Last Updated on November 17, 2025 by Ugurkan Demir

If you have multiple myeloma, a bone marrow transplant might be key to beating the disease. At Liv Hospital, we know how complex this treatment is. We’re dedicated to giving you top-notch care.
An autologous stem cell transplant (ASCT) is often the best choice for some patients. It uses healthy stem cells to replace damaged bone marrow. This can lead to a lasting response to the disease.
We’ll share important facts about this treatment. This will help you know what to expect and make smart choices about your care.
Key Takeaways
- Autologous stem cell transplant is a standard treatment for eligible multiple myeloma patients.
- This procedure can lead to long-lasting remission and improved quality of life.
- Liv Hospital provides internationally benchmarked care for patients undergoing bone marrow transplant.
- A multidisciplinary team will guide you through the treatment process.
- Advanced protocols are in place to ensure the best possible outcomes.
Understanding Multiple Myeloma and Its Treatment Landscape

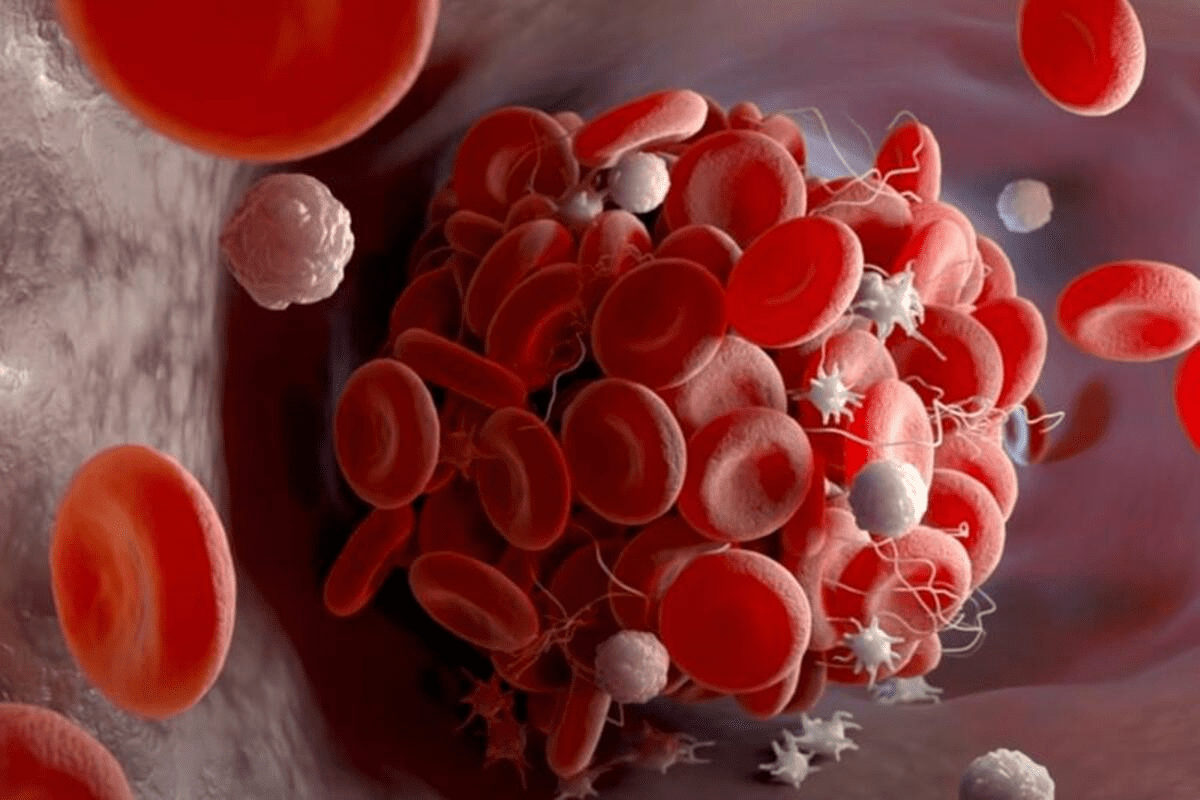
Multiple myeloma is a cancer that affects a type of white blood cell called plasma cells. These cells help fight infections by making antibodies. But in multiple myeloma, these cells become abnormal and multiply too much.
What is Multiple Myeloma?
When plasma cells become abnormal, they crowd out healthy blood cells in the bone marrow. Instead of making useful antibodies, they produce harmful proteins. This can lead to serious health problems.
Key characteristics of multiple myeloma include:
- Anemia
- Bone pain or lesions
- Hypercalcemia (high calcium levels)
- Renal impairment
Standard Treatment Approaches
Treatment for multiple myeloma has changed a lot. It now includes a mix of therapies based on each patient’s needs. These treatments can be:
- Targeted therapy: Drugs that target cancer cells.
