immune response. Sometimes, the cause is unknown, making diagnosis and treatment hard.
Clinical Presentation and Diagnostic Criteria
People with aplastic anemia often feel tired, get infections easily, and bruise or bleed a lot. Doctors use blood tests, bone marrow biopsies, and rule out other causes to diagnose it. Early diagnosis is key for starting the right treatment and improving chances of recovery.
Treatment Approaches: From Supportive Care to Transplantation
Treatment for aplastic anemia depends on how severe it is and the patient’s health. Supportive care, like blood transfusions and antibiotics, helps manage symptoms. For more serious cases, immunosuppressive therapy may be used to calm the immune system’s attack on the bone marrow. In some cases, bone marrow transplantation can be a cure by replacing the damaged marrow with healthy cells from a donor.
Dealing with aplastic anemia can be tough, but the right treatment can greatly improve a patient’s condition. It’s important for patients to work closely with their healthcare team to find the best treatment plan.
Fanconi Anemia: Hereditary Bone Marrow Failure Syndrome
Fanconi anemia is a rare genetic disorder that affects the bone marrow. It leads to bone marrow failure and raises the risk of cancer. This makes it essential to manage it thoroughly.
Genetic Basis and Inheritance Patterns
Fanconi anemia is caused by DNA repair gene mutations. It is inherited in an autosomal recessive pattern. This means a person needs two copies of the mutated gene to have the condition.
Finding the genetic defect is key for diagnosis and understanding family risks. Genetic counseling is advised for families with Fanconi anemia.
Physical Manifestations and Hematologic Abnormalities
People with Fanconi anemia may have short stature, skin color changes, and birth defects. Hematologic problems are common, like aplastic anemia and low blood cells.
The bone marrow failure leads to infections, bleeding, and the need for blood transfusions.
Comprehensive Management and Cancer Surveillance
Managing Fanconi anemia requires a team effort from doctors and specialists. Supportive care, like blood transfusions, is used. Also, treatments like stem cell transplants are considered.
| Management Approach | Description | Benefits |
| Supportive Care | Blood transfusions, antibiotics, and other measures to manage symptoms | Improves quality of life, reduces complications |
| Hematopoietic Stem Cell Transplantation | Curative treatment replacing the defective bone marrow | Potential cure for bone marrow failure |
| Cancer Surveillance | Regular monitoring for cancer development | Early detection and treatment of cancers |
It’s vital to watch for cancer because of the high risk. We stress the need for a detailed care plan for each person.
Myelodysplastic Syndromes (MDS): Precancerous Bone Marrow Disorders
MDS is a group of disorders where the bone marrow doesn’t work right. This leads to blood cells that don’t function well. It also raises the chance of getting acute myeloid leukemia (AML).
Classification Systems and Risk Assessment
There are different ways to classify MDS. The World Health Organization (WHO) and the International Prognostic Scoring System (IPSS) are two main ones. The WHO looks at cell shapes to diagnose MDS. The IPSS assesses risk based on blast cells, chromosome changes, and blood counts.
Knowing the risk level is key in treating MDS. The IPSS puts patients into low, intermediate, or high risk groups. This helps doctors decide the best treatment plan.
Key factors in MDS risk assessment include:
- Cytogenetic abnormalities
- Percentage of bone marrow blasts
- Number of cytopenias
Diagnostic Workup and Cytogenetic Analysis
Diagnosing MDS requires a detailed process. It includes:
- Complete blood count (CBC) to check for blood shortages
- Bone marrow biopsy to look at cell shapes and count
- Cytogenetic analysis to find chromosome problems
- Molecular studies to find specific mutations
Cytogenetic analysis is very important in MDS diagnosis. It gives clues about the disease’s severity and possible treatments. Common problems include missing parts of chromosomes 5 and 7, and extra chromosome 8.
