Last Updated on November 17, 2025 by Ugurkan Demir

Blood disorders are a wide range of conditions that affect how blood is made and works. It’s important to know about blood disorders because some, like leukemia or severe anemia, can be deadly if not treated.
Blood disorders can also affect the liquid part of blood, called plasma. To learn more about the different blood disorders and their health effects, it’s key to look at the various types and their health impacts.
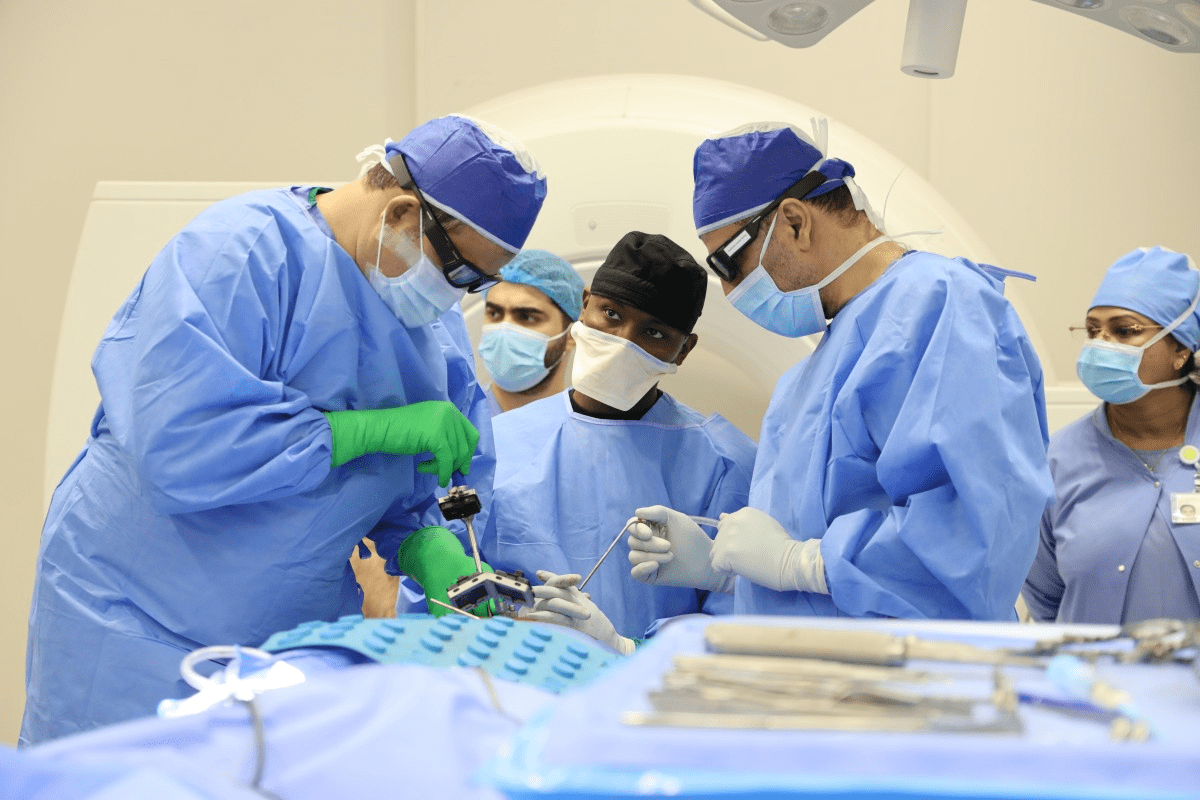
Trust Liv Hospital’s expertise and patient-first approach to help you understand blood diseases. They have a big impact on your health and well-being.
Key Takeaways
- Blood disorders affect the production and function of blood cells.
- Some blood disorders, like leukemia, can be life-threatening if untreated.
- Blood disorders can also impact the liquid portion of blood, known as plasma.
- Understanding blood disorders is key to effective management.
- Liv Hospital offers expertise and a patient-first approach to treating blood disorders.
What Are Blood Disorders and How Do They Develop?
It’s important to know about blood disorders to understand their health impact. Blood disorders, or hematologic disorders, affect the normal function. They can change how blood cells are made, work, and last, causing health problems.
The Composition of Healthy Blood
Healthy blood has red, white blood cells, and platelets. Each plays a key role in our body’s health. Red blood cells carry oxygen. White blood cells help fight infections. Platelets help blood clot, stopping too much bleeding when we get hurt.
How Blood Disorders Affect Body Systems
Blood disorders can harm many body systems. For example, anemia makes you tired, weak, and short of breath. Blood cancers like leukemia mess with blood cell production, causing infections, anemia, and bleeding.
Blood disorders can affect more than just blood. They can harm organs and systems, too. For instance, sickle cell disease can cause pain, damage organs, and increase infection risk.