- Chemotherapy: Traditional treatment that kills fast-growing cells.
- Corticosteroids: Anti-inflammatory drugs that kill myeloma cells.
- Immunotherapy: Treatments that boost the immune system to fight cancer.
Where Transplantation Fits in the Treatment Strategy
Bone marrow transplantation is a key treatment for many patients with multiple myeloma. It replaces the diseased marrow with healthy marrow. For some, autologous stem cell transplant (ASCT) is a standard treatment, aiming for better outcomes and longer life.
Choosing to have a bone marrow transplant depends on several factors. These include the patient’s health, disease status, and how well they respond to initial treatments. We’ll look into ASCT and who might be eligible in the next sections.
Bone Marrow Transplant for Multiple Myeloma: The Basics
It’s important for patients and doctors to know about bone marrow transplant in treating multiple myeloma. This treatment, called autologous stem cell transplant (ASCT), is key for some patients with this disease.
Autologous Stem Cell Transplant (ASCT) Explained
ASCT uses the patient’s own stem cells, taken before high-dose chemotherapy. This lets doctors give stronger treatments to kill myeloma cells. The American Cancer Society explains, “Your own blood stem cells are removed before treatment and then given back to you later to rebuild your bone marrow.”
The ASCT process includes several steps:
- Stem cell collection: Gathering the patient’s stem cells, typically from the peripheral blood.
- Conditioning regimen: Administering high-dose chemotherapy to eliminate the myeloma cells.
- Stem cell infusion: Reinfusing the collected stem cells to repopulate the bone marrow.
Difference Between Bone Marrow and Peripheral Blood Stem Cell Collection
Before, bone marrow was taken directly from bones. Now, most use peripheral blood stem cell collection. This method uses growth factors to move stem cells into the blood, then collects them through apheresis.
| Characteristics | Bone Marrow Harvest | Peripheral Blood Stem Cell Collection |
| Method | Surgical extraction from bones | Apheresis after mobilization |
| Pain and Recovery | More invasive, longer recovery | Less invasive, quicker recovery |
| Stem Cell Yield | Limited by the number of bones | Can be enhanced with mobilization agents |
Why ASCT Remains the Standard of Care
ASCT is a main treatment for some multiple myeloma patients. It greatly improves response rates and survival. A leading expert says, “ASCT has been shown to provide a significant progression-free survival benefit, making it a cornerstone in the treatment of multiple myeloma.”
The benefits of ASCT include:
- Improved depth of response
- Prolonged progression-free survival
- Potential for improved overall survival
In conclusion, ASCT is a key part of treating multiple myeloma for many patients. Knowing how it works and its benefits is vital for making informed care decisions.
Patient Eligibility: Who Can Benefit from Transplantation?
To see if a patient can get a stem cell transplant, we look at their health and the disease. For those with multiple myeloma, several things matter. These help us decide if the transplant is a good choice.
Age Considerations and Performance Status
Age is key, but not the only thing we look at. We consider physiological age and health, too. We check how well a patient can handle the transplant.
- Patients under 65 are usually better candidates.
- Those over 65 might also qualify, based on their health.
- We also check for other health issues and organ function.
Disease Status Requirements
The state of multiple myeloma is very important. Patients who have responded well to treatment do better with a transplant.
Disease responsiveness to first treatments is a big factor. We look at:
- How well the disease responds to initial treatments.
- Presence of high-risk genetic features.
- How long has the disease been responding to treatment?
Comorbidities and Contraindications
Having other health issues can affect transplant eligibility. Problems like heart, lung, or kidney disease raise risks.
We check each patient’s medical history and current health. This helps us find any issues that might stop them from getting a transplant. Relative contraindications include:
- Severe heart problems.
- Major lung issues.
- Active infections.
In short, deciding if a patient can get a bone marrow transplant is complex. We look at age, disease, and health issues. This way, we can find out who will likely benefit from this treatment.
The Stem Cell Collection Process: From Mobilization to Harvest
The journey to a bone marrow transplant for multiple myeloma starts with collecting stem cells. This step is key to transplant success. It gives healthy stem cells to replace damaged bone marrow.
Modern Stem Cell Mobilization Techniques
Stem cell mobilization is the first step. It gets stem cells from the bone marrow into the blood. We use new methods that mix growth factors with chemotherapy to boost stem cell production.
Growth factors, like granulocyte-colony stimulating factor (G-CSF), help the bone marrow. Sometimes, chemotherapy is added to G-CSF for better results.
Colony-Stimulating Factors and Chemotherapy Combinations
Colony-stimulating factors, like G-CSF, are key in mobilization. They help the bone marrow make more stem cells. Adding chemotherapy can increase the stem cell count collected.