“Cytogenetic analysis is essential for risk stratification and treatment planning in MDS patients.” – Hematology Expert
Treatment Options Based on Risk Stratification
Treatment for MDS varies based on the patient’s risk level, age, and health. For those at lower risk, the goal is to improve life quality and reduce blood transfusions. Treatment options include:
- Supportive care with blood transfusions
- Immunosuppressive therapy
- Lenalidomide for patients with del(5q) abnormality
- Hypomethylating agents like azacitidine and decitabine
For those at higher risk, the aim is to change the disease’s course and possibly cure it. Treatment options include strong chemotherapy and stem cell transplants.
Every patient with MDS is unique. So, treatment must be tailored to their specific needs, health, and wishes.
Polycythemia Vera: Myeloproliferative Bone Marrow Blood Disease
Polycythemia vera is a complex condition. It involves the JAK2 mutation, which affects how the body makes blood cells. This leads to too many red and white blood cells and platelets.
JAK2 Mutation and Disease Pathophysiology
The JAK2 V617F mutation makes the JAK-STAT pathway work too much. This causes cells to grow and live longer than they should. Most people with polycythemia vera have this mutation.
This mutation makes the bone marrow produce too many blood cells. This can cause blood to get too thick. This can lead to blood clots and other problems.
Symptoms, Complications, and Thrombotic Risk
People with polycythemia vera might feel dizzy, have headaches, or itch after taking a warm bath. The thick blood can also harm the heart and blood vessels.
One big worry is blood clots. Older age, past blood clots, and heart disease risk factors all raise this risk.
| Risk Factor | Description | Impact on Thrombotic Risk |
| Age >60 years | Advanced age is associated with increased thrombotic risk. | High |
| History of Thrombosis | Previous thrombotic events increase the risk of future events. | High |
| Cardiovascular Risk Factors | Presence of hypertension, diabetes, and hyperlipidemia. | Moderate to High |
Therapeutic Strategies and Disease Monitoring
Treating polycythemia vera aims to lower blood clot risk and ease symptoms. Doctors might use phlebotomy to reduce red blood cells. They might also give medications like hydroxyurea to slow blood cell production. Low-dose aspirin is used to prevent blood clots.
It’s important to keep an eye on blood counts and watch for blood clots and disease growth. Treatment plans are adjusted based on how the patient responds and their risk factors.
“The management of polycythemia vera requires a complete plan. This includes regular phlebotomy, medicine, and careful watching to lower blood clot risk.”
Understanding polycythemia vera and using the right treatments can help patients live better lives. It’s all about improving their health and happiness.
Essential Thrombocythemia: Abnormal Platelet Production Disorder
In essential thrombocythemia, the bone marrow makes too many platelets. This can cause serious problems. It’s a type of myeloproliferative neoplasm, affecting how blood cells are made.
Molecular Pathogenesis and Clonal Evolution
Genetic mutations drive essential thrombocythemia. These mutations make too many platelets. The JAK2, MPL, and CALR genes are often involved.
Understanding the complex genetics is key. It helps us find better treatments.
Clinical Features and Vascular Complications
Patients often have high platelet counts. This can cause blood clots and other problems. Symptoms include headaches and dizziness.
Vascular complications are a big worry. They can be very dangerous. We need to manage patients carefully to avoid these risks.
Risk-Adapted Treatment Approaches
Treatment plans vary based on the patient’s risk. Low-risk patients might just need antiplatelet therapy and regular checks. High-risk patients might need stronger treatments to lower platelet counts.
It’s important for patients to work with their doctors.
Primary Myelofibrosis: Progressive Bone Marrow Scarring
Bone marrow scarring, or primary myelofibrosis, is a serious condition that affects patients’ lives. It causes the bone marrow to scar, making it hard to produce blood cells.
Fibrotic Transformation and Pathophysiology
The disease starts with genetic changes that make fibroblasts grow and deposit proteins. JAK2, MPL, and CALR mutations play a big role in this process.
As the disease gets worse, the bone marrow can’t make blood cells well. This leads to anemia, fatigue, and other problems that hurt patients’ health.
Symptom Burden and Quality of Life
Patients with primary myelofibrosis face many symptoms like fatigue, night sweats, and bone pain. These symptoms can really affect their health and mood.
