Last Updated on October 21, 2025 by mcelik
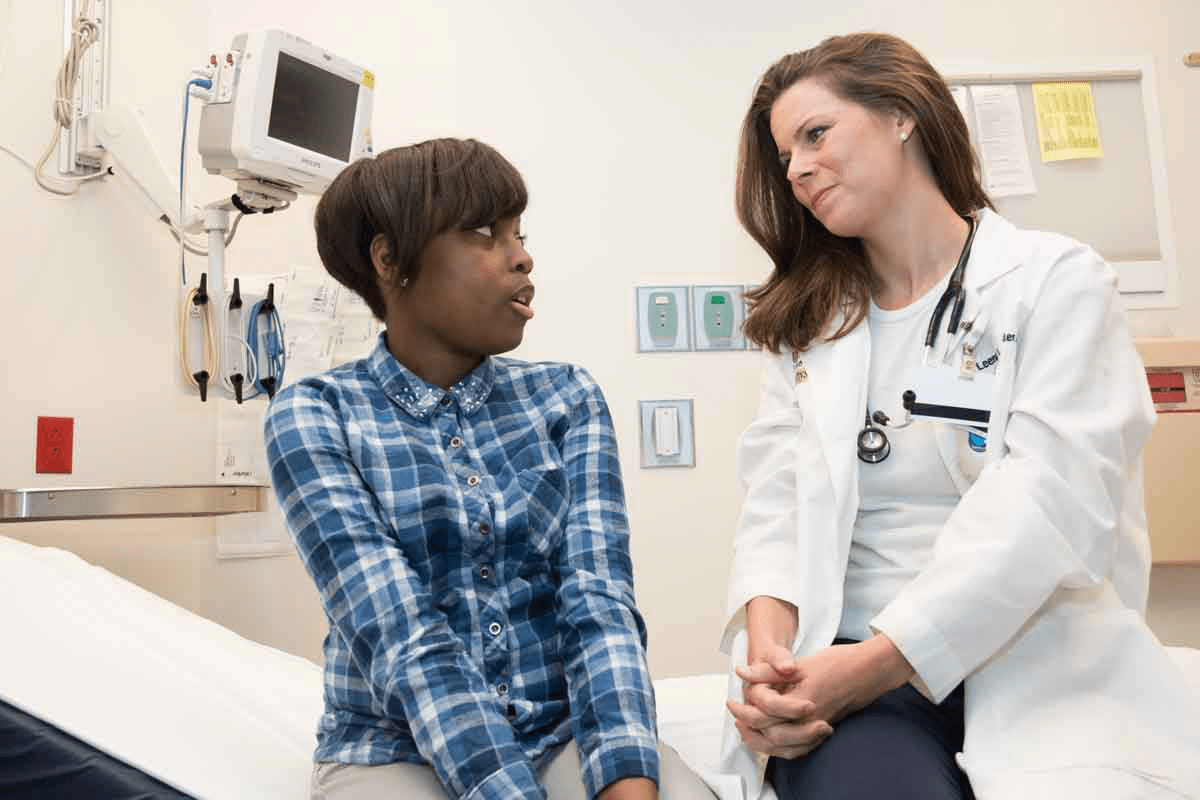
For those getting allogeneic stem cell transplants, pulmonary graft versus host disease (GVHD) is a big worry. At Liv Hospital, we tackle this complex issue head-on. We’re all about giving top-notch, patient-centered care.
