Last Updated on November 17, 2025 by Ugurkan Demir
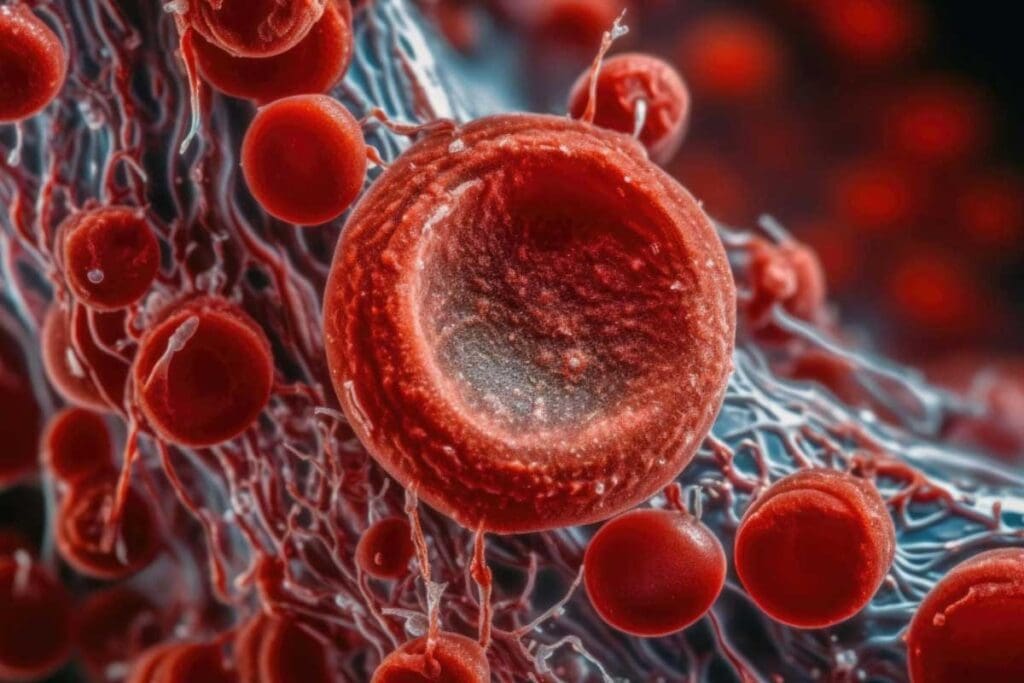
Pregnancy brings many changes to the body, including a higher risk of blood clots. The CDC says pregnancy raises this risk by five times. It’s very important for pregnant women to know the signs and dangers of blood clots.

At Liv Hospital, we focus on giving full care to pregnant people, including those with thromboembolic disorders. We help every step of the way, from finding blood clots early to using the latest ways to prevent them.
Key Takeaways
- Pregnancy increases the risk of developing blood clots fivefold.
- Blood clots can pose a significant risk to both mother and baby.
- Understanding symptoms and risks is key for early detection.
- Advanced prevention strategies can greatly lower risks.
- Comprehensive care is vital for managing pregnancy-related blood clots.
- Expectant mothers should know the risks and symptoms.
Understanding Blood Clots While Pregnant
Pregnant women face a higher risk of blood clots than non-pregnant women. Pregnancy brings many changes that raise this risk.
We will explore how pregnancy affects blood clot risk. We will also look at the common types of blood clots that can happen.
Fact 1: Pregnancy Increases Blood Clot Risk by Five Times
Pregnancy changes the body in ways that increase blood clot risk. Pregnant women are five times more likely to develop blood clots than non-pregnant women. These changes include blood clotting factors, venous pressure, and blood flow.
Fact 2: Common Types of Blood Clots in Pregnancy
The most common blood clots in pregnancy are deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT occurs when a blood clot forms in the deep veins, typically in the legs. If it breaks loose, it can travel to the lungs, causing a life-threatening pulmonary embolism.

The National Blood Clot Alliance warns that blood clots during pregnancy are dangerous. They can harm both the mother and the baby. A blood clot in the lungs is a leading cause of pregnancy-related death in the U.S.
Recognizing the Warning Signs of Blood Clots During Pregnancy
Knowing the signs of blood clots during pregnancy is key to avoiding serious problems. Pregnancy changes the body in ways that raise the risk of blood clots. Spotting these signs early can help get quick medical help.
Critical Symptoms That Require Immediate Attention
Blood clots in pregnancy often show up as Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE). DVT symptoms include swelling, pain, or tenderness in one leg, warmth, or redness of the skin. PE symptoms are more serious and can include trouble breathing, chest pain, and coughing up blood.
The American Society of Hematology says DVT symptoms are swelling, pain, and warmth in one leg. For PE, look out for trouble breathing, chest pain, and coughing up blood.
When to Seek Emergency Medical Care
If you have persistent pain, swelling, redness, or warmth in one leg, or chest pain, shortness of breath, or coughing up blood, get help right away. These signs could mean a blood clot and need quick checking.
| Condition | Symptoms | Action |
| Deep Vein Thrombosis (DVT) | Swelling, pain, warmth, redness in one leg | Seek medical care if symptoms persist |
| Pulmonary Embolism (PE) | Difficulty breathing, chest pain, coughing up blood | Seek emergency medical care immediately |
Pregnant people need to watch their health closely and know the signs of blood clots. If unsure, always talk to a healthcare provider.
Key Risk Factors for Blood Clots While Pregnant
Blood clots during pregnancy can be caused by several factors. These include pre-existing conditions and pregnancy-specific issues. Knowing these risks is key to managing them.