Quality of life is very important when treating this disease. Doctors need to help with both physical and emotional issues to care for patients fully.
Contemporary Treatment Paradigms
Treatment plans for primary myelofibrosis vary based on each patient’s needs. JAK inhibitors are a key treatment that helps reduce symptoms and improve life quality.
- Supportive care, like blood transfusions, is also important in managing the disease.
- In some cases, allogeneic stem cell transplantation might be an option, aiming for a cure.
Sideroblastic Anemia: Iron Utilization Disorders in Bone Marrow
Sideroblastic anemia is a disorder of iron metabolism in the bone marrow. It presents unique challenges in diagnosis and treatment. This condition is caused by iron buildup in mitochondria, leading to poor hemoglobin production and anemia.
Congenital vs. Acquired Forms
Sideroblastic anemia can be either congenital or acquired. The congenital form is linked to genetic mutations, like those affecting the ALAS2 gene. Acquired forms can be caused by myelodysplastic syndromes, certain medications, and alcohol abuse.
Knowing the cause is key to choosing the right treatment. This knowledge helps doctors manage the condition effectively, whether it’s congenital or acquired.
Diagnostic Features and Ring Sideroblasts
Diagnosing sideroblastic anemia involves finding ring sideroblasts in the bone marrow. These are erythroblasts with iron-loaded mitochondria visible as a ring around the nucleus. The presence of ring sideroblasts is confirmed through bone marrow biopsy and Prussian blue staining.
We use various tools to diagnose sideroblastic anemia. Finding ring sideroblasts helps in understanding the condition’s severity.
Treatment Strategies and Nutritional Considerations
Treatment for sideroblastic anemia depends on the cause. It may include blood transfusions, iron chelation therapy, and pyridoxine supplementation. Nutritional considerations are also important, as deficiencies can worsen the condition.
A complete treatment plan is essential. It should address the hematological, nutritional, and overall well-being of the patient.
| Treatment Approach | Description | Applicability |
| Blood Transfusions | Regular transfusions to maintain adequate hemoglobin levels | Transfusion-dependent patients |
| Iron Chelation Therapy | Treatment to reduce iron overload | Patients with significant iron overload |
| Pyridoxine Supplementation | Vitamin B6 supplementation to potentially improve erythropoiesis | Patients with pyridoxine-responsive sideroblastic anemia |
Understanding sideroblastic anemia’s different forms, diagnostic features, and treatments is key. This knowledge helps us provide complete care for those affected by this complex condition.
Hemophagocytic Lymphohistiocytosis (HLH): Immune Dysregulation in Bone Marrow
Hemophagocytic Lymphohistiocytosis (HLH) is a rare and dangerous condition. It happens when the immune system can’t stop its response to a stimulus. This leads to too much inflammation, causing damage to tissues and organs.
Pathogenesis: Familial vs. Secondary HLH
HLH comes in two types: familial (primary) and secondary. Familial HLH is caused by genetic mutations that affect immune cells. This makes it hard for the immune system to control itself. Secondary HLH is triggered by infections, cancers, or autoimmune diseases. It can happen to anyone, not just those with a family history.
The disease is caused by a mix of immune cells and cytokines. It’s marked by too much inflammation, thanks to cytokines like IFN-γ and TNF-α. This inflammation causes the damage seen in HLH.
Diagnostic Challenges and HLH-2004 Criteria
Diagnosing HLH is hard because its symptoms are similar to other diseases. The HLH-2004 criteria were set by the Histiocyte Society. They include fever, big spleen, low blood cells, high triglycerides, and bone marrow changes.
- Fever
- Splenomegaly
- Cytopenias affecting at least two cell lines
- Hypertriglyceridemia or hypofibrinogenemia
- Hemophagocytosis in bone marrow, spleen, or lymph nodes
- Low or absent NK-cell activity
- Ferritin levels ≥ 500 ng/mL
- Elevated soluble CD25 (sIL-2Rα) levels
To be diagnosed with HLH, a patient must meet five of these eight criteria.
