Last Updated on November 17, 2025 by Ugurkan Demir
It’s key for patients and doctors to know the medical terms for blood clots and clotting. At Liv Hospital, we stress the need for clear terms like ‘thrombus’ for a blood clot and ‘thrombosis’ for the clotting process. Understanding the medical terminology for blood clot is essential for effective communication and treatment.
When a blood vessel gets hurt, the body makes a clot to stop blood loss. This happens through a process called
We will look at 12 key terms about blood clots and clotting. We’ll dive into what they mean and why they matter in medical practice. Knowing these terms is important for spotting and treating problems.
Key Takeaways
- Understanding thrombus and thrombosis is key for patients and doctors.
- The body’s injury response includes coagulation to stop blood loss.
- Liv Hospital focuses on accurate medical terminology for better care.
- Knowing blood clot terms helps in diagnosing and treating.
- We will explore 12 essential terms related to blood clots and clotting.
The Science Behind Blood Clotting
When a blood vessel gets damaged, the body starts a complex process to stop too much blood loss. This process is key to keeping the body balanced between bleeding and clotting.
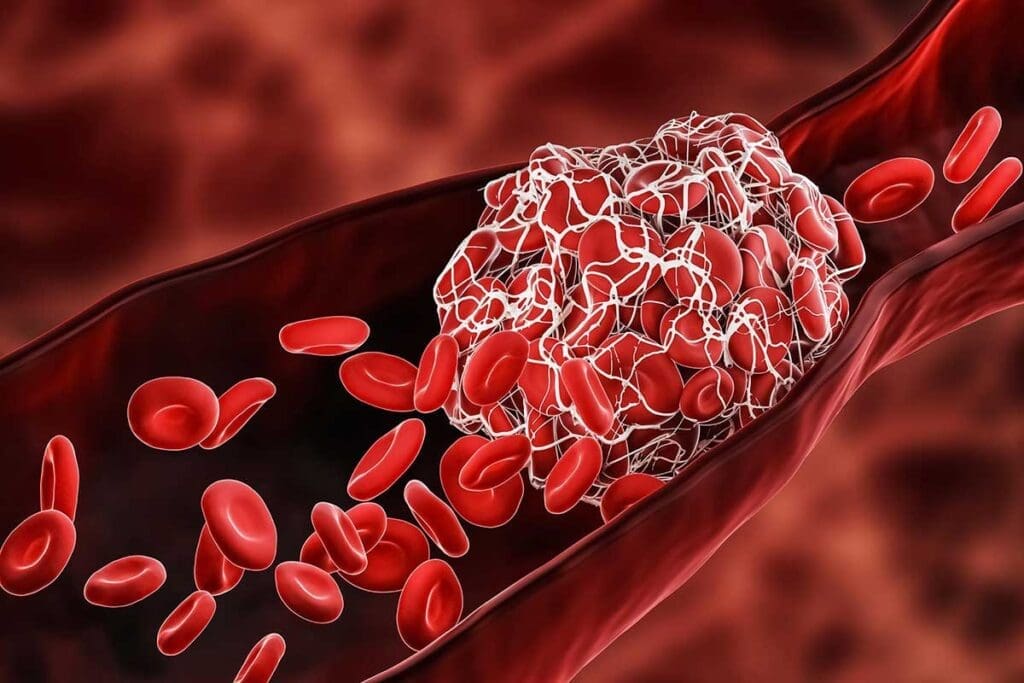
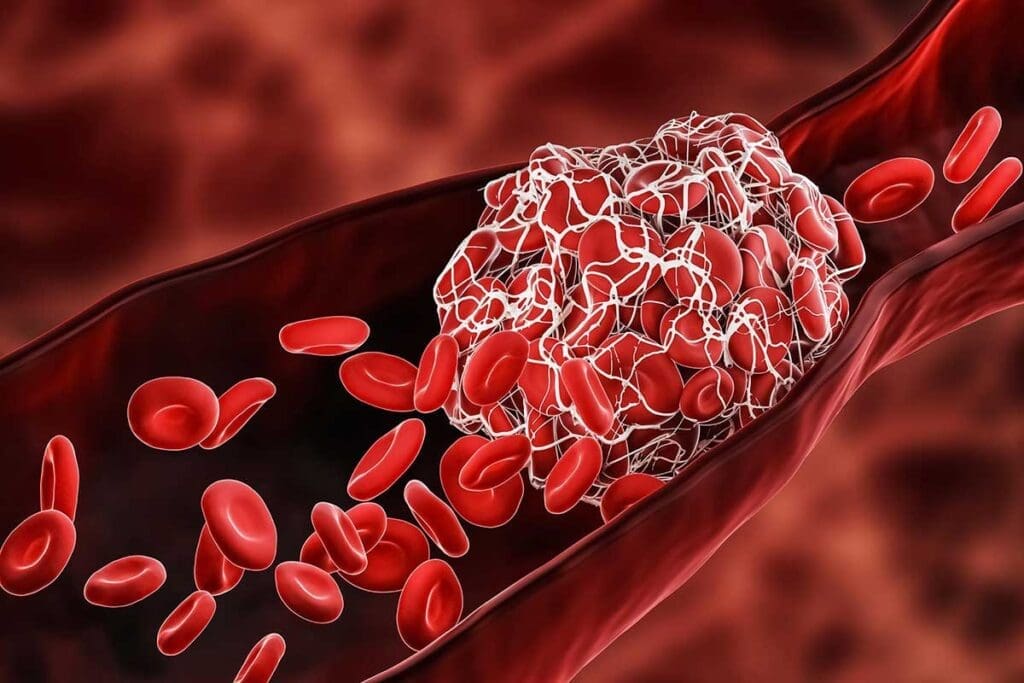
Blood clotting, or coagulation, involves many parts like platelets, clotting factors, and fibrin. We’ll see how these work together to make a blood clot, known as a thrombus. Knowing about blood clotting is important for diagnosing and treating clotting problems.
The Physiological Purpose of Clotting
The main goal of blood clotting is to stop too much bleeding when a blood vessel is hurt. This is essential for keeping the blood vessels strong and helping the body heal from injuries. A blood clot seals the injured vessel, starting the healing process.