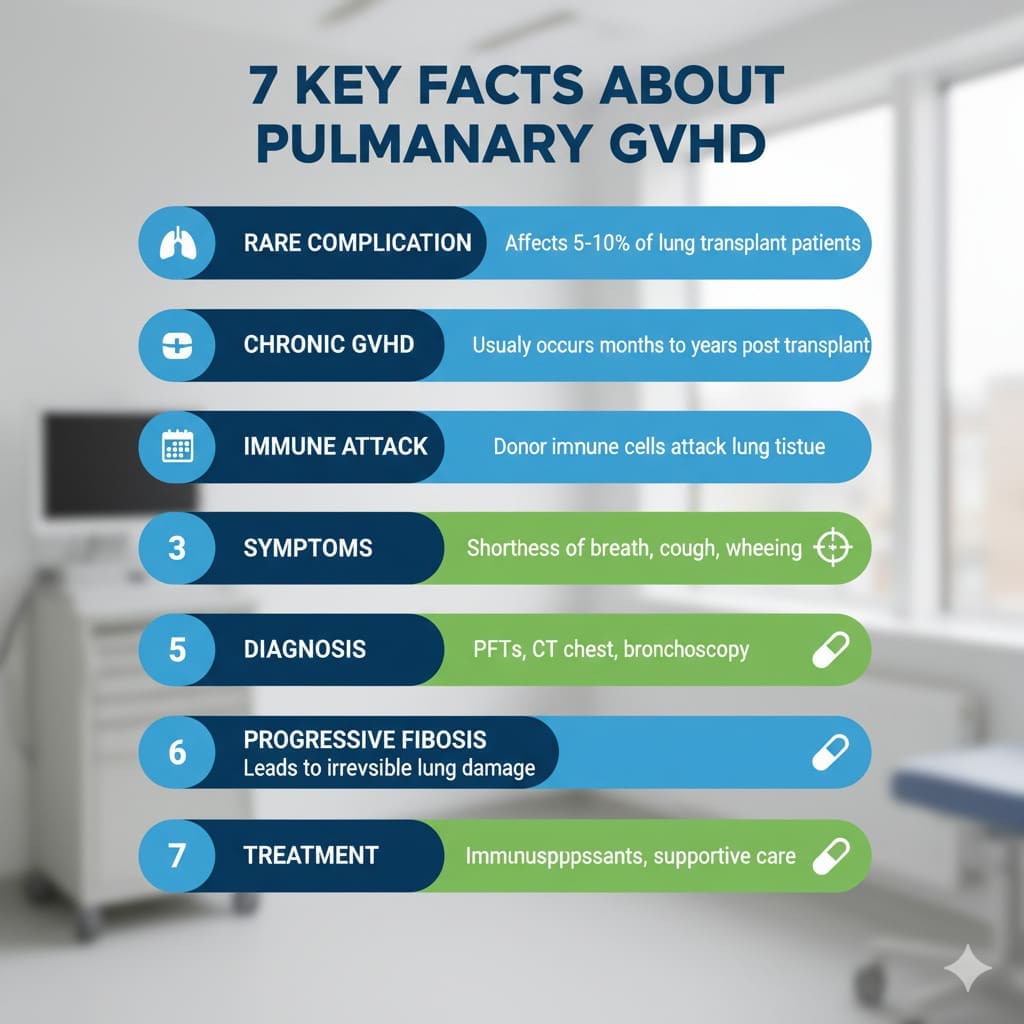
Pulmonary GVHD can show up as either acute or chronic. Chronic GVHD is tough, with about 14% of patients getting bronchiolitis obliterans syndrome (BOS). This is a severe lung disease caused by GVHD.
It’s key to know the signs and treatment choices for graft versus host disease lung. Our team is ready to offer care that meets international standards. We aim for the best results for our patients.
Key Takeaways
- Pulmonary GVHD is a serious complication following allogeneic stem cell transplantation.
- Chronic GVHD can lead to bronchiolitis obliterans syndrome (BOS).
- Understanding symptoms and treatment options is key for managing the disease well.
- Liv Hospital offers advanced, patient-focused care for pulmonary GVHD.
- Our dedicated team delivers care that meets international standards.
What is Graft Versus Host Disease Lung?