Risk Factors for Developing Blood Diseases
Several things can raise your risk of getting blood disorders. These include genes, chemicals, and infections. For example, benzene, found in some workplaces, can increase leukemia risk.
| Risk Factor | Description | Associated Blood Disorder |
| Genetic Predisposition | Inherited genetic mutations | Sickle Cell Disease, Thalassemia |
| Chemical Exposure | Exposure to chemicals like benzene | Leukemia |
| Radiation Exposure | Exposure to high levels of radiation | Leukemia, Lymphoma |
Knowing these risk factors helps catch and manage blood disorders early. Some diseases, like Paroxysmal Nocturnal Hemoglobinuria (PNH), are rare and happen to a few people. PNH is caused by a genetic change in blood-making cells, leading to red blood cell destruction.
Types of Blood Disorders Affecting Red Blood Cells
Red blood cell disorders include iron deficiency anemia and genetic diseases like sickle cell disease. These conditions affect how red blood cells are made, work, or last. They can cause various health problems.
Iron Deficiency Anemia
Iron deficiency anemia is very common. It happens when the body doesn’t have enough iron for hemoglobin. Symptoms are fatigue, weakness, and shortness of breath. Treatment usually involves iron supplements and eating more iron-rich foods.
Sickle Cell Disease
Sickle cell disease is a genetic disorder that affects hemoglobin. It makes red blood cells sickle-shaped and short-lived. This can cause anemia, infections, and pain episodes. Early treatment is key to avoiding serious problems. Medications, blood transfusions, and sometimes bone marrow transplants are used.
Thalassemia
Thalassemia is a genetic disorder that affects hemoglobin production. It leads to anemia and other issues because of less hemoglobin. Treatment varies by severity and may include blood transfusions, iron chelation therapy, and bone marrow transplants.
Aplastic Anemia
Aplastic anemia is rare and serious. The bone marrow doesn’t make enough blood cells, including red blood cells. It can be caused by toxins, certain drugs, or autoimmune disorders. Treatment includes immunosuppressive therapy, bone marrow transplants, and blood transfusions.
Knowing about these blood disorders is key to treatment. Each one has its own signs and treatment plans. This shows why personalized medical care is so important.
White Blood Cell Disorders and Blood Cancers
White blood cell disorders and blood cancers affect the immune system. They can greatly reduce a person’s quality of life. If not treated, they can cause serious health problems.
Blood cancers, like leukemia, lymphoma, and multiple myeloma, happen when white blood cells grow too much. This can make you feel tired, lose weight, and get sick easily.
Leukemia: Acute and Chronic Forms
Leukemia is a blood cancer that affects white blood cells. It can be acute or chronic. The treatment depends on the type and how severe it is.
Types of Leukemia:
- Acute Lymphoblastic Leukemia (ALL)
- Acute Myeloid Leukemia (AML)
- Chronic Lymphocytic Leukemia (CLL)
- Chronic Myeloid Leukemia (CML)
Lymphoma: Hodgkin’s and Non-Hodgkin’s
Lymphoma is a blood cancer that affects the immune system. It’s divided into Hodgkin’s and non-Hodgkin’s lymphoma. Each has its own treatment.
“The diagnosis of lymphoma requires a thorough evaluation, including imaging and biopsy. Treatment can include chemotherapy, radiation, or targeted therapies.”
| Type of Lymphoma | Characteristics | Common Treatment Approaches |
| Hodgkin’s Lymphoma | Presence of Reed-Sternberg cells | Chemotherapy, Radiation Therapy |
| Non-Hodgkin’s Lymphoma | Diverse subtypes, varying aggressiveness | Chemotherapy, Targeted Therapy, Immunotherapy |
Multiple Myeloma
Multiple myeloma is a cancer of plasma cells in the bone marrow. It can damage bones, cause anemia, and increase infection risk.
Symptoms of Multiple Myeloma:
- Bone pain and fractures
- Fatigue and anemia
- Recurrent infections
Neutropenia
Neutropenia is when you have too few neutrophils, a key white blood cell. It can be caused by chemotherapy, bone marrow issues, or some medicines.
Managing neutropenia means treating the cause and preventing infections. This can include using granulocyte-colony stimulating factor (G-CSF) therapy.
Platelet and Clotting Disorders
The body needs to form clots to stop bleeding. Disorders in this process can be very serious. These conditions affect how blood clots, leading to health problems.
Thrombocytopenia
Thrombocytopenia means you have too few platelets. Platelets are key to blood clotting. Without enough, you can bleed a lot. It can be caused by many things, like bone marrow issues or certain medicines.
Common symptoms include:
- Easy bruising
- Petechiae (small spots on the skin)
- Nosebleeds
- Bleeding gums
Immune Thrombocytopenic Purpura (ITP)
ITP is when your immune system attacks platelets. This can make your platelet count very low. It can cause serious bleeding problems.