When Normal Clotting Becomes Pathological
While clotting is needed, it can be harmful if it goes wrong. Dysregulated clotting can cause dangerous clots that block blood flow. This is called thrombosis and can lead to heart attacks, strokes, and deep vein thrombosis. Knowing when clotting goes wrong is key to spotting risks and treating them.
At Liv Hospital, we focus on finding the right balance between preventing bleeding and clotting. By understanding blood clotting and its mechanisms, we can better treat coagulation disorders.
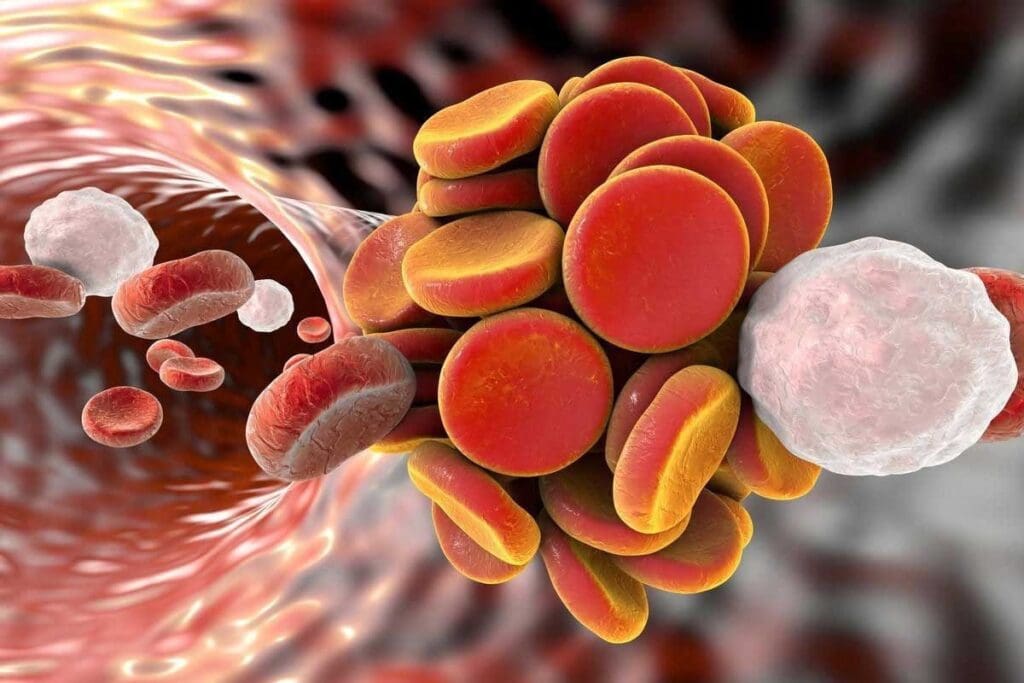
Medical Terminology for Blood Clot: Thrombus Explained
A blood clot that forms inside a blood vessel is called a thrombus. This term is key to understanding heart and blood vessel problems. It includes deep vein thrombosis and stroke.
Definition and Etymology of Thrombus
A thrombus is a blood clot stuck to a blood vessel wall. The word “thrombus” comes from the Greek for “clot” or “curd.” It shows the clot’s coagulated blood nature. Knowing what a thrombus is helps doctors diagnose and treat blood clot issues.
Formation Mechanism of a Thrombus
Creating a thrombus involves platelets, clotting factors, and the vessel wall working together. It can start from injury, blood flow changes, or clotting imbalances. A thrombus can block the blood vessel fully or just partly.
Common Sites for Thrombus Development
Thrombi can form in any blood vessel, like arteries and veins. They often happen where blood flow is turbulent or the vessel is injured. For example, deep vein thrombosis usually occurs in the legs. Arterial thrombi can block heart or brain blood flow, causing heart attacks or strokes.
Knowing the term “thrombus” is important for grasping blood clot issues. It helps in finding the right treatments for these problems.
Coagulation: The Biochemical Process of Blood Clotting