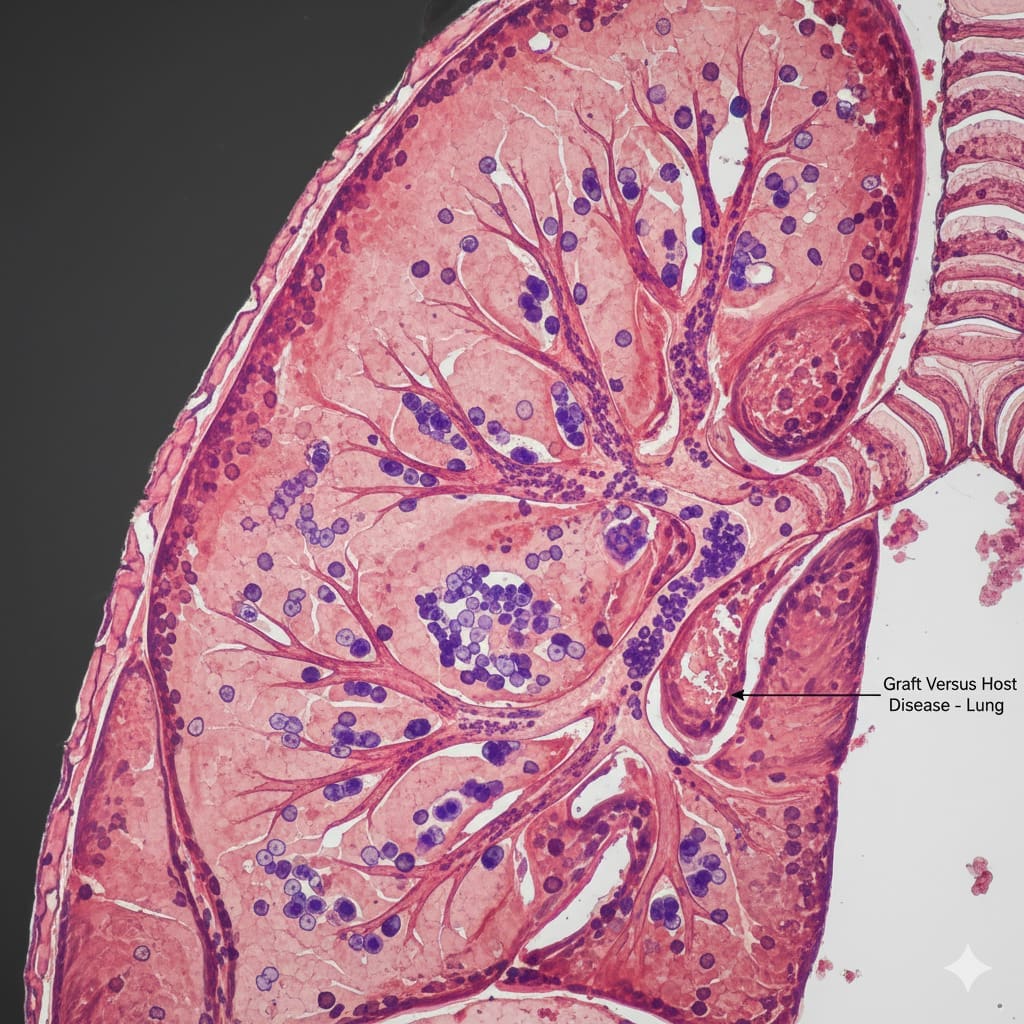
Pulmonary GVHD is when the graft attacks the host’s lung tissue. It’s a big worry for those getting allogeneic hematopoietic stem cell transplantation. This lung GVHD is serious and can cause a lot of harm and death.
To get pulmonary GVHD, we need to understand how the host and graft interact. The thymus is key in keeping the immune system balanced. CD8+ cytotoxic T lymphocytes (CTLs) help fight infections and tumors. Their fight with the graft can cause GVHD.
The Pathophysiology of Pulmonary GVHD
Pulmonary GVHD is a complex fight between donor immune cells and the host’s lung. This fight causes inflammation and damage to the lung. Knowing this helps us find better ways to diagnose and treat it.
Studies show T cells drive the GVHD immune response. When donor T cells see host antigens, they attack the host’s tissues, including the lungs.