Pre-existing Conditions That Increase Risk
Some health issues before pregnancy can raise the risk of blood clots. These include:
- Previous history of blood clots: Women who have had blood clots before are more likely to have them again during pregnancy.
- Inherited blood clotting disorders: Conditions like Factor V Leiden thrombophilia and Prothrombin G20210A mutation can increase clotting risk.
- Obesity: Being overweight can put more pressure on veins, raising the risk of clotting.
- Age over 35: Women over 35 are at a higher risk of blood clots during pregnancy.
Pregnancy-Specific Risk Factors
Pregnancy itself brings unique risks for blood clots. These include:
- C-section delivery: Cesarean sections can increase clot risk due to prolonged immobility.
- Prolonged immobility: Being bedridden for long periods can raise clot risk.
- Multiple pregnancy: Carrying twins or more can increase risk due to increased blood volume and vein pressure.
The CDC says knowing these risks helps in early detection and management of blood clots during pregnancy. Let’s look at these risks in more detail:
| Risk Factor | Description | Implication |
| Previous Blood Clot | History of blood clots before pregnancy | Increased risk of another clot during pregnancy |
| Inherited Clotting Disorder | Genetic conditions affecting blood clotting | Higher risk of clot formation |
| C-Section | Delivery by cesarean section | Increased risk due to surgery and immobility |
Understanding these risk factors helps pregnant women and their healthcare providers take steps to reduce blood clot risk. This ensures a healthier pregnancy.
Prevention and Treatment of Pregnancy Blood Clots
Learning about preventing and treating blood clots in pregnancy is key. We’ll look at ways to stop blood clots and safe treatments for those who get them.
Effective Prevention Strategies
Stopping blood clots in pregnancy needs lifestyle changes and sometimes medicine. Staying active is a good start. But, too much bed rest is bad unless a doctor says it’s okay.
- Walking regularly helps blood flow.
- Drinking lots of water is important.
- Don’t stand or sit for too long to avoid blood clots.
Women at high risk should take low-molecular weight heparin, says the National Institutes of Health. This medicine is safe for pregnant women.
“The use of low-molecular weight heparin has been shown to be effective in preventing blood clots in pregnant women at high risk.”
NATIONAL INSTITUTES OF HEALTH
Safe Treatment Options During Pregnancy
If a blood clot happens during pregnancy, quick action is needed. Treatment usually means anticoagulant medicines to stop the clot from growing and to prevent new ones.
| Treatment Option | Description | Safety During Pregnancy |
| Low-Molecular Weight Heparin | An anticoagulant that prevents clot formation | Generally considered safe |
| Unfractionated Heparin | Another type of anticoagulant used for blood clot treatment | Safe when monitored properly |
Pregnant women should talk to their doctors about the best treatment. Regular checks and changes to the treatment plan are important for the health of mom and baby.
Knowing about prevention and treatment helps pregnant women avoid blood clots. This makes for a healthier pregnancy.
Conclusion: Staying Vigilant About Blood Clots Throughout Pregnancy
It’s important to know about blood clot risks during pregnancy for a healthy journey. We’ve talked about how pregnancy ups the risk of blood clots and the types that can happen.
Knowing the signs of a blood clot, like swelling or pain in the legs, can help avoid serious issues. The Stop the Clot, Spread the Word campaign highlights the need for awareness and education about blood clots in pregnancy.
By staying informed and recognizing warning signs, women can lower their risk of blood clots. We need to focus on education and awareness to help all women have a healthy pregnancy, even those at higher risk.
Can you get blood clots during pregnancy? Yes, and knowing the risks and taking steps to prevent them can greatly reduce complications.
FAQ
What are the symptoms of a blood clot during pregnancy?
Symptoms include swelling, pain, or tenderness in the leg, arm, or other areas. Redness or discoloration is also a sign. For a pulmonary embolism (PE), look out for trouble breathing, chest pain, or a fast heart rate.
Can pregnancy cause blood clots in the legs?
Yes, pregnancy can lead to blood clots in the legs, known as deep vein thrombosis (DVT). This happens due to changes in blood clotting, increased blood volume, and vein pressure.
How common are blood clots during pregnancy?
Blood clots during pregnancy are rare but more common than in non-pregnant women. Pregnancy raises the risk by about five times.
What are the risk factors for developing blood clots during pregnancy?
Risk factors include a history of blood clots, family history, obesity, age over 35, and multiple pregnancy. Certain medical conditions like thrombophilia also increase the risk.
How are blood clots during pregnancy diagnosed?
Diagnosis involves a physical exam, ultrasound, and imaging tests like a ventilation-perfusion scan or CT scan.
What is the treatment for blood clots during pregnancy?
Treatment includes anticoagulant medication, like low-molecular-weight heparin. It prevents the clot from growing and reduces the risk of more clots.
Can blood clots during pregnancy be prevented?
Yes, preventing blood clots is possible. Stay active, avoid long periods of sitting, and use compression stockings.
Are blood clots during labor a significant risk?
Yes, blood clots are a significant risk during labor and delivery. Women at risk may receive anticoagulant medication to lower this risk.
How can I reduce my risk of blood clots during pregnancy?
To lower your risk, stay active, keep a healthy weight, avoid smoking, and follow your healthcare provider’s advice on preventing blood clots.
References
- Alsheef, M. A., et al. (2020). Pregnancy and Venous Thromboembolism: Risk Factors, Mechanisms, and Management. Frontiers in Cardiovascular Medicine, 7, 89.