The coagulation cascade is a series of biochemical reactions that lead to blood clotting. This is key for keeping blood from flowing too much. We’ll explore the details of this process, including the important factors and how they’re checked in a medical setting.
The Coagulation Cascade Explained
The coagulation cascade has two main paths: the intrinsic and extrinsic pathways. They both end up in a common pathway. The intrinsic pathway starts with damage inside the blood vessels. The extrinsic pathway is triggered by damage outside the body that releases tissue factor.
A leading hematologist says, “The coagulation cascade is a complex interplay of various factors that ultimately leads to the formation of a fibrin clot.”
“The coagulation cascade is not just a series of biochemical reactions; it’s a highly regulated process that prevents excessive bleeding or clotting.”
Essential Clotting Factors and Their Functions
Clotting factors are proteins in blood that are vital for clotting. There are 13 clotting factors, each with a Roman numeral. Key factors include fibrinogen (Factor I), prothrombin (Factor II), and Factor X.
| Clotting Factor | Function |
| Fibrinogen (Factor I) | Precursor to fibrin, which forms the clot |
| Prothrombin (Factor II) | Precursor to thrombin, which converts fibrinogen to fibrin |
| Factor X | Converges the intrinsic and extrinsic pathways into the common pathway |
Laboratory Tests for Coagulation Assessment
To check a patient’s coagulation status, several lab tests are used. The most common are prothrombin time (PT) and activated partial thromboplastin time (aPTT).
- PT evaluates the extrinsic and common pathways.
- aPTT assesses the intrinsic and common pathways.
These tests are vital for diagnosing coagulopathies and monitoring anticoagulant therapy. They help ensure patients get the right treatment to avoid bleeding or clotting problems.