Before apheresis, patients get daily growth factor shots. This increases stem cell production and moves them into the blood for collection. This takes a few days.
The Apheresis Procedure Explained
Apheresis collects stem cells from the blood. The patient’s blood is drawn, and the stem cells are separated. Then, the stem cells are collected, and the rest of the blood is returned.
This can take hours and might need to be done over several days. Our team watches over the patient to make sure it goes smoothly.
Understanding the stem cell collection process helps patients prepare for this important step in treating multiple myeloma. Our team is here to support you every step of the way.
High-Dose Chemotherapy and the Transplantation Procedure
Before a stem cell transplant, patients get a special treatment to kill cancer cells and weaken their immune system. This step is key to the transplant’s success.
Melphalan as the Standard Conditioning Regimen
Melphalan is the main treatment for multiple myeloma patients getting a stem cell transplant. High-dose melphalan kills cancer cells in the bone marrow. This makes room for new stem cells to grow. It’s backed by lots of research and is a mainstay in treating multiple myeloma.
The conditioning process uses chemotherapy and sometimes radiation. It kills cancer cells and weakens the immune system. This step is vital to lowering cancer relapse risk and helping the graft succeed.
The Transplantation Process Step-by-Step
The transplant process is detailed and involves several important steps:
- Preparation for the transplant, including the administration of high-dose chemotherapy
- Infusion of the stem cells into the patient’s bloodstream
- Monitoring the patient for signs of engraftment and possible complications
After the conditioning, the stem cells are given back to the patient through an IV. This is like a blood transfusion and takes a few hours.
Hospital Stay and Immediate Recovery Period
The hospital stay for a stem cell transplant can last from a few days to a couple of weeks. Patients are watched closely for any complications or graft failure.
After leaving the hospital, patients start their recovery. They are watched for signs of engraftment and complications. Recovery times vary, but most patients feel better in a few weeks.
Important parts of recovery include:
- Managing side effects and complications
- Following a strict infection prevention protocol
- Attending follow-up appointments with the healthcare team
Knowing about the transplant process and what to expect in the hospital and recovery helps patients prepare for this important part of their treatment.
Post-Transplant Recovery and Maintenance Therapy
The journey doesn’t end with a bone marrow transplant. Post-transplant recovery and maintenance therapy are key to managing multiple myeloma. After the transplant, patients need careful monitoring and treatment strategies for the best outcomes.
Recovery Timeline After Discharge
Recovery after discharge can vary a lot from patient to patient. It usually takes several months to a year or more to fully recover. During this time, patients are watched closely for signs of relapse, infections, and other complications.
Key aspects of the recovery timeline include:
- Initial recovery phase (0-3 months): Focus on managing immediate post-transplant side effects and complications.
- Intermediate phase (3-6 months): Gradual improvement in energy levels and overall health.
- Long-term recovery (6-12 months and beyond): Continued monitoring and adjustment of maintenance therapy as needed.
Lenalidomide and Other Maintenance Options
Maintenance therapy is a key part of post-transplant care for multiple myeloma patients. The American Cancer Society says most patients start maintenance therapy a few months after transplant. Lenalidomide is often used, either alone or with another drug. It has been shown to improve survival and disease-free time for many patients.
Other maintenance options include:
- Bortezomib: A proteasome inhibitor used in various maintenance regimens.
- Daratumumab: A monoclonal antibody that targets myeloma cells.
- Combination therapies: Using multiple drugs to target different aspects of the disease.
Long-term Monitoring Protocol
Long-term monitoring is key to catching early signs of relapse and managing treatment side effects. This involves:
- Regular blood tests to monitor blood cell counts and detect any abnormalities.
- Periodic bone marrow biopsies to assess the status of the disease.
- Imaging studies (e.g., PET scans) as needed to evaluate disease activity.
- Monitoring for late effects of treatment, such as secondary cancers or organ damage.
Effective maintenance therapy and long-term monitoring help healthcare providers improve outcomes for multiple myeloma patients after a bone marrow transplant.
Advanced Transplant Strategies: Beyond Standard ASCT
For those with multiple myeloma, new transplant methods offer hope. These methods go beyond the usual autologous stem cell transplant (ASCT). Research is always moving forward, leading to new ways to help patients.
Tandem (Double) Transplants for High-Risk Disease
Tandem or double transplants use two autologous transplants, spaced 3 to 6 months apart. This is for patients with high-risk multiple myeloma. The American Cancer Society says some doctors suggest this for certain patients, hoping to improve treatment results.
Tandem transplants might help by killing more myeloma cells. But they also raise the chance of side effects from treatment.
Allogeneic Transplantation: When Is It Considered?
Allogeneic transplantation uses stem cells from a donor. It’s not often used for multiple myeloma because of risks like graft-versus-host disease (GVHD). Yet, it might be an option for younger patients or those with certain disease traits.