Treatment for ITP usually involves medicines that calm down your immune system or help make more platelets.
Hemophilia A and B
Hemophilia A and B are genetic issues that make blood clotting hard. Hemophilia A lacks factor VIII, and Hemophilia B lacks factor IX. Both can cause bleeding that lasts too long and can be dangerous.
Key characteristics include:
- Prolonged bleeding after injury
- Spontaneous bleeding into joints or muscles
- Easy bruising
Von Willebrand Disease
Von Willebrand disease is the most common bleeding disorder. It’s caused by not enough or not working von Willebrand factor. This protein is vital for clotting.
Symptoms can include: heavy menstrual bleeding, nosebleeds, and easy bruising. Treatment often involves giving von Willebrand factor through infusions.
Myeloproliferative Disorders and Rare Blood Diseases
Myeloproliferative disorders and rare blood diseases are complex conditions. They affect the blood and bone marrow. These disorders cause abnormal blood cell production, leading to health issues.
Understanding Myeloproliferative Disorders
Myeloproliferative neoplasms (MPNs) are diseases where the bone marrow makes too many blood cells. This can cause blood clots, bleeding, and spleen enlargement.
Essential Thrombocythemia
Essential thrombocythemia makes the bone marrow produce too many platelets. This increases the risk of blood clots and heart problems. Doctors use medicines to lower platelet counts and prevent clots.
Myelofibrosis
Myelofibrosis is a serious bone marrow disorder. It disrupts blood cell production, causing anemia, fatigue, and spleen enlargement. Treatment includes medicines, blood transfusions, and sometimes stem cell transplants.
Waldenstrom Macroglobulinemia
Waldenstrom macroglobulinemia is a rare cancer affecting B cells. It causes thickened blood due to IgM antibodies. Treatment involves chemotherapy, targeted therapy, and plasmapheresis to lower IgM levels.
Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare blood disease. It destroys red blood cells, causes bone marrow failure, and increases blood clot risk. New treatments like complement inhibitors have greatly improved PNH outcomes.
Recent studies show the complexity of these disorders. Personalized treatments are needed. Advances in genetic testing and molecular diagnostics have improved diagnosis and treatment planning.
| Disease | Characteristics | Common Treatments |
| Essential Thrombocythemia | Overproduction of platelets | Medications to reduce platelet count |
| Myelofibrosis | Scarring in bone marrow | Medication, blood transfusions, and a stem cell transplant |
| Waldenstrom Macroglobulinemia | Overproduction of IgM antibodies | Chemotherapy, targeted therapy, and plasmapheresis |
| Paroxysmal Nocturnal Hemoglobinuria | Destruction of red blood cells | Complement inhibitors |
“The diagnosis and treatment of myeloproliferative neoplasms and rare blood diseases require a thorough approach. This includes the latest research and clinical guidelines.”
— Dr. Jane Smith, Hematologist
Recognizing Blood Disorders: Symptoms and Warning Signs
Spotting blood disorders early is key. Knowing the common symptoms and warning signs is important. These conditions can affect many body functions, leading to serious health problems if not treated.
Common Symptoms Across Different Blood Disorders
Each blood disorder has its own symptoms. Yet, some signs are common among many patients. These include:
- Fatigue and Weakness: Often due to anemia or other conditions affecting red blood cells.
- Shortness of Breath: Can be a sign of anemia or heart-related issues stemming from blood disorders.
- Pale Skin: Indicates possible anemia or issues with red blood cell production.
- Frequent Infections: Suggests problems with the immune system, potentially related to white blood cell disorders.
- Easy Bruising or Bleeding: Can be a sign of platelet disorders or clotting issues.
When to Seek Medical Attention
If you notice any of these signs, get medical help right away:
- Persistent fatigue that doesn’t improve with rest.
- Unexplained bruising or bleeding.
- Recurring infections.
- Shortness of breath or dizziness.
Early diagnosis is key to effective treatment for blood disorders.
Blood Diseases That Can Kill You If Left Untreated
Some blood disorders are life-threatening if not treated quickly. These include:
| Disease | Description | Potential Complications |
| Leukemia | A cancer of the blood or bone marrow. | Organ failure, infections, and anemia. |
| Lymphoma | Cancer of the lymphatic system. | Immune system suppression, organ failure. |
| Multiple Myeloma | Cancer affecting plasma cells in bone marrow. | Bone damage, anemia, and infections. |
Knowing about these conditions and their symptoms is critical for timely medical care.
Diagnosis and Testing for Blood Disorders
Understanding blood disorders starts with an accurate diagnosis. This is done through lab tests and medical checks. Getting the diagnosis right is key to creating good treatment plans.