Thrombosis: Pathological Blood Clot Formation
Blood clotting inside a blood vessel is a complex issue. At Liv Hospital, we focus on understanding thrombosis to help our patients. This knowledge is key to giving them the best care.
Differentiating Arterial and Venous Thrombosis
Thrombosis can happen in arteries and veins, each with its own causes and effects. Arterial thrombosis is linked to plaque buildup in arteries. On the other hand, venous thrombosis is often caused by immobility, clotting disorders, and cancer.
Knowing these differences helps us diagnose and treat better. We use advanced tests to figure out the type of thrombosis. Then, we create a treatment plan that fits each patient’s needs.
Risk Factors and Predisposing Conditions
Many factors can lead to thrombosis. These include genetic conditions, lifestyle choices like smoking and obesity, and health issues like cancer and heart disease. Identifying these risk factors is key to preventing blood clots.
- Genetic clotting disorders
- Prolonged immobility
- Cancer and its treatment
- Smoking and obesity
Clinical Manifestations of Thrombotic Events
The symptoms of thrombosis depend on where and how big the clot is. Arterial thrombosis can cause sudden limb ischemia, heart attacks, or strokes. Venous thrombosis usually shows up as swelling, pain, and warmth in the affected limb.
It’s important to recognize these symptoms quickly. We teach our patients about the signs of thrombosis. We stress the need to seek medical help right away if they notice any of these symptoms.
Embolus: When Blood Clots Travel
Emboli are clots or particles that move from one part of the body to another. They can cause serious conditions. Knowing about emboli helps doctors treat these problems well.
Distinguishing Emboli from Thrombi
Emboli and thrombi are both blood clots, but they differ. A thrombus forms in a blood vessel. An embolus is a clot or particle that travels through the blood. This difference is important because treating them differently can affect outcomes.
For example, a clot in the leg’s deep veins is a DVT. If it breaks loose, it becomes an embolus. This can go to the lungs, causing a pulmonary embolism, or to the brain, leading to a stroke.
Common Embolic Sources and Pathways
Emboli can come from many places, like DVT, heart clots, or even air bubbles. Where an embolus goes depends on where it starts. For instance, a clot from the heart’s left side can go anywhere, like the brain or kidneys, causing damage.
There are main areas where emboli can start:
- Venous thromboembolism (VTE), which includes DVT and pulmonary embolism
- Cardiac sources, such as atrial fibrillation or post-myocardial infarction thrombi
- Arterial sources, including aneurysms or atherosclerotic plaques
Clinical Consequences of Embolization
The effects of an embolism can be serious and vary by location. For example, a lung embolism can cause heart failure. A brain embolism can lead to a stroke. The symptoms can range from mild to severe.
Here’s what can happen when an embolus lodges in different areas:
| Location | Consequence | Symptoms |
| Lungs | Pulmonary Embolism | Dyspnea, Chest Pain, Tachypnea |
| Brain | Ischemic Stroke | Weakness, Speech Disturbances, Vision Changes |
| Limbs | Acute Limb Ischemia | Pain, Pallor, Pulselessness |
In summary, knowing about emboli and their effects is key for doctors. Quick diagnosis and treatment can greatly help patients.
Hemostasis: The Body’s Bleeding Control Mechanism
When an injury happens, the body starts hemostasis to stop too much blood loss. This complex process has several steps. It aims to stop bleeding while keeping blood flowing.
Primary Hemostasis and Platelet Function
Primary hemostasis is the first step after an injury. Platelets are key here. They stick to the injury site, get activated, and form a plug. This plug helps stop the bleeding.
Secondary Hemostasis and Fibrin Formation
Secondary hemostasis is about the coagulation cascade. This series of reactions makes fibrin. Fibrin strengthens the plug, making the clot more stable. This is important for fixing the injured vessel.
Fibrinolysis: The Clot Breakdown Process
Fibrinolysis breaks down clots when they’re no longer needed. Plasmin, a key enzyme, breaks down fibrin. This process is vital for keeping blood flowing and preventing clots.