Host vs. Graft Immunologic Interactions
The fight between the host and graft is at the heart of GVHD. Donor immune cells see the host’s tissues as foreign and attack. This can badly damage the lungs.
CD8+ CTLs and other immune cells play a big role in this fight. The table below shows the main interactions in pulmonary GVHD.
| Immune Cell | Role in GVHD |
|---|---|
| CD8+ CTLs | Mediate cytotoxic response against host lung tissues |
| CD4+ T cells | Regulate immune response and cytokine production |
| Dendritic Cells | Present antigens to T cells, initiating the immune response |
A study found, “The fight between donor and host immune cells is key in GVHD. Understanding this fight is important for finding treatments.”
“GVHD is a big problem for allogeneic hematopoietic stem cell transplantation. Its lung effects are very serious and can lead to a lot of harm and death.”
Fact 1: Acute vs. Chronic Pulmonary GVHD Present Differently
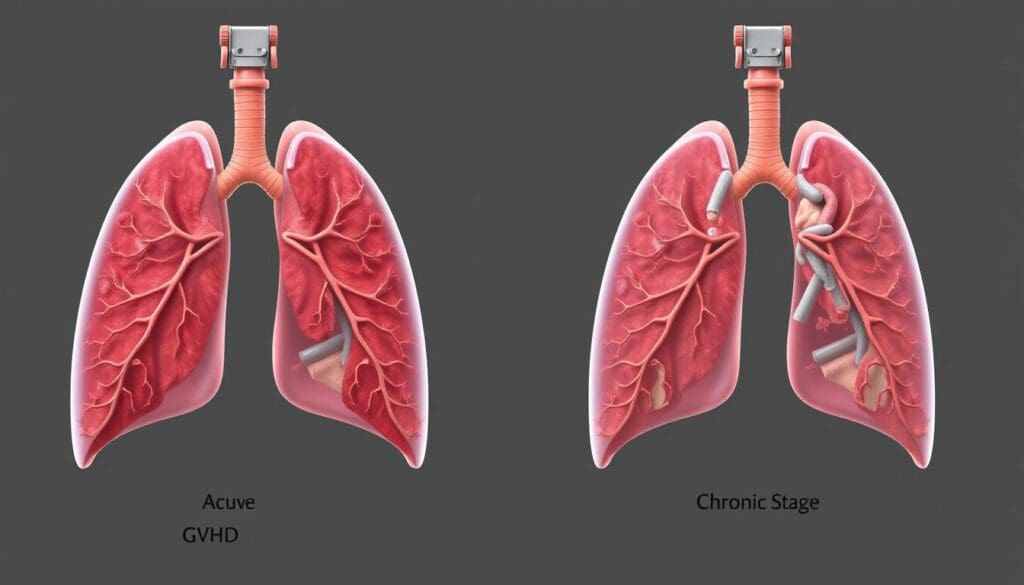
It’s important to know the difference between acute and chronic pulmonary GVHD. GVHD lung symptoms change based on the type, affecting how we treat pulmonary GVHD.
Acute GVHD happens in the first 100 days after a transplant. It’s marked by a strong immune reaction. In the lungs, it can cause cough, trouble breathing, and fever.
Acute Lung GVHD Manifestations
Acute lung GVHD can be hard to spot because its symptoms are not always clear. “It can look like other lung problems, like infections or idiopathic pneumonia syndrome,” says a doctor. This makes it key to watch for it in transplant patients.
- Dyspnea
- Cough
- Fever
- Pulmonary infiltrates on imaging
Spotting these signs early is vital for quick treatment.
Chronic Lung GVHD Characteristics
Chronic GVHD starts after 100 days post-transplant and can affect many parts of the body, including the lungs. It shows up slowly, with symptoms like getting worse breathing and lung blockages.
A doctor notes, “Chronic GVHD can cause a lot of problems, with bronchiolitis obliterans syndrome being a big issue in lung health.”