“Allogeneic transplantation can offer a potentially curative graft-versus-myeloma effect, but its use is limited by the availability of suitable donors and the risk of severe complications.”
Novel Conditioning Regimens
Scientists are looking into new ways to make transplants work better and safer. They want to kill more myeloma cells while keeping the patient safe.
They’re trying out different combinations of conditioning agents. Personalized conditioning regimens based on each patient’s needs and disease are also being studied.
As we move forward in treating multiple myeloma, these new transplant methods will likely become more important. They could help make treatments better for patients.
Potential Complications and How They’re Managed
Bone marrow transplantation can cure multiple myeloma, but it comes with risks. Knowing about these complications and how to handle them is key for both patients and doctors.
Common Short-Term Side Effects
Right after a bone marrow transplant, patients face many challenges. They might feel tired, nauseous, vomit, have diarrhea, and lose their hair. We use different methods to help them feel better and live better during this tough time.
Managing these side effects well is important. It helps keep patients healthy and strong. We use medicines to stop nausea, give them food to eat, and tailor care to each patient’s needs.
Infection Risks and Prevention Strategies
Patients getting bone marrow transplants are more likely to get infections. This is because the treatment weakens their immune system. We use antibiotics, antiviral drugs, and keep them isolated to lower the risk of infections.
Watching for signs of infection is a big part of taking care of patients after transplant. We teach them to watch for fever, chills, or cough. If they see these signs, they need to get help right away.
Long-Term Health Considerations
After recovering from a bone marrow transplant, patients face long-term health issues. These include risks of graft-versus-host disease, damage to organs, and new cancers.
We stress the need for ongoing care to watch for these problems. This means regular check-ups, checking how organs are working, and looking for new cancers.
By knowing about the risks of bone marrow transplantation and how to deal with them, we can make sure patients do well. This helps them live better lives after treatment.
Conclusion: The Evolving Role of Transplantation in Multiple Myeloma Care
We’ve looked into the key points of bone marrow transplant for multiple myeloma. This treatment has changed how we manage this disease. Autologous stem cell transplantation (ASCT) is a key part of treatment for some patients. It helps them live longer and fight the disease better.
The advancements in ASCT have made a big difference. Using melphalan in treatment and lenalidomide for maintenance has improved results. As we keep learning, the treatment for multiple myeloma will likely get even better.
Thanks to new treatments, people with multiple myeloma are living longer. It’s important to keep up with the latest in bone marrow transplant for multiple myeloma. The changing role of transplantation shows we need a team effort to care for patients. This ensures they get the best treatment possible.
FAQ
What is the role of autologous stem cell transplant (ASCT) in multiple myeloma treatment?
ASCT is a key treatment for multiple myeloma. It uses high-dose chemotherapy. Then, the patient’s own stem cells are given back to them.
How are stem cells collected for multiple myeloma patients undergoing ASCT?
Stem cells are collected from the blood. This is done after using special drugs to help move the stem cells into the blood.
What is the difference between bone marrow and peripheral blood stem cell collection?
Bone marrow collection takes stem cells directly from the bone. It’s done under general anesthesia. Peripheral blood collection moves stem cells into the blood first, then collects them.
What are the eligibility criteria for bone marrow transplantation in multiple myeloma?
Who can get a bone marrow transplant depends on age, disease status, and health. It also looks at how well the patient can handle treatment.
What is the conditioning regimen used in ASCT for multiple myeloma?
Melphalan is the main treatment used in ASCT. It’s given in high doses to kill myeloma cells.
What are the possible complications of bone marrow transplantation for multiple myeloma?
Complications can include short-term side effects and infection risks. There are also long-term risks like secondary cancers and organ damage.
What is maintenance therapy, and why is it used after ASCT?
Maintenance therapy, like lenalidomide, is used after ASCT. It helps keep the disease under control and lowers the chance of relapse.
Can patients with high-risk multiple myeloma benefit from tandem transplants?
Tandem transplants might help those with high-risk multiple myeloma. It can reduce the disease burden and improve outcomes.
What is the role of allogeneic transplantation in multiple myeloma treatment?
Allogeneic transplantation uses donor stem cells. It’s considered for younger patients with high-risk disease or those who’ve had ASCT before.
How are infection risks managed during the post-transplant period?
Infection risks are managed with antibiotics and antiviral drugs. Patients are also closely monitored for signs of infection.
What is the typical recovery timeline after discharge following ASCT?
Recovery time varies. Patients usually get their blood counts back in a few weeks. Full recovery can take several months.
References:
- Deloitte US Center for Health Solutions. (2025). 2025 global health care outlook. Deloitte. https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-global-health-care-executive-outlook.html