In summary, hemostasis is a delicate balance. It stops bleeding while keeping blood flowing. Knowing about primary and secondary hemostasis and fibrinolysis helps us understand how the body responds to injury.
Platelets and Plasma Proteins: Key Players in Clotting
Platelets and plasma proteins are key to stopping bleeding after an injury. They work together to form a blood clot. This process is complex and involves many steps.
Platelet Structure and Activation
Platelets are small cells that start the clotting process. When a blood vessel is injured, platelets stick to the damage. They then release signals that bring more platelets.
This creates a platelet plug that seals the injury. Recent studies show how important platelet activation is in clotting.
Fibrinogen and Other Crucial Plasma Proteins
Fibrinogen is a plasma protein vital for clotting. It turns into fibrin, which makes a strong clot. Other proteins like prothrombin and factors VIII and IX are also key.
| Plasma Protein | Function in Coagulation |
| Fibrinogen | Converted to fibrin to form a stable clot |
| Prothrombin | Converted to thrombin to facilitate clot formation |
| Factor VIII | Essential for the intrinsic pathway of coagulation |
The Role of Calcium in Coagulation
Calcium ions are vital for clotting. They help clotting factors work right and bind to surfaces. Without enough calcium, clotting fails.
Platelets, plasma proteins, and calcium ions are essential for stopping bleeding. Knowing how they work together helps us understand blood clotting better.
Thromboembolism: Complications of Traveling Clots
When a clot breaks loose, it can cause a serious condition called thromboembolism. This can lead to serious health problems, depending on where the clot goes. At Liv Hospital, we take thromboembolism very seriously and its effects on health.
Pulmonary Embolism: Causes and Consequences
A pulmonary embolism happens when a clot blocks a lung artery. This can be very dangerous. It often starts with a clot in the deep veins of the legs. We work to prevent this by identifying at-risk patients and taking steps to stop it.
Cerebral Thromboembolism and Stroke
Cerebral thromboembolism occurs when a clot reaches the brain, causing a stroke. This can lead to serious brain damage or even death. It’s important to know the risks and symptoms to act quickly.
Prevention Strategies and Treatment Options
To prevent thromboembolism, we look for patients at risk and use anticoagulant medications. We also use mechanical methods in some cases. Treatment depends on where and how severe the clot is, from medication to emergency procedures.
| Type of Thromboembolism | Causes | Consequences | Prevention/Treatment |
| Pulmonary Embolism | Often related to DVT | Life-threatening blockage in the lungs | Anticoagulation, thrombolysis |
| Cerebral Thromboembolism | An embolus traveling to the brain | Stroke, neurological damage | Anticoagulation, thrombolysis, mechanical thrombectomy |
Coagulopathy: Disorders of the Clotting System
Coagulopathy is a group of disorders that affect how the body clots. This can lead to too much bleeding or clots forming where they shouldn’t. These issues can really impact a person’s life and need careful handling.
Hereditary Coagulation Disorders
Hereditary coagulation disorders are genetic and affect clotting factors. Hemophilia A and B are well-known, caused by a lack of factors VIII and IX. Von Willebrand disease also affects clotting, impacting platelet adhesion and clot formation.
| Disorder | Deficiency | Clinical Manifestation |
| Hemophilia A | Factor VIII | Excessive bleeding, joint pain |
| Hemophilia B | Factor IX | Excessive bleeding, joint pain |
| Von Willebrand Disease | Von Willebrand Factor | Bleeding after injury, easy bruising |
Acquired Clotting Abnormalities
Acquired clotting issues can come from liver disease, vitamin K deficiency, or anticoagulant use. Liver problems can lower clotting factor production. Vitamin K deficiency affects how these factors work. Anticoagulants, meant to prevent clots, can increase bleeding risk.
Diagnostic Approaches and Management
Diagnosing coagulopathy involves clinical checks and lab tests like PT, aPTT, and specific factor assays. Treatment depends on the cause. It might include replacing clotting factors for hereditary disorders, fixing underlying causes for acquired ones, and monitoring anticoagulant use.