Knowing these differences helps us manage pulmonary GVHD better and improve patient care.
Fact 2: Bronchiolitis Obliterans Syndrome Affects 14% of Chronic GVHD Patients
BOS is a major problem for 14% of those with chronic GVHD. It blocks small airways, causing lasting lung damage.
Understanding BOS as the Primary Form of GVHD Lung Disease
BOS is a big issue for those with chronic GVHD. It happens when the immune system attacks the lungs. The inflammation and scarring of the bronchioles lead to their blockage.
Spotting BOS early is key to better care. Symptoms like shortness of breath, cough, and wheezing can really hurt a patient’s life quality.
Impact on Mortality and Quality of Life
BOS in chronic GVHD patients leads to high rates of sickness and death. It can cut down survival chances and harm lung function. This makes managing GVHD very important.
| Condition | Impact on Lung Function | Mortality Rate |
|---|---|---|
| BOS | Severe Obstruction | High |
| Chronic GVHD without BOS | Variable | Moderate |
Dealing with lung GVHD needs a full plan. This includes watching for BOS and using the right treatments. We aim to help patients by giving them the best care on time.
Knowing about BOS in chronic GVHD helps us tackle lung problems better. Good care plans are vital for improving life quality for these patients.
Fact 3: Graft Versus Host Disease Lung Manifests in Multiple Forms
The lung problems caused by GVHD can vary a lot. This makes it hard to diagnose and treat pulmonary GVHD. Each type needs a different way to handle it.
Obstructive Lung Syndromes
Obstructive lung problems, like bronchiolitis obliterans syndrome (BOS), are common in chronic GVHD. BOS causes inflammation and scarring in the small airways. This leads to trouble breathing, coughing, and wheezing. Early detection is key to avoid lasting damage.
Restrictive Lung Syndromes
Restrictive lung issues, on the other hand, make it hard to take a deep breath. This is because of inflammation and scarring in the lung tissue. Symptoms include shortness of breath and feeling tired easily. High-resolution CT scans are vital for spotting these problems.
Mixed Lung Syndromes
Some people have both obstructive and restrictive lung problems at the same time. This makes it even harder to diagnose. A thorough check-up, including lung function tests and imaging, is needed.
Diagnosing GVHD lung issues involves a few steps. These include checking the patient, doing lung function tests, and using imaging. Getting it right is key to helping patients get better.
- Pulmonary function tests help assess lung function and identify specific patterns of lung disease.
- High-resolution CT scans provide detailed images of the lung parenchyma and airways.
- Bronchoscopy with bronchoalveolar lavage (BAL) may be used to assess for infection or inflammation.
It’s important to know about the different lung problems caused by GVHD. This helps doctors give the best care to their patients. By understanding the various lung issues, doctors can tailor treatments to each patient’s needs.
Fact 4: Incidence of Pulmonary GVHD Ranges from 15% to 50%
The incidence of pulmonary GVHD varies a lot. This is due to many factors like donor-recipient matching and patient demographics. It shows how complex GVHD is and why we need care tailored to each patient.
Variation in Reported Incidence Rates
Research shows pulmonary GVHD can affect 15% to 50% of patients. This range comes from the diversity in patient groups and transplant methods. Differences in donor types, conditioning regimens, and how to prevent GVHD play a big role.
A study on allogeneic hematopoietic stem cell transplants found a higher incidence of pulmonary GVHD in patients with unrelated donors. This shows how important matching donors is in assessing GVHD risk.
Key Risk Factors Including Donor Matching and Patient Age
Donor matching and patient age are key factors in developing pulmonary GVHD. Mismatched donors face a higher risk because of increased alloreactivity. Older patients are also more at risk due to weaker immune systems and more health issues.