Therapeutic Protocols and Emerging Treatments
Treating HLH involves several steps to control inflammation and find the cause. First, doctors use corticosteroids and immunoglobulins. For severe cases, they add more drugs. For some, a bone marrow transplant is the best option.
New treatments for HLH are being tested. For example, ruxolitinib, a drug that targets certain immune cells, shows promise. It could help reduce inflammation and improve patient outcomes.
“The management of HLH requires a prompt and accurate diagnosis, followed by an appropriate therapeutic intervention. Emerging treatments offer new hope for improving patient outcomes in this challenging condition.”
As we learn more about HLH, we’ll see better treatments. This will help patients with this serious condition live better lives.
Conclusion: Advances in Diagnosis and Treatment of Bone Marrow Disorders
Recent years have brought big changes in how we understand and treat bone marrow disorders. This has led to better results for patients. We’ve looked at many bone marrow diseases, like aplastic anemia and myeloproliferative neoplasms.
Diagnosing and treating these conditions has gotten much better. New genetic tests and treatments have made a big difference. For example, finding specific mutations helps doctors diagnose more accurately. And new therapies have made treatments more effective.
We’ve seen how complex bone marrow disorders are. It’s clear that a team effort is needed to care for patients. Healthcare providers must keep up with the latest in diagnosis and treatment to help patients the best they can.
As we learn more about bone marrow, we’ll see even more progress in treating these disorders. This will lead to better health outcomes and a higher quality of life for patients.
FAQ
What is bone marrow and its role in blood cell production?
Bone marrow is the spongy tissue inside some bones, like the hips and thighbones. It makes blood cells, including red blood cells, white blood cells, and platelets.
What are bone marrow disorders?
Bone marrow disorders are conditions that affect the bone marrow’s ability to make healthy blood cells. Examples include aplastic anemia, Fanconi anemia, myelodysplastic syndromes, and myeloproliferative neoplasms.
What are the common symptoms of bone marrow dysfunction?
Symptoms include anemia, infections, bleeding disorders, fatigue, and shortness of breath. These depend on the specific disorder.
Does abnormal bone marrow mean cancer?
Not always. Some disorders, like myelodysplastic syndromes, can be precancerous or turn into cancer. But others, like aplastic anemia, are not cancerous. The type of disorder depends on its cause and characteristics.
What is the difference between myelodysplastic syndromes and myeloproliferative neoplasms?
Myelodysplastic syndromes mean the bone marrow can’t make healthy blood cells and may turn into leukemia. Myeloproliferative neoplasms are when the bone marrow makes too many blood cells, leading to problems like thrombosis.
How are bone marrow disorders diagnosed?
Doctors use blood tests, bone marrow biopsy, and genetic testing to diagnose. These tests help find specific mutations or abnormalities.
What are the treatment options for bone marrow disorders?
Treatment varies by disorder. It can include supportive care, medications, immunosuppressive therapy, and sometimes bone marrow transplantation.
Can bone marrow disorders be cured?
Cure chances vary by disorder. Some, like aplastic anemia, can be treated with bone marrow transplantation. Others need ongoing management to control symptoms and prevent complications.
What is the role of genetic testing in diagnosing bone marrow disorders?
Genetic testing finds specific mutations linked to certain disorders, like the JAK2 mutation in polycythemia vera. It helps in diagnosis and treatment planning.
Are there non-cancerous bone marrow disorders?
Yes, aplastic anemia and sideroblastic anemia are non-cancerous disorders that affect blood cell production.
How do bone marrow disorders affect quality of life?
The impact on quality of life varies by disorder and severity. Symptoms like fatigue, infections, and bleeding can affect daily life. But, the right treatment and management can improve quality of life.
References
- Killick, S. B., Bown, N., Cavenagh, J., Dokal, I., Foukaneli, T., Hill, A., … & Marsh, J. C. W. (2021). Guidelines for the diagnosis and management of adult aplastic anaemia. British Journal of Haematology, *172*(2), 187-207. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7988580/