Managing coagulopathy needs a detailed plan, considering the disorder, its severity, and the patient’s health. Accurate diagnosis and tailored treatment can greatly improve patient outcomes.
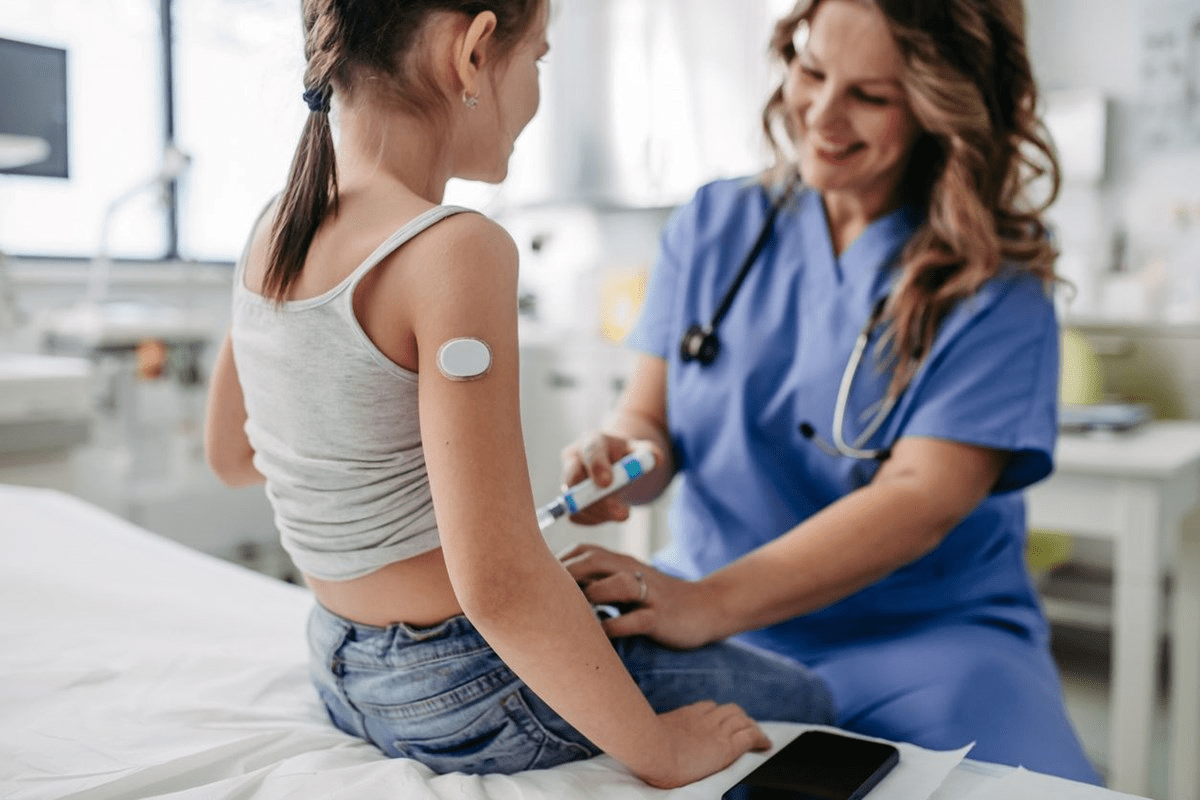
Therapeutic Interventions for Blood Clots
Managing blood clots requires different treatments. These aim to stop new clots, dissolve old ones, and handle any problems that might arise. It’s key for those at risk of blood clots.
Anticoagulant Medications and Mechanisms
Anticoagulants are vital in fighting blood clots. They block the coagulation process, stopping new clots or making old ones smaller. Warfarin and DOACs like rivaroxaban and apixaban are common types. They target specific parts of the clotting process.
Warfarin needs regular INR checks to keep it effective. DOACs offer a steady effect without constant monitoring.
“The introduction of DOACs has revolutionized anticoagulation therapy, making it easier and safer than traditional warfarin.”