We have made a table to show the main risk factors and their effect on pulmonary GVHD incidence:
| Risk Factor | Impact on Pulmonary GVHD Incidence | Relative Risk |
|---|---|---|
| Donor Mismatch | Increased incidence due to heightened alloreactivity | 2.5 |
| Patient Age > 50 | Increased susceptibility due to decreased immune function | 1.8 |
| Prior History of GVHD | Higher risk of developing pulmonary GVHD | 2.2 |
Knowing these risk factors is key to spotting and treating pulmonary GVHD early. By understanding what increases GVHD risk, doctors can create better plans to lower these risks. This helps improve patient care and outcomes.
Fact 5: Early Pulmonary GVHD is Often Underdiagnosed
Diagnosing pulmonary GVHD early is hard because its symptoms are not clear. Finding it early is key to treating it well. But, its symptoms are similar to many other lung problems, making it hard to diagnose.
Challenges in Early Detection
One big problem is that GVHD symptoms like cough and wheezing are common. These symptoms can be found in many lung diseases. This makes it tough to know if it’s GVHD without special tests.
Doctors usually look at symptoms and if someone had a bone marrow transplant. But, there’s no clear way to tell if someone has GVHD in their lungs early on.
Diagnostic Approaches and Testing
To figure out if someone has GVHD in their lungs, doctors use several methods. Pulmonary function tests can show if the lungs are working right or not.
High-resolution CT scans are also important. They help see how bad the lung damage is. These scans can help doctors confirm GVHD, along with other signs and tests.
The Role of Pulmonary Function Tests and Imaging
Pulmonary function tests are key in diagnosing and tracking GVHD. They show how bad the lung damage is. This helps doctors decide the best treatment.
Imaging, like HRCT, gives detailed pictures of the lungs. This helps doctors see how severe the disease is. Using tests and images together is important for managing GVHD in the lungs.
By understanding the challenges in early detection and using the right tests, we can better manage GVHD. This could lead to better outcomes for patients.
Fact 6: Treatment Options Include Lung Transplantation for Advanced Cases
GVHD lung treatment has many strategies, from common therapies to lung transplantation. The treatment choice depends on the disease’s severity, the patient’s health, and how GVHD affects the lungs.
Standard Therapeutic Approaches
GVHD treatment often starts with immunosuppressive drugs to stop the immune system from attacking the graft. Corticosteroids are usually the first choice because they reduce inflammation and immune reactions. Other drugs may also be used, alone or together, to manage GVHD.
A study in the Journal of Clinical Oncology found that immunosuppressive therapy has greatly improved GVHD outcomes. It’s important to tailor treatment to each patient and adjust it as needed.
The Role of Anti-Thymocyte Globulin and Other Agents
Anti-thymocyte globulin (ATG) is key in GVHD treatment. ATG reduces T-cells, which are central to the immune response and GVHD. Studies show that ATG can improve survival and reduce GVHD severity in some patients.
“The incorporation of ATG into GVHD treatment protocols has been a significant advancement, giving new hope to patients with severe or refractory disease.”
Other drugs, like rituximab and sirolimus, may also be used in GVHD treatment. The choice depends on the patient’s condition and any comorbidities.
Lung Transplantation and 5-Year Survival Rates
For severe GVHD lung disease, lung transplantation might be considered. This major surgery carries risks but can offer a chance of long-term survival for selected patients.
| Treatment Outcome | 1-Year Survival | 5-Year Survival |
|---|---|---|
| Lung Transplantation | 70% | 40% |
| Standard Therapy | 60% | 30% |
The table shows lung transplantation can improve survival rates for advanced GVHD lung disease. Yet, the 5-year survival rate is a challenge. Deciding on lung transplantation must consider the patient’s health, GVHD severity, and other factors.
Fact 7: Long-Term Outcomes of Graft Versus Host Disease Lung
It’s important to know about the long-term effects of graft versus host disease lung. This knowledge helps both patients and doctors. The outcome depends on how severe the disease is, how well it responds to treatment, and the patient’s overall health.
Graft versus host disease lung can affect people in different ways. It can change their quality of life and how long they live. Because of this, finding the right treatment for each person is key.