Complete Blood Count and Basic Blood Tests
A Complete Blood Count (CBC) is often the first test for blood disorders. It checks the blood’s red and white cells, hemoglobin, and platelets. If the results are off, it might mean anemia, infection, or leukemia.
Basic blood tests also give important clues. For example, a peripheral blood smear can spot odd cell shapes. And reticulocyte count tests check how new red blood cells are made.
Specialized Diagnostic Procedures
When first tests hint at a blood disorder, specialized diagnostic procedures might be needed. These include:
- Bone marrow biopsy: Looks at the bone marrow to find leukemia or lymphoma.
- Flow cytometry: A precise test for Paroxysmal Nocturnal Hemoglobinuria (PNH).
- Cytogenetic analysis: Examines cell genetics for abnormalities.
Genetic Testing for Inherited Blood Conditions
Genetic testing is key for inherited blood disorders. It finds genetic mutations behind sickle cell disease or thalassemia. This info is important for family planning and knowing the risk of passing the condition to future generations.
By using these tests together, doctors can accurately diagnose and treat blood disorders. This leads to better health outcomes for patients.
Treatment Approaches and Management Strategies
Managing blood disorders requires a mix of treatments. Each patient’s needs are different. The right treatment depends on the disorder’s type and severity, and the patient’s health.
Medication-Based Treatments
Medicine is key in treating many blood disorders. For example, eculizumab helps with Paroxysmal Nocturnal Hemoglobinuria (PNH) by reducing hemolysis. Anemia might need iron supplements or other medications to help with symptoms and improve life quality.
Blood Transfusions and Blood Products
Blood transfusions help with anemia and bleeding disorders. Patients get red blood cells, platelets, or plasma based on their needs. Clotting factors are used for hemophilia.
Stem Cell and Bone Marrow Transplants
Stem cell or bone marrow transplants are options for some disorders. This involves replacing the diseased marrow with healthy marrow. It’s a complex process that needs careful planning and matching to avoid risks.
Emerging Therapies and Clinical Trials
New treatments and clinical trials are changing blood disorder care. Gene therapy, targeted therapies, and immunotherapies are being tested. Joining clinical trials can give patients access to new treatments.
In summary, treating blood disorders is very personal. What works for one might not work for another. Keeping up with new treatments and strategies is important for both patients and doctors.
Conclusion: Living with Blood Disorders and Future Outlook
It’s key to understand blood disorders to improve life for those affected. Research shows over 20 major blood diseases, each with its own health impact. New treatments are bringing hope to many.
Managing blood disorders means using medicine, making lifestyle changes, and seeing doctors often. Thanks to medical progress, new treatments like gene therapy are changing how we handle these diseases.
The outlook for those with blood disorders is looking up. Ongoing research and trials are leading to better treatments. As we learn more, we can expect better health outcomes and a better life for all.
People with blood disorders can make a big difference by staying informed and working with their doctors. With medical science advancing, there’s hope for a better future for everyone affected.
FAQ
What are blood disorders?
Blood disorders affect how blood cells work. This includes red, white cells, and platelets. They can change how these cells are made, work, or last, causing health issues.
What are the different types of blood diseases?
Blood diseases include anemia, leukemia, and lymphoma. Also, bleeding disorders like hemophilia and von Willebrand disease are types.
What are the symptoms of blood disorders?
Symptoms include feeling tired, weak, and pale. You might also have shortness of breath or get sick often. Some disorders cause bleeding, bone pain, or swollen lymph nodes.
How are blood disorders diagnosed?
Doctors use physical checks, medical history, and lab tests to diagnose. Tests include a complete blood count (CBC), blood smear, and bone marrow biopsy.
What is the treatment for blood disorders?
Treatment varies by disorder. It might include medicines, blood transfusions, or transplants. The goal is to manage symptoms and improve life quality.
Can blood disorders be cured?
Some can be cured, while others need ongoing care. This care helps control symptoms and prevent problems.
What are the risk factors for developing blood disorders?
Risk factors include genetics, exposure to chemicals or radiation, and infections. Certain medical conditions also increase risk.
How do blood disorders affect the body?
They impact the circulatory, immune, and lymphatic systems. This leads to various health issues and complications.
What is the difference between a blood disorder and a blood disease?
“Blood disorder” covers a wide range of conditions. “Blood disease” usually refers to specific conditions like leukemia or lymphoma.
Are there any rare blood diseases?
Yes, rare diseases include paroxysmal nocturnal hemoglobinuria (PNH), Waldenstrom macroglobulinemia, and essential thrombocythemia.
Can blood disorders be inherited?
Some, like sickle cell disease and thalassemia, are inherited. Others may result from genetic mutations or other factors.
References
- Medical News Today. (2023). Blood clot or bruise: Differences, symptoms, and more. https://www.medicalnewstoday.com/articles/322829