— Cardiologist
| Anticoagulant | Mechanism of Action | Monitoring Requirements |
| Warfarin | Vitamin K antagonist | Regular INR monitoring |
| Rivaroxaban | Direct Factor Xa inhibitor | No routine monitoring |
| Apixaban | Direct Factor Xa inhibitor | No routine monitoring |
Thrombolytic Agents for Clot Dissolution
Thrombolytics are used to break up clots. They work by activating plasminogen, which breaks down fibrin clots. This therapy is used in acute stroke and massive pulmonary embolism to quickly restore blood flow.
Alteplase is a common thrombolytic given intravenously quickly after symptoms start to work well.
Monitoring Therapy and Managing Complications
Keeping an eye on treatment and managing side effects is vital. It’s important to check coagulation, kidney function, and watch for bleeding or clotting signs.
Dealing with side effects might mean changing doses, switching meds, or finding ways to lower bleeding risks.
Knowing how these treatments work helps doctors improve patient care for blood clots.
Conclusion: Advancing Our Understanding of Blood Clotting
Understanding blood clotting is key for healthcare workers and patients. The complex coagulation and thrombosis processes need a detailed approach for diagnosis and treatment.
At Liv Hospital, we keep up with the latest in blood clotting research. Our commitment to top-notch care shows in our use of the newest medical terms and proven practices. We tackle thrombosis and coagulopathy with the latest treatments.
Learning about blood clotting helps us better care for those affected. Managing thrombosis and coagulopathy well means knowing the science behind them. It also means using the newest treatments, like anticoagulants and thrombolytics.
As we learn more about blood clotting, we can give better care to our patients. Our aim is to offer complete, world-class medical care that meets each patient’s specific needs.
FAQ
What is the medical term for a blood clot?
The term for a blood clot is ‘thrombus’. It’s a clot stuck to a blood vessel wall.
What is thrombosis?
Thrombosis is when a blood clot forms inside a blood vessel. It can happen in arteries or veins. Each has its own risks and effects.
What is the coagulation cascade?
The coagulation cascade is a complex process. It involves many clotting factors working together. This leads to fibrin formation and a stable clot.
What is the difference between an embolus and a thrombus?
An embolus is a clot or particle that travels in the blood. It can block a vital area. A thrombus is a clot stuck to a blood vessel wall.
What is hemostasis?
Hemostasis is a process to stop bleeding after an injury. It has primary and secondary steps. The first involves a platelet plug. The second is the coagulation cascade to stabilize the clot.
What is thromboembolism?
Thromboembolism is a serious condition. It happens when a clot breaks loose and travels. It can block areas like the lungs or brain.
What is coagulopathy?
Coagulopathy is a range of disorders affecting the clotting system. It can cause too much bleeding or clotting. Understanding it is key to diagnosis and treatment.
What are anticoagulant medications used for?
Anticoagulant medications prevent new clots or stop existing ones from growing. They work in different ways to stop clotting. They’re used to treat and prevent blood clots.
What is fibrinolysis?
Fibrinolysis is the process of breaking down clots. It’s important for restoring blood flow. It ensures clots are dissolved when they’re no longer needed.
What is the role of platelets in blood clotting?
Platelets are key to blood clotting. They’re activated by injury, releasing signals for more platelets. They help form a plug and stabilize the clot with fibrin.
What is the significance of understanding medical terminology related to blood clots and clotting?
Knowing medical terms for blood clots is vital. It helps in diagnosing and treating clotting issues. It ensures patients get the best care.
What are some common laboratory tests used to assess coagulation status?
Tests like prothrombin time (PT) and activated partial thromboplastin time (aPTT) check coagulation status. They help guide treatment decisions.
References:
- McLendon, K., & Willis, J. (2023). Deep venous thrombosis risk factors. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470215/
- Heit, J. A. (2015). Epidemiology of venous thromboembolism. Nature Reviews Cardiology, 12(8), 464–474. https://www.nature.com/articles/nrcardio.2015.83