Post-Transplant Survival Rates Up to 80%
Research shows that some patients with GVHD can live up to 80% of the time after a transplant. Early detection, the right treatment, and the patient’s health are important for this survival rate. We stress the need for full care to achieve these results.
Factors Influencing Prognosis and Recovery
Many things can affect how well a patient with graft versus host disease lung does. These include:
- The severity of GVHD at diagnosis
- Response to initial treatment
- Presence of comorbidities
- The effectiveness of supportive care measures
Every patient’s experience with GVHD lung is different. Recovery depends on many factors. By focusing on individual care and using new treatments, we can help patients live better lives.
As we learn more about pulmonary GVHD, we can better manage its long-term effects. This helps improve the lives of those affected.
Conclusion: Advancing Our Understanding of Pulmonary GVHD
Pulmonary GVHD is a complex condition that affects patients differently. It needs a detailed approach to manage well. This is key to improving patient outcomes and quality of life.
Understanding pulmonary GVHD is vital. We need more research on its causes, diagnosis, and treatment. This will help us create better treatments and care for patients.
Dealing with GVHD requires a team effort. Hematologists, pulmonologists, and others must work together. This teamwork helps in better diagnosing, treating, and managing pulmonary GVHD, leading to better patient care.
As we learn more about pulmonary GVHD, we’re dedicated to top-notch healthcare for all patients. Our aim is to lead in managing lung GVHD and provide the best care with compassion.
FAQ
What is graft versus host disease lung?
Graft versus host disease (GVHD) lung happens in some patients after a stem cell transplant. The immune cells from the donor attack the lung tissue of the recipient.
What are the symptoms of pulmonary GVHD?
Symptoms of pulmonary GVHD include shortness of breath, cough, and trouble breathing. It can also lead to bronchiolitis obliterans syndrome (BOS), causing scarring and narrowing of the airways.
How is pulmonary GVHD diagnosed?
Diagnosing pulmonary GVHD is tough. It involves pulmonary function tests, imaging studies, and sometimes lung biopsy. This helps assess lung damage and rule out other conditions.
What is the difference between acute and chronic pulmonary GVHD?
Acute pulmonary GVHD happens soon after transplant with a strong immune response. Chronic GVHD develops later and can cause long-term lung damage and BOS.
What are the treatment options for GVHD lung?
Treatment for GVHD lung depends on its severity and type. Options include immunosuppressive medications, anti-thymocyte globulin, and lung transplantation in severe cases.
Can GVHD lung be managed or prevented?
GVHD lung can’t always be prevented, but early detection and management help. Monitoring for signs, using immunosuppressive therapy, and addressing lung complications promptly are key.
What is the prognosis for patients with GVHD lung?
The prognosis for GVHD lung patients varies. It depends on the condition’s severity, treatment response, and other complications. Chronic GVHD can significantly affect quality of life and survival.
How does bronchiolitis obliterans syndrome (BOS) affect patients with chronic GVHD?
BOS is a serious complication of chronic GVHD. It causes significant lung damage, impairs lung function, and affects quality of life. Early detection and treatment are essential to slow disease progression.
What are the risk factors for developing pulmonary GVHD?
Risk factors for pulmonary GVHD include donor-recipient HLA mismatch, patient age, and GVHD in other organs. Understanding these can help manage and potentially reduce GVHD incidence.
Is lung transplantation an option for patients with advanced GVHD lung?
Lung transplantation is an option for patients with advanced GVHD lung who haven’t responded to other treatments. The decision involves careful evaluation of the patient’s health and the chance for a successful outcome.
References
PubMed (NCBI): Acute Graft-Versus-Host Disease Prophylaxis and Treatment
Frontiers in Transplantation: Predictive Biomarkers and Strategies for Diagnosing Chronic Graft-Versus-Host Disease
NCBI Bookshelf: Graft-Versus-Host Disease (StatPearls)
Clinical Hematology International (Scholastica HQ): Pulmonary GVHD: Is It Time to Change the NIH Diagnostic Criteria?